TO THE EDITOR:
SARS-CoV-2 causes more severe COVID-19 disease in patients with hematologic diseases than in healthy individuals.1-4 Reportedly, the acquisition of antibodies after SARS-CoV-2 vaccination in these patients is also inferior to that in healthy individuals.5-12 In particular, patients with B-cell malignancies who have been treated with anti-CD20 antibody therapeutics or Bruton’s tyrosine kinase inhibitors present much lower anti-SARS-CoV-2 antibody levels after vaccination, and the rate of antibody acquisition correlates inversely with the interval between discontinuation of the drugs and vaccination.8,11,12 However, there is still limited information about the conditions under which such patients may acquire antibodies after vaccination. In this study, we conducted a prospective observation study (registered on the University Hospital Medical Information Network [UMIN] as #000045150) to evaluate antibody titers achieved after SARS-CoV-2 vaccination in patients with hematological diseases, focusing on peripheral blood lymphocyte subsets and γ-globulin levels, to evaluate the response and search for markers that predict the response.
This study included patients with hematological diseases (n = 263) and healthy volunteers (n = 41) who were vaccinated with messenger RNA vaccines (BNT162b2, mRNA-1273) from May through July 2021 at Fujita Health University and 3 affiliated hospitals (supplemental Methods; supplemental Tables 1-3). The primary end point was the concentration of anti-SARS-CoV-2 receptor-binding domain of spike protein subunit 1 conjugated IgG antibody 14 to 28 days after administration of the second vaccine dose.13 Secondary end points included the association between the acquired antibody titer and diagnosis of hematological diseases, treatment strategy, duration from the last treatment, blood cell counts, including lymphocyte subset at the time of vaccination, and serum immunoglobulin levels. Because the lowest antibody titer obtained after the second dose in healthy subjects (n = 41) was 21.3 U/mL in this cohort, and all but one of the healthy volunteers in a previous study (n = 219) at Fujita Health University showed an antibody titer of 20 U/mL or higher (manuscript submitted by Fujigaki et al),14 an antibody titer of 20 U/mL or higher was used as the cutoff to define a positive antibody response after vaccination in this study. The protocol for the experimental use of patient samples was approved by the institutional review board of Fujita Health University (HM21-067 and HM21-179). Blood samples were harvested after obtaining appropriate informed consent from all the participants. The study was conducted in accordance with the Declaration of Helsinki.
BNT162b2 was administered to 74.1% of the patient group and 100% of the healthy group. The percentage of positive results was significantly lower in the hematological disease group than in the healthy group (52.5% vs 100%; P < .001), and antibody titers acquired after vaccination were also significantly lower (median; 23.8 vs 105.6 U/mL; P < .001; supplemental Table 1). The results of age- and gender-matched analysis were similar (58.7% vs 100%; P < .001). In a comparison of patient groups with lymphoproliferative disorders (lymphoid; n = 176), myeloproliferative disorders (myeloid; n = 49), and benign hematological diseases (benign; n = 38), antibody titers were significantly lower in the collective disease group than in the healthy group (n = 41), as reported previously (supplemental Figure 1).
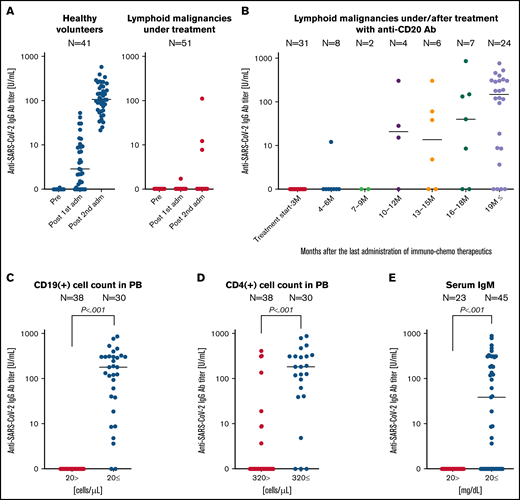
We then further analyzed the lymphoid group, which had a particularly lower antibody acquisition rate after vaccination than other groups. In patients with lymphoid malignancies (47 with B-cell lymphoid [BCL] malignancies and 4 with T-cell lymphoid malignancies) undergoing immunotherapy and/or chemotherapy (under treatment or within 3 months after the last administration of therapeutics), a positive antibody titer was not observed in any of the cases, except for 1 patient with T-cell lymphoma (Figure 1A; supplemental Table 2). Next, we examined the relationship between duration since the last administration and acquired antibody titers in patients with BCL who received anti-CD20 antibody therapeutics (n = 82; Figure 1B). Patients who were within 10 months of the last dose of anti-CD20 antibody therapeutics tended to have more difficulty in acquiring antibodies than those with an interval of more than 10 months, which was