Key Points
The findings of these reviews support VWF multimer analysis or VWF:CB/VWF:Ag to diagnose type 2 VWD.
The reviews confirm that desmopressin trial is the test of choice to confirm increased VWF clearance in patients with suspected VWD type 1C.
Abstract
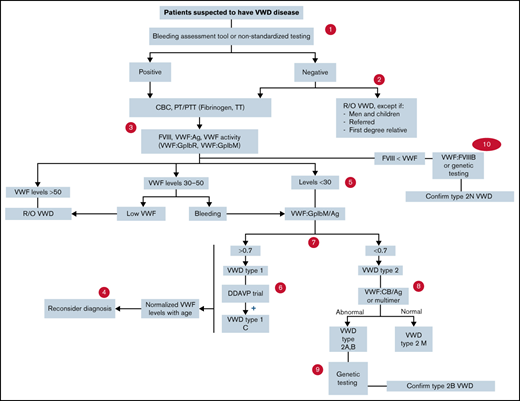
von Willebrand Disease (VWD) is associated with significant morbidity because of excessive bleeding. Early diagnosis and treatment are important to prevent and treat these symptoms. We systematically reviewed the accuracy of any von Willebrand factor (VWF) activity assay in the diagnosis and classification of patients for VWD. We searched Cochrane Central, MEDLINE, and EMBASE for eligible studies. The risk of bias was assessed using the Quality Assessment of Diagnostic Accuracy Studies (QUADAS)-2 and the certainty of evidence using the GRADE framework. We pooled estimates of sensitivity and specificity. The review included 77 studies that evaluated the use of newer tests of VWF platelet binding activity (VWF:GPIbR, VWF:GPIbM) and VWF:RCo for the diagnosis of VWD (13 studies), VWF propeptide to VWF:Ag ratio, and desmopressin trial for the diagnosis of type 1C VWD (5 studies), VWF multimer analysis and VWF:CB/VWF:Ag ratio for the classification of type 2 VWD (11 studies), genetic testing and ristocetin-induced platelet aggregation to diagnose type 2B VWD (14 studies), genetic testing and FVIII:VWF binding to diagnose type 2N VWD (17 studies). Based on available diagnostic test accuracy, there appear to be comparable test accuracy results between newer tests of platelet binding activity of VWF function and VWF:RCo. The findings of these reviews support VWF multimer analysis or VWF:CB/VWF:Ag to diagnose type 2 VWD. The desmopressin trial test with 1- and 4-hour postinfusion blood work is the test of choice to confirm increased VWF clearance in patients with suspected VWD type 1C. Additionally, genetic testing is most useful in diagnosing type 2B VWD and has a role in the diagnostic algorithm of suspected type 2N VWD.
Background
von Willebrand factor (VWF) is a hemostatic protein that binds and stabilizes coagulation factor VIII (FVIII) as well as facilitates platelet adhesion and aggregation at sites of vascular injury.1-4 Qualitative or quantitative abnormalities in VWF lead to von Willebrand disease (VWD).5 The reported prevalence of VWD is up to 1% in the general population based on epidemiologic studies, with the symptomatic prevalence of ∼0.1% at the level of primary care.6-9 This prevalence is ∼15% in women with chronic heavy menstrual bleeding.10,11
Patients with VWD may experience bruising, epistaxis, and oral cavity bleeding, as well as heavy menstrual bleeding and bleeding after dental work, surgical procedures, and childbirth. There is significant heterogeneity in symptoms among patients with VWD, and an individual patient's bleeding phenotype may vary throughout the course of life, leading to the need for individualized management plans depending on the type and subtype of VWD.12,13 Three types of VWD have been defined depending on the type of abnormality in VWF. Type 1 VWD is the result of a partial quantitative deficiency in VWF, whereas patients with type 3 VWD have a virtual absence of VWF. Patients with type 2 VWD have qualitative abnormalities of VWF (types 2A, 2B, 2M, and 2N): type 2A is characterized by a reduction in or complete absence of the most hemostatically active high molecular weight VWF multimers; type 2B is due to a gain of function in VWF that increases its affinity for platelets; type 2M is caused by reduced VWF interactions with platelets or collagen; and type 2N results from reduced binding of VWF to FVIII.4,7,10
The accurate diagnosis and classification of VWD are complex, requiring a correlation between clinical findings and laboratory results.14 Recommended initial laboratory tests include measurements of plasma VWF antigen (VWF:Ag), VWF-platelet GP Ib binding activity (eg, VWF:RCo), and FVIII:C.15,16 Automated methods to measure VWF activity are becoming more widely available and have advantages and limitations.17,18 Additionally, shortened VWF survival has been suggested as a mechanism for the laboratory abnormalities and clinical phenotype observed in some patients. Increased VWF clearance from the plasma was first described in type Vicenza VWD, and shortened VWF survival has also been reported in type 1 VWD.19,20 Haberichter et al showed that a shorter VWF survival could be predicted from the ratio of VWF propeptide (VWFpp) to VWF:Ag concentrations in the plasma.21
In addition to variation in the diagnosis and management of VWD, there is limited awareness within the VWD community on the best clinical practice.22 The aim of this systematic review is to determine the accuracy of commonly available diagnostic tests for VWD, which can be used to inform a combined strategy for diagnosis. The results were used to inform evidence-based recommendations on diagnostic strategies for the recently published clinical practice guidelines on VWD, developed by a combined effort from the American Society of Hematology (ASH), the International Society on Thrombosis and Haemostasis (ISTH), the National Hemophilia Foundation (NHF), the World Federation of Hemophilia (WFH), and the University of Kansas Medical Center.23,24 These guidelines aim to inform all stakeholders on essential issues where there is variation or uncertainty in clinical practice and will support decision-making in the context of the values and preferences of patients.
