Key Points
Women and early-career faculty participation in hematology and oncology board review series is inadequate.
Efforts should be made to ensure adequate participation of women and early-career faculty in hematology and oncology board review series.
Abstract
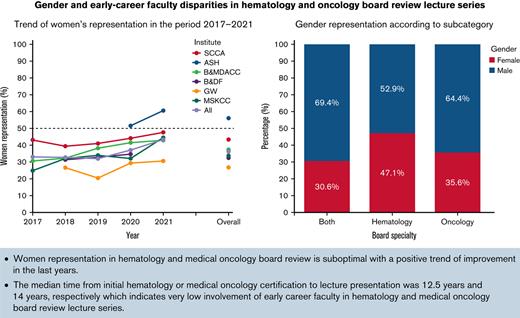
Participation of women and early-career faculty in hematology and medical oncology board review lecture series has not been studied previously. We aimed to evaluate gender and early-career faculty disparities in hematology and medical oncology board review lecture series. Speakers at major hematology and/or oncology board review lecture series meetings in the United States were analyzed in this cross-sectional study during a 5-year period from the years 2017 through 2021. Data about the lecture topic, field, speaker’s gender, years of experience, and the frequency at which the lecture was given by the speaker were collected. Of 386 speakers participating, 315 (81.6%) were ABIM (American Board of Internal Medicine)-certified. A total of 1,224 board review lectures were given in the studied period, of which 1,016 (83%) were given by an ABIM-certified speaker. Women constituted 37.7% of all speakers, with less than 50% representation in five out of six courses. Lectures discussing malignant hematology topics had the lowest proportion of women presenters (24.8%), followed by solid tumors (38.9%) and benign hematology lectures (44.1%). Faculty with more than 15 years since initial certification presented more than 50% of lectures. The median time from initial hematology or medical oncology certification to lecture presentation was 12.5 years and 14 years, respectively. A positive trend in the participation of women was found at all board review conferences across the studied period. Our data suggest that women and early-career faculty participation in hematology and oncology board review series is inadequate.
Introduction
Diversity within the health care workforce has been shown to improve patients’ outcomes.1 Within overall diversity, gender equity in academic and clinical medicine may also produce similar improvements;2 however, disparities are prevalent and hinder progress toward equity. In 2021, only 35.2% of oncologists and 44.6% of oncologists in training in the United States were women.3 Gender disparity has been well-described over the past two decades, with multiple recent efforts to help in closing the gap.4 The representation of women in the medical field is steadily improving; however, women have less access to career development opportunities and leadership positions, which slows the progress of change. Gender transformative measures from medical institutions and societies are necessary.5 A vital pillar that will help in lowering gender inequity is centered on the proper representation of women physicians using a diversity-based panel selection.
Women physicians are also underrepresented in leadership positions in academic oncology.6,7 Underrepresentation of women physicians may contribute to self discomfort and marginalization, thus compromising academic innovation and the quality of patient care.7,8 Being a speaker at academic meetings and conferences is a key factor that helps in achieving promotion, career advancement, leadership opportunities, and improved wages.9,10
Diversity in career stage may result in an overall positive effect on the medical workforce. Early-career faculty members’ involvement as speakers will help advance their careers and may improve retention in academic positions; however, gender disparities in academic conferences are prevalent in multiple medical subspecialties.11-15
A study of 181 major academic medical conferences in the United States and Canada between 2007 and 2017 found that only 15% of the speakers were women physicians.16 Overall rates of early-career faculty presenting at conferences and/or meetings are largely unknown. There is little information about the representation of women in specific education-based meetings, and specifically, the participation of women and early-career faculty speakers in the fields of Hematology and Medical Oncology is not well described. Therefore, we conducted a study to assess the representation trends of women and early-career faculty speakers at major hematology and medical oncology board review lecture series meetings in the United States over a 5-year period.