consistent with previous reports.8,11 In addition, in our cohort, 37.8% of the patients beyond 12 months after antibody treatment (n = 37) did not mount an antibody response after vaccination (Figure 1B). Based on these results, the factors involved in antibody response after vaccination among patients treated with anti-CD20 antibodies were examined in detail, focusing on blood cell counts, including lymphocyte subsets, and globulin levels at the time of vaccination (supplemental Figure 2; supplemental Table 4). The results showed that the number of CD19+ and CD4+ cells in the peripheral blood and serum IgM titer correlated significantly with the acquired antibody titer. These trends were also seen in patients with hematologic diseases overall, but were particularly pronounced in patients treated with anti-CD20 antibody therapeutics (supplemental Table 4). Using receiver operating characteristic analyses, we calculated the cutoff values as a CD19+ cell count of 20 cells per microliter, CD4+ cell count of 320 cells per microliter, and serum IgM level of 20 mg/dL (supplemental Figure 3). With these criteria, CD19-positive cell counts in peripheral blood showed the strongest correlation with increased anti-SARS-CoV-2 IgG titers (r = 0.844; P < .001), with 0% antibody gain at a titer of <20 per microliter and 76.7% gain at >20 per microliter (Figure 1C). In addition, CD4+ cell counts of more than 320 cells per microliter and IgM levels of more than 20 mg/dL also significantly correlated with increased antibody titers (Figure 1D-E, supplemental Figure 4), although the correlation coefficient was lower than that of CD19+ cell count.
Acquisition of anti-SARS-CoV-2 IgG after vaccination in patients with malignant lymphoma. (A) Anti-SARS-CoV-2 IgG titers increased after the first and second vaccine doses in healthy volunteers (blue dots) and patients in treatment for malignant lymphoma (red dots). Patients in treatment were defined as those receiving treatment at the time of the first dose or within 3 months after the last dose of medication. (B) Differences in antibody titers after the second dose in patients with B-cell malignancies who were in treatment regimens including anti-CD20 antibody therapeutics. IgG titers after the second dose in the same group with appropriate laboratory data were stratified according to the respective cutoff values of prevaccination peripheral blood CD19+ cell count (20 cells per microliter) (C), peripheral blood CD4+cell count (320 cells per microliter μL) (D), and serum IgM level (20 mg/dL) (E), respectively. The cutoff values were calculated by analysis of the receiver operating characteristic curve shown in supplemental Figure 3. pre, before vaccination; adm, administration; treatment start-3M, patients under therapy or up to 3 months after completion of the treatment regimen.
Acquisition of anti-SARS-CoV-2 IgG after vaccination in patients with malignant lymphoma. (A) Anti-SARS-CoV-2 IgG titers increased after the first and second vaccine doses in healthy volunteers (blue dots) and patients in treatment for malignant lymphoma (red dots). Patients in treatment were defined as those receiving treatment at the time of the first dose or within 3 months after the last dose of medication. (B) Differences in antibody titers after the second dose in patients with B-cell malignancies who were in treatment regimens including anti-CD20 antibody therapeutics. IgG titers after the second dose in the same group with appropriate laboratory data were stratified according to the respective cutoff values of prevaccination peripheral blood CD19+ cell count (20 cells per microliter) (C), peripheral blood CD4+cell count (320 cells per microliter μL) (D), and serum IgM level (20 mg/dL) (E), respectively. The cutoff values were calculated by analysis of the receiver operating characteristic curve shown in supplemental Figure 3. pre, before vaccination; adm, administration; treatment start-3M, patients under therapy or up to 3 months after completion of the treatment regimen.
Finally, the same analyses were performed, focusing only on patients in whom BNT162b2 was used to check whether the results were biased by the type of vaccine used. Similar results were obtained for antibody acquisition after vaccination in each hematological disease, and for the relationship between peripheral blood CD19+ and CD4+ cell counts and serum IgM levels and antibody acquisition in patients treated with the anti-CD20 antibody (supplemental Figure 5).