Methods
Search strategy and data sources
We searched MEDLINE, EMBASE, and the Cochrane Central Register of Controlled Trials (CENTRAL) from inception until August 2019. We also manually searched the reference lists of relevant articles and existing reviews. We limited the search to studies reporting data for the accuracy of diagnostic tests. The complete search strategy is available in supplement 1. The prespecified protocol for this review is registered with PROSPERO (CRD42020147977). This review is reported in accordance with Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) for diagnostic test accuracy guidelines.25
PICO questions
In this systematic review, we addressed the following 5 Population Intervention Comparison Outcome questions:
- 1.
In patients suspected of VWD, should we use VWF:RCo (automated and nonautomated assays) or use newer assays that reflect the platelet binding activity of VWF function (ie: VWF:G1bM, VWF:GP1bR)?
- 2.
In patients suspected of type 1 VWD with increased VWF clearance (eg, type 1C), should we use ratio of VWF propeptide to VWF antigen (VWFpp/VWF:Ag) or use desmopressin trial with 1- and 4-hour bloodwork?
- 3.
In patients suspected of type 2A, 2B, or 2M VWD in need of additional testing, should we use VWF multimer analysis or use VWF collagen binding (VWF:CB) to VWF antigen ratio (VWF:CB/VWF:Ag)?
- 4.
In patients suspected of type 2B VWD, should we use ristocetin-induced platelet aggregation/agglutination (RIPA) or use genetic testing (mutation analysis)?
- 5.
In patients suspected of type 2N in need of additional testing, should we use VWF Factor VIII binding (VWF:FVIII binding) or use genetic testing (mutation analysis)?
Study selection
Studies.
Studies reporting data on diagnostic test accuracy (cohort studies, cross-sectional studies) for VWD were eligible for inclusion in this systematic review.
Participants.
Patients of any age with VWD presenting to inpatient or outpatient setting with suspected VWD were eligible for inclusion.
Index tests for diagnosis.
All of the following tests were considered in eligible studies: VWF:RCo, newer tests of platelet-binding activity of VWF function (VWF:GPIbR, VWF:GPIbM), VWFpp to VWF:Ag ratio, desmopressin trial, VWF multimer analysis and VWF collagen binding (VWF:CB) to VWF:Ag ratio, genetic testing, RIPA, and FVIII:VWF binding. We did not exclude studies based on the timeframe when the index test was conducted.
Reference standards.
If a reference diagnostic test was not conducted, clinical follow-up for symptoms alone was sufficient as a reference standard.
Exclusion criteria.
While studies reporting on patients with VWD as well as other bleeding disorders were eligible for inclusion, we excluded studies in which >80% of the study sample was represented by a different bleeding disorder. When possible, we extracted data separately for patients with VWD from these studies. We also excluded studies that did not provide sufficient data to determine test accuracy (sensitivity and specificity), abstracts, and studies with a sample size of <10 patients.
Screening and data extraction
Independent reviewers conducted title and abstract screening and full-text review in duplicate to identify eligible studies. Data extraction was also conducted independently and in duplicate and verified by a third author (M.A.K.). Disagreements were resolved by discussion to reach a consensus in consultation with 2 expert clinician scientists (N.C. and P.J.). Data extracted included general study characteristics (authors, publication year, country, study design), diagnostic index test and reference standard, the prevalence of VWD, and parameters to determine test accuracy (ie, sensitivity and specificity of the index test).
Risk of bias and certainty of evidence
We conducted the risk of bias assessment for diagnostic test accuracy studies using the Quality Assessment of Diagnostic Accuracy Studies (QUADAS)-2 revised tool.26 The Grading of Recommendations Assessment, Development and Evaluation (GRADE) framework was used to assess overall certainty by evaluating the evidence for each outcome on the following domains: risk of bias, imprecision, inconsistency, indirectness, and publication bias.27,28
Data synthesis
The accuracy estimates from individual studies were combined quantitatively (pooled) for each test using OpenMetaAnalyst. We conducted a bivariate analysis for pooling sensitivity and specificity for each of the test comparisons to account for variation within and between studies. Forest plots were created for each comparison. The Breslow-Day test was used to measure the percentage of total variation across studies due to heterogeneity (I2); however, the results did not influence our judgment of the pooled estimates as the literature has discouraged its use for test accuracy.29
It is important to note that diagnostic strategies for VWD are based on an assessment of the pretest probability of an individual patient, which provides an estimate of the expected prevalence of VWD at a population level. We calculated the absolute differences in effects for each comparison as true positives, true negatives, false positives, and false negatives. Here, we present the results for the low, intermediate, and high pretest probability groups.