Materials and Methods
Data sources and extraction
We included all hematology and medical oncology board review lecture series conducted either yearly or every other year. Six board review lecture series from five institutions and one society were included in our study: Baylor College of Medicine/the M.D. Anderson Cancer Center (Baylor&MDA), the Brigham and Dana-Farber (B&DF), George Washington School of Medicine and Health Sciences (GW), Memorial Sloan-Kettering Cancer Center (MSKCC), Seattle Cancer Care Alliance (SCCA), and the hematology board review series from the American Society of Hematology (ASH). All lectures from the years 2017 through 2021 were included. Details of the lectures were obtained via brochures available on the institutions’ official websites, and all available lectures were included in our analysis. Extraction was conducted on variables, including the title of each lecture; speaker’s name, gender, and affiliation; whether the lecture was local or external; if it was related to board certification (hematology, oncology, or both) or for “maintenance of certification” (MOC); the category of the presented lecture (malignant hematology, benign hematology, or solid tumors); and the number of publications per speaker. Data on board certification and MOC were obtained from the American Board of Internal Medicine (ABIM) website. We have excluded members who were assigned to lunch reviews, opening or closing remarks, adjournments, and question-and-answer sessions. Gender was defined as either man or woman and was determined using the full name in addition to biography information or images available on department websites. The study was reported according to EQUATOR (Enhancing the Quality and Transparency of Health Research) guidelines.17 We extracted the number of publications for all speakers in each conference year using the PubMed database.
Statistical analysis
Comparative analyses was performed using t test and ANOVA for continuous variables and χ-square test and Fisher’s exact test for categorical variables. A P < .05 was considered statistically significant. The analyses for this study was performed using R (v.4.1.2) (at the University of Auckland, Auckland, New Zealand) and RStudio (v.1.1.423) (RStudio, Boston, MA). We assumed a 5% type-I error rate for all hypothesis tests (two-sided).18
Results
Our analysis included 1,224 board review lectures. Women presented 37.7% of all the lectures (Table 1). We focused on the largest subset of lectures presented by ABIM-certified speakers (n = 1,016, 83%). Representation of women in lectures varied significantly across the included institutes (28.3% to 57.3%, P < .001), with a representation of less than 50% in five out of six board reviews series. Approximately 50% of the lectures were given by speakers boarded in oncology, 15.3% by speakers boarded in hematology, 32.5% by speakers boarded in both, and 3.6% by speakers with no board certification. Lecture topics included solid tumors (46.4%), malignant hematology (26.2%), benign hematology (24.3%), and other topics (3.1%) (eg, palliative care, pharmacology, and infectious disease).