At present, there is no clear evidence suggesting the optimal timing of vaccination in patients with hematologic malignancies during or after chemoimmunotherapy. In particular, patients after the use of anti-CD20 antibody therapeutics are much less likely to benefit from vaccination than other patients, a finding that emphasizes the need for an objective marker that can guide vaccination practice in this special population. Our analysis suggests that the number of CD19+cells in peripheral blood may be a useful marker to predict the likelihood of an antibody response to SARS-CoV-2 vaccination in patients with hematological diseases. Furthermore, serum IgM levels may be useful as an alternative indicator in cases where subset analysis is difficult. One finding of this study that requires attention is that some patients who did not show low levels of CD19, CD4, or IgM also failed to acquire sufficient antibody titers after vaccination (supplemental Figures 2 and 4). Although lymphocyte function and/or other related mechanisms are thought to be important for antibody acquisition, we did not analyze these functions in individual cases in this study, and the question of their role in acquiring antibodies provides an issue for further study.
Our findings showed that the antibody response to SARS-CoV-2 vaccination is grossly suboptimal in patients with hematological disorders, especially in patients with BCL who are undergoing treatment. Alternative preventive strategies, such as proactive vaccination of the patient’s family and surrounding supporters and, in the event of close contact with an infected person, prophylactic administration of monoclonal antibodies or antivirals should be considered to protect patients receiving anti-CD20 antibody therapeutics.
Acknowledgments: The authors thank Yohei Doi (Fujita Health University) for critical review of the manuscript, Takuma Ishihara (Gifu University Hospital) for suggestions regarding the statistical analyses, and Sayoko Ogata and Saori Takagi for laboratory work.
Contribution: A.O., A.T., H.F., K.S., C.I., N.G., H.Y., and M.O. designed the study; A.T., A.O., C.I., N.G., H.Y., M.O., K. Mihara, Y.I., Y. Miura, K.F., Y.Y., Y.A., S.K., K. Miyao, and M.T. collected patient blood samples; A.T., A.O., C.I., N.G., H.Y., M.O., K. Mihara, Y.I., Y. Miura, K.F., Y.Y., Y.A., S.K., K. Miyao, K.H., S.I., and R.K. collected clinical data; H.F. and K.S. performed measurement of anti-SARS-CoV-2 antibody titers; S.S., Y. Mizutani, and M.O. performed lymphocyte subset analysis; A.O. performed statistical analysis; A.O. and A.T. generated figures and tables; A.O., A.T., C.I., and N.G. wrote the paper; and all authors participated in discussions and interpretation of the data and results.
Conflict-of-interest disclosure: K. Mihara has received research funding from Takara Bio and lecture fees from Janssen Pharmaceutical, Sanofi, and CSL Behring. Y.A. has received honoraria from Celgene, Takeda Pharmaceutical, Kyowa Kirin, Teijin Pharma, Novartis Japan, Astra Zeneca, Sanofi, Shire Japan, Chugai Pharmaceutical, Janssen Pharmaceutical, and Bristol Myers Squibb; has served in as an advisor to Takeda Bio; and has received research funding from SRL and Bristol Myers Squibb. K. Miyao has received lecture fees from Novartis Japan, Kyowa Kirin, Nippon Shinyaku, Takeda Pharmaceutical, Eisai, Janssen Pharmaceutical, Bristol Myers Squibb, Celgene, Ono Pharmaceutical, and Otsuka Pharmaceutical. K.S. belongs to an endowed department sponsored by FUJIFILIM Wako Pure Chemical Corporation. A.T. has received research funding from Chugai Pharmaceutical, Astellas Pharma, Eisai, Otsuka Pharmaceutical, Ono Pharmaceutical, Kyowa Kirin, Shionogi, Sumitomo Dainippon Pharma, Taiho Pharmaceutical, Takeda Pharmaceutical, Teijin, Nippon Shinyaku, Nihon Pharmaceutical, Pfizer Japan, Mochida Pharmaceutical, Yakult Honsha, and Perseus Proteomics; and lecture fees from Chugai Pharmaceutical, Kyowa Kirin, Eisai, Takeda Pharmaceutical, Astellas Pharma, Nippon Shinyaku, Janssen Pharmaceutical, Zenyaku Kogyo, AbbVie GK, Bristol Myers Squibb, and SymBio Pharmaceutical.
Correspondence: Akihiro Tomita, Department of Hematology, Fujita Health University School of Medicine, 1-98 Dengakugakubo, Kutsukake-cho, Toyoake, Aichi 470-1192, Japan; e-mail: atomita@fujita-hu.ac.jp
References
Author notes
The full-text version of this article contains a data supplement.