Results
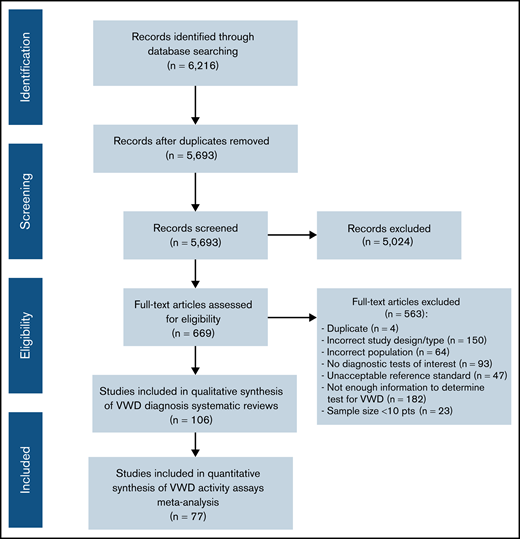
Description of studies
The initial search retrieved 5693 nonduplicate studies, of which 669 were included for full-text review. Following full-text review, 106 were found to be eligible for data abstraction, and 77 answered the question addressed in the systematic review and were included. A list of excluded studies is provided in supplement 2. Reasons for exclusion at full-text review were ineligible study design, study population, diagnostic test, sample size <10 patients, unacceptable reference standards, and/or not enough information to determine diagnostic test accuracy for VWD (Figure 1).
Use of newer tests of platelet binding activity of VWF function (VWF:GPIbR, VWF:GPIbM) and VWF:RCo for VWD diagnosis
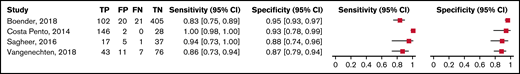
Of the included studies, 13 reported on the use of VWF:GPIbR, VWF:GPIbM, and VWF:RCo in VWD.14,30-41 The different tests used in the 13 studies are reported in supplement 4. The complete risk of bias assessment for individual studies is included in supplement 3. The range of sensitivities for using VWF:RCo was assessed across 4 studies with 337 patients and was 0.83 to 1.00. The range of specificities was assessed across 4 studies with 587 patients and was 0.87 to 0.95 (moderate certainty in the sensitivity results and low certainty in the specificity results). Figure 2 shows the forest plot displaying the sensitivity and specificity from individual studies. Table 1 summarizes the findings for VWF:RCo.
Forest plots for sensitivity and specificity for individual studies assessing VWF:RCo
Forest plots for sensitivity and specificity for individual studies assessing VWF:RCo
GRADE test accuracy evidence summary for VWF:RCo in patients with suspected VWD
| Sensitivity: 0.83-1.00 Specificity: 0.87-0.95 | Prevalences: 3%, 20%, 50% |
| Sensitivity: 0.83-1.00 Specificity: 0.87-0.95 | Prevalences: 3%, 20%, 50% |
| Outcome . | Studies (n); patients (n) . | Study design . | Factors that may decrease certainty of evidence . | Effect per 1000 patients tested . | Test accuracy CoE . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Risk of bias . | Indirectness . | Inconsistency . | Imprecision . | Publication bias . | Pretest probability of 3%* . | Pretest probability of 20%† . | Pretest probability of 50%§ . | ||||
| True positives (patients with VWD) | 4;337 | Cohort & case-control type studies | Serious‡ | Not serious | Not serious | Not serious | None | 25-30 | 166-200 | 415-500 | ⨁⨁⨁◯ MODERATE |
| False negatives (patients incorrectly classified as not having VWD) | 0-5 | 0-34 | 0-85 | ||||||||
| True negatives (patients without VWD) | 4;584 | Cohort & case-control type studies | Serious‡ | Not serious | Not serious | Not serious | None | 844-922 | 696-760 | 435-475 | ⨁⨁◯◯ LOW |
| False positives (patients incorrectly classified as having VWD) | 48-126 | 40-104 | 25-65 | ||||||||
| Outcome . | Studies (n); patients (n) . | Study design . | Factors that may decrease certainty of evidence . | Effect per 1000 patients tested . | Test accuracy CoE . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Risk of bias . | Indirectness . | Inconsistency . | Imprecision . | Publication bias . | Pretest probability of 3%* . | Pretest probability of 20%† . | Pretest probability of 50%§ . | ||||
| True positives (patients with VWD) | 4;337 | Cohort & case-control type studies | Serious‡ | Not serious | Not serious | Not serious | None | 25-30 | 166-200 | 415-500 | ⨁⨁⨁◯ MODERATE |
| False negatives (patients incorrectly classified as not having VWD) | 0-5 | 0-34 | 0-85 | ||||||||
| True negatives (patients without VWD) | 4;584 | Cohort & case-control type studies | Serious‡ | Not serious | Not serious | Not serious | None | 844-922 | 696-760 | 435-475 | ⨁⨁◯◯ LOW |
| False positives (patients incorrectly classified as having VWD) | 48-126 | 40-104 | 25-65 | ||||||||
Typically seen in patients investigated for VWD because of a personal history of bleeding symptoms (eg, mucocutaneous bleeding) (Quiroga, 2007).46
Typically seen in patients investigated for VWD as a first-degree relative of a patient with VWD.
Serious patient selection risk of bias due to case-control design. Also, 3 of the 4 studies (Boender [2018],47 Vangenechten [2018],48 and Sagheer [2016])49 investigated test accuracy for classifying type 2 VWD patients (using a ratio of 0.6), not for diagnosing VWD. The majority of included studies were judged to be low risk of bias for test and reference standard interpretation. Although there was unclear reporting regarding flow and timing in some studies, the certainty of evidence was generally not downgraded for risk of bias. The patient selection risk of bias was moderate/high in all studies.
Typically seen in patients investigated for VWD because of a personal history of abnormal laboratory test (eg, increased Partial Thromboplastin Time (PTT)).
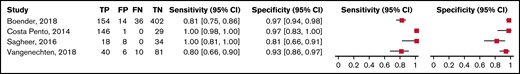
The range of sensitivities for using VWF:GPIbR was assessed across 4 studies with 404 patients and was 0.80 to 1.00. The range of specificities was assessed across 4 studies with 575 patients and was 0.81 to 0.97 (moderate certainty in the sensitivity results and low certainty in the specificity results). Figure 3 shows the forest plot displaying the sensitivity and specificity from individual studies.
Forest plots for sensitivity and specificity for individual studies for VWF:GPIbR
Forest plots for sensitivity and specificity for individual studies for VWF:GPIbR
Overall, the test was shown to be highly sensitive and moderately specific, and the certainty of the evidence was low to moderate. Table 2 shows the summary of findings.
GRADE test accuracy evidence summary for VWF:GPIbR in patients with suspected VWD
| Sensitivity: 0.80-1.00 Specificity: 0.81-0.97 | Prevalences: 3%, 20%, 50% |
| Sensitivity: 0.80-1.00 Specificity: 0.81-0.97 | Prevalences: 3%, 20%, 50% |
| Outcome . | Studies (n); patients (n) . | Study design . | Factors that may decrease certainty of evidence . | Effect per 1000 patients tested . | Test accuracy CoE . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Risk of bias . | Indirectness . | Inconsistency . | Imprecision . | Publication bias . | Pretest probability of 3%* . | Pretest probability of 20%† . | Pretest probability of 50%§ . | ||||
| True positives (patients with VWD) | 4;404 | Cohort & case-control type studies | Serious‡ | Not serious | Not serious | Not serious | None | 24-30 | 160-200 | 400-500 | ⨁⨁⨁◯ MODERATE |
| False negatives (patients incorrectly classified as not having VWD) | 0-6 | 0-40 | 0-100 | ||||||||
| True negatives (patients without VWD) | 4;575 | Cohort & case-control type studies | Serious‡ | Not serious | Not serious | Not serious | None | 786-941 | 648-776 | 405-485 | ⨁⨁◯◯ LOW |
| False positives (patients incorrectly classified as having VWD) | 29-184 | 24-152 | 15-95 | ||||||||
| Outcome . | Studies (n); patients (n) . | Study design . | Factors that may decrease certainty of evidence . | Effect per 1000 patients tested . | Test accuracy CoE . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Risk of bias . | Indirectness . | Inconsistency . | Imprecision . | Publication bias . | Pretest probability of 3%* . | Pretest probability of 20%† . | Pretest probability of 50%§ . | ||||
| True positives (patients with VWD) | 4;404 | Cohort & case-control type studies | Serious‡ | Not serious | Not serious | Not serious | None | 24-30 | 160-200 | 400-500 | ⨁⨁⨁◯ MODERATE |
| False negatives (patients incorrectly classified as not having VWD) | 0-6 | 0-40 | 0-100 | ||||||||
| True negatives (patients without VWD) | 4;575 | Cohort & case-control type studies | Serious‡ | Not serious | Not serious | Not serious | None | 786-941 | 648-776 | 405-485 | ⨁⨁◯◯ LOW |
| False positives (patients incorrectly classified as having VWD) | 29-184 | 24-152 | 15-95 | ||||||||
Typically seen in patients investigated for VWD because of a personal history of bleeding symptoms (eg, mucocutaneous bleeding) (Quiroga, 2007).46
Typically seen in patients investigated for VWD as a first-degree relative of a patient with VWD.
Serious patient selection risk of bias due to case-control design. Also, 3 of the 4 studies (Boender [2018],47 Vangenechten [2018],48 and Sagheer [2016])49 investigated test accuracy for classifying type 2 VWD patients (using a ratio of 0.6), not for diagnosing VWD.
Typically seen in patients investigated for VWD because of a personal history of abnormal laboratory test (eg, increased partial thromboplastin time).
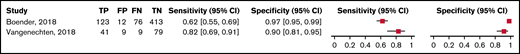
The range of sensitivities for using VWF:GPIbM was assessed across 2 studies with 249 patients and was 0.62 to 0.82. The range of specificities was assessed across 2 studies with 513 patients and was 0.90 to 0.97 (low certainty in the sensitivity and specificity results). Figure 4 shows the forest plot displaying the sensitivity and specificity from individual studies.
Forest plots for sensitivity and specificity for individual studies for VWF:GPIbM
Forest plots for sensitivity and specificity for individual studies for VWF:GPIbM
Overall, the test was shown to be highly sensitive and moderately specific, and the certainty of the evidence was low to moderate. Table 3 shows the summary of findings.
GRADE test accuracy evidence summary for VWF:GPIbM in patients with suspected VWD
| Sensitivity: 0.62-0.82 Specificity: 0.90-0.97 | Prevalences: 3%, 20%, 50% |
| Sensitivity: 0.62-0.82 Specificity: 0.90-0.97 | Prevalences: 3%, 20%, 50% |
| Outcome . | Studies (n); patients (n) . | Study design . | Factors that may decrease certainty of evidence . | Effect per 1000 patients tested . | Test accuracy CoE . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Risk of bias . | Indirectness . | Inconsistency . | Imprecision . | Publication bias . | Pretest probability of 3%* . | Pretest probability of 20%† . | Pretest probability of 50%‡ . | ||||
| True positives (patients with VWD) | 2;249 | Cohort & case-control type studies | Serious§ | Not serious | Not serious | Not serious | None | 19-25 | 124-164 | 310-410 | ⨁⨁◯◯ LOW |
| False negatives (patients incorrectly classified as not having VWD) | 5-11 | 36-76 | 90-190 | ||||||||
| True negatives (patients without VWD) | 2;513 | Cohort & case-control type studies | Serious§ | Not serious | Not serious | Not serious | None | 873-941 | 720-776 | 450-485 | ⨁⨁◯◯ LOW |
| False positives (patients incorrectly classified as having VWD) | 29-97 | 24-80 | 15-50 | ||||||||
| Outcome . | Studies (n); patients (n) . | Study design . | Factors that may decrease certainty of evidence . | Effect per 1000 patients tested . | Test accuracy CoE . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Risk of bias . | Indirectness . | Inconsistency . | Imprecision . | Publication bias . | Pretest probability of 3%* . | Pretest probability of 20%† . | Pretest probability of 50%‡ . | ||||
| True positives (patients with VWD) | 2;249 | Cohort & case-control type studies | Serious§ | Not serious | Not serious | Not serious | None | 19-25 | 124-164 | 310-410 | ⨁⨁◯◯ LOW |
| False negatives (patients incorrectly classified as not having VWD) | 5-11 | 36-76 | 90-190 | ||||||||
| True negatives (patients without VWD) | 2;513 | Cohort & case-control type studies | Serious§ | Not serious | Not serious | Not serious | None | 873-941 | 720-776 | 450-485 | ⨁⨁◯◯ LOW |
| False positives (patients incorrectly classified as having VWD) | 29-97 | 24-80 | 15-50 | ||||||||
Typically seen in patients investigated for VWD because of a personal history of abnormal laboratory test (eg, increased PTT).
Typically seen in patients investigated for VWD because of a personal history of bleeding symptoms (eg, mucocutaneous bleeding) (Quiroga, 2007).46
Typically seen in patients investigated for VWD as a first-degree relative of a patient with VWD.
Serious patient selection risk of bias due to case-control design. Diagnostic test accuracy results for classifying type 2 VWD patients (using a 0.6 ratio), not for diagnosing VWD.
Use of VWF propeptide to VWF:Ag ratio and desmopressin trial for the diagnosis of type 1C VWD
No test accuracy results were presented in the studies due to lack of an agreed-on reference standard to define type 1C VWD; desmopressin trial was used in some papers to determine the increased clearance while the VWFpp to VWF:Ag ratio was used in other papers.
However, an inverse correlation between VWFpp/VWF:Ag and VWF:Ag half-life was shown in 3 studies. The results indicate that the steady-state ratio of plasma VWFpp and VWF can be used to easily identify patients with type 1 VWD with an increased plasma VWF clearance phenotype. Table 4 shows the summary of findings.
Evidence summary for the use of VWF propeptide to VWF:Ag ratio and desmopressin trial for the diagnosis of type 1C VWD
| Outcomes . | Impact . | participants (n, studies) . | Certainty of the evidence (GRADE) . |
|---|---|---|---|
| VWFpp/VWF:Ag ratio correlation with VWF:Ag half-life | In Sztukowska,50 a pronounced drop in VWF survival in the type Vicenza VWD patients was reported: mean half-life significantly shorter than in control groups (1.3 ± 0.2 h, vs 15.4 ± 2.5 h; P < .0001). A dramatic increase in VWFpp ratio in the type Vicenza VWD cases was shown: VWFpp ratio from 7.14 to 17.7, mean 13.02 ± 0.49; 10× higher than in the control group (P < .001).In Haberichter,43 a substantially increased VWFpp/VWF:Ag ratio was predictive of a significantly decreased VWF half-life in 7 individuals who had a >twofold desmopressin response and an initial VWF:Ag <30 IU/dL. Three individuals had a decreased VWF half-life that was not predicted by an increased VWFpp/VWF:Ag ratio. Individuals who had a substantially increased VWFpp/VWF:Ag ratio and significantly reduced VWF:Ag level were also found to have an enhanced response to desmopressin (>fourfold increase). The desmopressin response was found to correlate with the VWFpp/VWF:Ag ratio (r = 0.92; P < .001) | (2 Observational studies) | ⨁◯◯◯ VERY LOW |
| Correlation of the VWFpp/VWF:Ag ratio with the presence or absence of a VWF gene mutation | In Haberichter,21 all affected individuals harbored a VWF gene mutation and showed an increased ratio, whereas no mutation was detected in unaffected individuals. In Eikenboom,44 the increased VWFpp/VWF:Ag ratio was particularly raised (median, 4.3) in patients with slightly abnormal multimers and mutations. An increased VWFpp/VWF:Ag ratio was a good predictor of VWD patients with mutations in the VWF gene: a VWFpp/VWF:Ag >3 had a positive predictive value for the presence of a VWF mutation of 98% with a specificity of 99% in the entire cohort of patients and family members.In Stufano,45 the genetic analysis of the mutation at codon 1205 in the group (n = 14) with the markedly increased VWF clearance distinguished between VWD type 1 Vicenza (characterized by the presence of the mutation p.R1205H) and AVWS (absence of this mutation). | (3 Observational studies) | ⨁⨁◯◯ LOW |
| Outcomes . | Impact . | participants (n, studies) . | Certainty of the evidence (GRADE) . |
|---|---|---|---|
| VWFpp/VWF:Ag ratio correlation with VWF:Ag half-life | In Sztukowska,50 a pronounced drop in VWF survival in the type Vicenza VWD patients was reported: mean half-life significantly shorter than in control groups (1.3 ± 0.2 h, vs 15.4 ± 2.5 h; P < .0001). A dramatic increase in VWFpp ratio in the type Vicenza VWD cases was shown: VWFpp ratio from 7.14 to 17.7, mean 13.02 ± 0.49; 10× higher than in the control group (P < .001).In Haberichter,43 a substantially increased VWFpp/VWF:Ag ratio was predictive of a significantly decreased VWF half-life in 7 individuals who had a >twofold desmopressin response and an initial VWF:Ag <30 IU/dL. Three individuals had a decreased VWF half-life that was not predicted by an increased VWFpp/VWF:Ag ratio. Individuals who had a substantially increased VWFpp/VWF:Ag ratio and significantly reduced VWF:Ag level were also found to have an enhanced response to desmopressin (>fourfold increase). The desmopressin response was found to correlate with the VWFpp/VWF:Ag ratio (r = 0.92; P < .001) | (2 Observational studies) | ⨁◯◯◯ VERY LOW |
| Correlation of the VWFpp/VWF:Ag ratio with the presence or absence of a VWF gene mutation | In Haberichter,21 all affected individuals harbored a VWF gene mutation and showed an increased ratio, whereas no mutation was detected in unaffected individuals. In Eikenboom,44 the increased VWFpp/VWF:Ag ratio was particularly raised (median, 4.3) in patients with slightly abnormal multimers and mutations. An increased VWFpp/VWF:Ag ratio was a good predictor of VWD patients with mutations in the VWF gene: a VWFpp/VWF:Ag >3 had a positive predictive value for the presence of a VWF mutation of 98% with a specificity of 99% in the entire cohort of patients and family members.In Stufano,45 the genetic analysis of the mutation at codon 1205 in the group (n = 14) with the markedly increased VWF clearance distinguished between VWD type 1 Vicenza (characterized by the presence of the mutation p.R1205H) and AVWS (absence of this mutation). | (3 Observational studies) | ⨁⨁◯◯ LOW |
Summary of findings for the use of VWF multimer analysis and VWF:CB/VWF:Ag ratio for the classification of type 2 VWD
| VWF multimer analysis VWF:CB/VWF:Ag Sensitivity: 0.94 (95% CI, 0.90-0.99)/Sensitivity: 0.84 (95% CI, 0.71-0.92) Specificity: 0.97 (95% CI, 0.94-0.99)/Specificity: 0.95 (95% CI, 0.90-0.98) | Prevalences: 80%* |
| VWF multimer analysis VWF:CB/VWF:Ag Sensitivity: 0.94 (95% CI, 0.90-0.99)/Sensitivity: 0.84 (95% CI, 0.71-0.92) Specificity: 0.97 (95% CI, 0.94-0.99)/Specificity: 0.95 (95% CI, 0.90-0.98) | Prevalences: 80%* |
| . | . | . | Factors that may decrease certainty of evidence . | Effect per 1000 patients tested Pretest probability of 80% . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome . | Studies (n); patients (n) . | Study design . | Risk of bias . | Indirectness . | Inconsistency . | Imprecision . | Publication bias . | VWF multimer analysis . | VWF:CB/Ag . | Test accuracy CoE . |
| True positives (patients with VWD type 2) | 9;476 | Cohort & case-control type studies | Very serious† | Not serious | Not serious | Serious‡ | None | 720 (720-792) | 720 (624-768) | ⨁◯◯◯ VERY LOW |
| 0 fewer TP in VWF multimer analysis | ||||||||||
| False negatives (patients incorrectly classified as not having VWD type 2) | 80 (8-80) | 80 (32-176) | ||||||||
| 0 fewer FN in VWF multimer analysis | ||||||||||
| True negatives (patients without VWD type 2) | 9;948 | Cohort & case-control type studies | Very serious† | Not serious | Not serious | Serious‡ | None | 194 (188-198) | 190 (178-196) | ⨁◯◯◯ VERY LOW |
| 4 more TN in VWF multimer analysis | ||||||||||
| False positives (patients incorrectly classified as having VWD type 2) | 6 (2-12) | 10 (4-22) | ||||||||
| 4 fewer FP in VWF multimer analysis | ||||||||||
| . | . | . | Factors that may decrease certainty of evidence . | Effect per 1000 patients tested Pretest probability of 80% . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome . | Studies (n); patients (n) . | Study design . | Risk of bias . | Indirectness . | Inconsistency . | Imprecision . | Publication bias . | VWF multimer analysis . | VWF:CB/Ag . | Test accuracy CoE . |
| True positives (patients with VWD type 2) | 9;476 | Cohort & case-control type studies | Very serious† | Not serious | Not serious | Serious‡ | None | 720 (720-792) | 720 (624-768) | ⨁◯◯◯ VERY LOW |
| 0 fewer TP in VWF multimer analysis | ||||||||||
| False negatives (patients incorrectly classified as not having VWD type 2) | 80 (8-80) | 80 (32-176) | ||||||||
| 0 fewer FN in VWF multimer analysis | ||||||||||
| True negatives (patients without VWD type 2) | 9;948 | Cohort & case-control type studies | Very serious† | Not serious | Not serious | Serious‡ | None | 194 (188-198) | 190 (178-196) | ⨁◯◯◯ VERY LOW |
| 4 more TN in VWF multimer analysis | ||||||||||
| False positives (patients incorrectly classified as having VWD type 2) | 6 (2-12) | 10 (4-22) | ||||||||
| 4 fewer FP in VWF multimer analysis | ||||||||||
Typically seen in patients with VWD type 2 in need for additional testing for subtype classification.
Case-control design makes patient selection bias serious. Different cutoffs were used in the VWF:CB/Ag ratios (0.5 in Popov vs 0.7 in Flood). The majority of included studies were judged to be low risk of bias for test and reference standard interpretation. Although there was unclear reporting regarding flow and timing in some studies, the certainty of evidence was generally not downgraded for risk of bias.
A different clinical decision would be considered if the upper vs lower boundary of the pooled effect estimate was used.
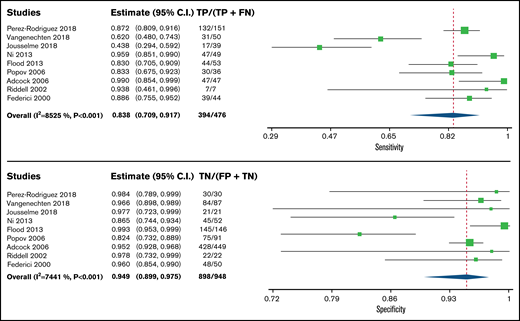
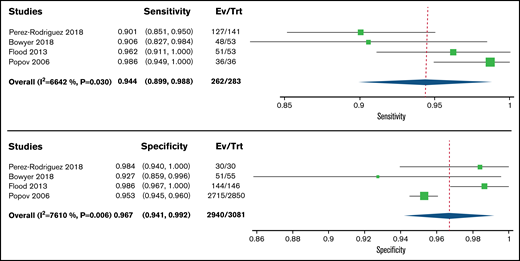
Use of VWF multimer analysis and VWF:CB/Ag ratio for the classification of type 2 VWD
Of the included studies, 11 reported on the use of VWF multimer analysis and VWF:CB/VWF:Ag ratio for the classification of type 2 VWD (Table 5). The complete risk of bias assessment for individual studies is included in supplemental 3.
Test accuracy using VWF multimer analysis and VWF:CB/VWF:Ag ratio was pooled from 9 cohort studies, including 948 participants. Studies used platelet function analyzer, RIPA, VWF:Ag, FVIII:C, VWF:Rco, VWF:GPIbR, VWF:GPIbM, and molecular diagnosis through DNA sequencing as a reference standard for confirming VWD. The pooled estimates for sensitivity and specificity for VWF multimer analysis to diagnose type 2A/B VWD were 0.94 (95% confidence interval [CI], 0.90-0.99) and 0.97 (95% CI, 0.94-0.99), respectively. The pooled estimates for sensitivity and specificity for VWF:CB/VWF:Ag ratio to diagnose type 2A/B VWD were 0.90 (95% CI, 0.78-0.96) and 0.95 (95% CI, 0.89-0.98), respectively (very low certainty in the sensitivity and specificity results). Figures 5 and 6 show the forest plot displaying the sensitivity and specificity from individual studies and the pooled estimates.
Forest plots for sensitivity and specificity for individual studies and the pooled estimated for VWF:CB/VWF:Ag ratio
Forest plots for sensitivity and specificity for individual studies and the pooled estimated for VWF:CB/VWF:Ag ratio
Forest plots for sensitivity and specificity for individual studies and the pooled estimated for multimer analysis
Forest plots for sensitivity and specificity for individual studies and the pooled estimated for multimer analysis
Use of genetic testing and RIPA to diagnose type 2B VWD
The studies reported different RIPA concentrations as the diagnostic threshold. Higher RIPA concentration resulted in higher sensitivity, while lower RIPA concentration led to higher specificity. Genotype was considered to be the reference standard, and correlation was made with RIPA results, providing the sensitivity of RIPA. The methods used in selecting patients led to the difference in the frequency (around 60%, unlike the majority that has 100%). We present the identified mutations across the studies and the correlation results between the 2 tests in supplemental 4.
Use of genetic testing and FVIII:VWF binding to diagnose type 2N VWD
There are no test accuracy results due to the lack of an agreed-on reference standard for type 2N VWD. Supplemental 4 shows genetic variants identified. In all studies, homozygous type 2N VWD patients had binding ratios <0.12, heterozygous carriers had intermediate binding ratios of 0.44 to 0.61, and healthy control subjects had ratios of 0.73 to 1.42 (supplemental 4).
Discussion
This systematic review presents pooled estimates of test accuracy for assays used to diagnose and classify patients with VWD. The certainty of the evidence was very low to moderate.
Based on available diagnostic test accuracy, there appear to be comparable test accuracy results between newer tests of platelet binding activity of VWF function (eg, VWF:GPIbR, VWF:GPIbM) and VWF:RCo. However, there is concern about accuracy in specific populations (eg, in patients with the D1472H polymorphism present in 67% of African American patients and 17% of White patients, who have normal antigen levels, but in whom ristocetin-based assays underestimate VWF activity due to this polymorphism). Borderline levels pose a unique issue given the physiologic change in VWF across the lifespan; however, the studies included patients with a wide range of VWF antigens and activity, minimizing the impact of borderline levels on test accuracy. External quality assessment studies are a great source of knowledge about the real utility of individual VWF assays, as VWF:RCo, VWF:GPIbR, VWF:GPIbM can all lead to false positives and negatives in VWD diagnosis. Additionally, the newer assays overcome the inaccuracy of the levels tested with VWF:RCo when the levels are low, which makes these assays superior to the VWF:RCo assay. To note, data were reviewed for all published methods for VWF:RCo, VWF:GPIbM, VWF:GPIbR, and VWF:Ab; however, consistent with the recommendation of the ISTH and other groups, we focused our deliberations on the first 3 as direct measures of the platelet-binding activity of VWF.
Regarding type 1C VWD, our impression of a diagnostic test is affected by the definition of increased clearance. Generally, this is defined as increased clearance of VWF from the circulation; however, when genetic variants are identified in cases with that phenotype without additional functional characterization, genetic testing becomes a poor reference standard. No test accuracy results were presented in the studies due to the lack of an agreed-on reference standard to define type 1C VWD. Currently, a desmopressin trial is still useful, even if the VWFpp is known, because the response to desmopressin cannot be predicted without that trial.
VWF activity/VWF:Ag can be used to differentiate type 1 VWD from type 2 VWD. As shown by Kalot et al, VWF activity/VWF:Ag ratio of <0.7 vs lower cutoff levels in patients with an abnormal initial VWD screen is more accurate for the diagnosis of type 2 VWD.42 Regarding the use of VWF multimer analysis and VWF:CB/VWF:Ag ratio for the classification of type 2 VWD, the well-correlated results in the multimer analysis evaluations in the different studies are due to the high-quality control standards under which the test was performed, as all were done in laboratories with significant experience in these complex assays. Also, very low VWF antigen levels (<0.15 IU/mL) will lead to unreliable VWF activity assays and ratios. It is important to note that collagen-binding corresponds to more than 1 assay depending on the collagen type: types I and/or III are generally used because type IV is not very sensitive to high molecular weight multimers. Multimer testing allows capturing abnormalities not captured by VWF:CB to allow for further characterization of the disease.
Many genetic variants resulting in type 2B VWD have been identified. In order to perform the analysis, genotype was selected as the gold standard; however, there may be some variants still not properly categorized. It is important to consider patient values when considering genetic testing, as some individuals may be concerned regarding the impact of genetic testing on the determination of parentage (if family testing is performed), along with normal privacy issues around genetic testing, and patients may have fears about what additional testing might be performed without their knowledge. Patients want to know that any stored genetic information is secure and anonymized. However, the targeted nature of genetic testing for type 2B and 2N VWD does help to minimize these concerns.
Patients and clinicians may find it complex to understand the results and clinical utility of genetic testing. Anxiety may result from the knowledge of a mutation that may or may not be clinically significant, and this information can impact other generations who may not give appropriate informed consent during the process of diagnostic genetic testing.
Regarding the diagnosis of type 2N VWD, genetic testing has traditionally been considered the reference standard; however, functional characterization may not have been done for all variants, and in those cases, the phenotype is defined by decreased binding of VWF to FVIII. Genetic testing will help ensure appropriate counseling of patients given that type 2N VWD is autosomal recessive. If only VWF:FVIII binding is performed, the underlying genetic basis will not be known, and genetic counseling may not be inaccurate.
This review has several strengths. The comprehensive and systematic approach for identifying studies makes it unlikely that relevant studies were missed. Additionally, we did not limit our review by language and translated articles that were not published in English. Finally, we assessed the certainty of evidence in this area and identified sources of bias.
We note a few limitations in this comprehensive systematic review. The pooled sensitivity and specificity estimates of the tests from this review only apply when the test is performed alone; however, they can be used to model various diagnostic strategies to inform clinical decision-making. Ultimately, the diagnostic tests will be used in a strategic approach based on clinical pretest probability and with consideration of the availability, cost, and patient and provider values and preferences. Additionally, the overall certainty in the estimates of effect was lowered due to the lack of agreed-on reference standard and possible risk of bias and due to the wide confidence intervals.
Conclusion
This comprehensive systematic review synthesizes and evaluates the accuracy of different assays for the diagnosis and classification of VWD. Estimates of sensitivity and specificity from this review were used to model diagnostic strategies and inform evidence-based recommendations for a clinical practice guideline. Along with sensitivity and specificity estimates, in clinical decision-making, the prevalence or pretest probability of VWD in a population should influence how patients are managed.
Acknowledgments
The authors would like to acknowledge Jenny Castano, members of the American Society of Hematology (ASH), the International Society on Thrombosis and Haemostasis (ISTH), the National Hemophilia Foundation (NHF), the World Federation of Hemophilia (WFH), and the VWD disease diagnosis guidelines panel members for their assistance with data management and organization of the manuscript.
This systematic review was conducted to support the development of the ASH 2021 guidelines for diagnosis and management of VWD. The entire guideline development process was funded by ASH. Through the Outcomes and Implementation Research Unit at the University of Kansas Medical Center, some researchers received a salary or grant support, others participated to fulfill requirements of an academic degree or program or volunteered their time.
Authorship
Contribution: R.A.M., M.A.K., and N.H. contributed to study design, study selection, data extraction, statistical analysis, and interpretation of results; M.A.K., N.H., O.A., O.D., A.E.A., S.T., B.M., A.D., and A.Q. contributed to study selection and data extraction; M.A.K. and R.A.M. contributed to drafting the report; P.J., N.T.C., V.F., R.B.-P., B.A., J.E., N.G., S.H., V.J.-P., B.A.K., S.M., R.M., and J.S.O., contributed to the interpretation of results and critical revision of the report; and all authors approved the final version of the manuscript.
Conflict-of-interest disclosure: P.J. receives research funding from CSL, Behring, Bayer, and Takeda. All other authors declare no competing financial interests.
Correspondence: Reem A. Mustafa, Division of Nephrology and Hypertension, Department of Medicine, University of Kansas Medical Center, Kansas City, Kansas 66160; e-mail: rmustafa@kumc.edu.
References
Author notes
The full-text version of this article contains a data supplement.