Characteristics of lectures across different board review lectures
| All specialties . | ASH (N = 75) . | B & MDA (N = 288) . | B & DF (N = 116) . | GW (N = 300) . | MSKCC (N = 199) . | SCCA (N = 246) . | P value . | Overall (N = 1224) . |
|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||
| Women | 43.0 (57.3%) | 109 (37.8%) | 38.0 (32.8%) | 85.0 (28.3%) | 75.0 (37.7%) | 111 (45.1%) | <0.001 | 461 (37.7%) |
| Men | 32.0 (42.7%) | 179 (62.2%) | 78.0 (67.2%) | 215 (71.7%) | 124 (62.3%) | 135 (54.9%) | — | 763 (62.3%) |
| Specialty | ||||||||
| ABIM | 64.0 (85.3%) | 226 (78.5%) | 98.0 (84.5%) | 244 (81.3%) | 179 (89.9%) | 205 (83.3%) | — | 1016 (83.0%) |
| Others | 2.00 (2.7%) | 36.0 (12.5%) | 4.00 (3.4%) | 40.0 (13.3%) | 20.0 (10.1%) | 41.0 (16.7%) | — | 143 (11.7%) |
| Pathology | 1.00 (1.3%) | 15.0 (5.2%) | 6.00 (5.2%) | 12.0 (4.0%) | 0 (0%) | 0 (0%) | — | 34.0 (2.8%) |
| Pediatrics | 8.00 (10.7%) | 11.0 (3.8%) | 8.00 (6.9%) | 4.00 (1.3%) | 0 (0%) | 0 (0%) | — | 31.0 (2.5%) |
| All specialties . | ASH (N = 75) . | B & MDA (N = 288) . | B & DF (N = 116) . | GW (N = 300) . | MSKCC (N = 199) . | SCCA (N = 246) . | P value . | Overall (N = 1224) . |
|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||
| Women | 43.0 (57.3%) | 109 (37.8%) | 38.0 (32.8%) | 85.0 (28.3%) | 75.0 (37.7%) | 111 (45.1%) | <0.001 | 461 (37.7%) |
| Men | 32.0 (42.7%) | 179 (62.2%) | 78.0 (67.2%) | 215 (71.7%) | 124 (62.3%) | 135 (54.9%) | — | 763 (62.3%) |
| Specialty | ||||||||
| ABIM | 64.0 (85.3%) | 226 (78.5%) | 98.0 (84.5%) | 244 (81.3%) | 179 (89.9%) | 205 (83.3%) | — | 1016 (83.0%) |
| Others | 2.00 (2.7%) | 36.0 (12.5%) | 4.00 (3.4%) | 40.0 (13.3%) | 20.0 (10.1%) | 41.0 (16.7%) | — | 143 (11.7%) |
| Pathology | 1.00 (1.3%) | 15.0 (5.2%) | 6.00 (5.2%) | 12.0 (4.0%) | 0 (0%) | 0 (0%) | — | 34.0 (2.8%) |
| Pediatrics | 8.00 (10.7%) | 11.0 (3.8%) | 8.00 (6.9%) | 4.00 (1.3%) | 0 (0%) | 0 (0%) | — | 31.0 (2.5%) |
| ABIM . | ASH (N = 64) . | B & MDA (N = 226) . | B & DF (N = 98) . | GW (N = 244) . | MSKCC (N = 179) . | SCCA (N = 2 05) . | P value . | Overall (N = 1016) . |
|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||
| Women | 36.0 (56.3%) | 80.0 (35.4%) | 34.0 (34.7%) | 66.0 (27.0%) | 64.0 (35.8%) | 89.0 (43.4%) | <0.001 | 369 (36.3%) |
| Men | 28.0 (43.8%) | 146 (64.6%) | 64.0 (65.3%) | 178 (73.0%) | 115 (64.2%) | 116 (56.6%) | — | 647 (63.7%) |
| Certification | ||||||||
| Heme | 19.0 (29.7%) | 28.0 (12.4%) | 12.0 (12.2%) | 52.0 (21.3%) | 21.0 (11.7%) | 23.0 (11.2%) | — | 155 (15.3%) |
| Oncology | 10.0 (15.6%) | 126 (55.8%) | 43.0 (43.9%) | 104 (42.6%) | 119 (66.5%) | 92.0 (44.9%) | — | 494 (48.6%) |
| Both | 32.0 (50.0%) | 66.0 (29.2%) | 36.0 (36.7%) | 79.0 (32.4%) | 39.0 (21.8%) | 78.0 (38.0%) | — | 330 (32.5%) |
| None | 3.00 (4.7%) | 6.00 (2.7%) | 7.00 (7.1%) | 9.00 (3.7%) | 0 (0%) | 12.0 (5.9%) | — | 37.0 (3.6%) |
| Role | ||||||||
| Benign hematology | 35.0 (54.7%) | 49.0 (21.7%) | 20.0 (20.4%) | 86.0 (35.2%) | 19.0 (10.6%) | 38.0 (18.5%) | — | 247 (24.3%) |
| Malignant hematology | 29.0 (45.3%) | 63.0 (27.9%) | 22.0 (22.4%) | 55.0 (22.5%) | 40.0 (22.3%) | 57.0 (27.8%) | — | 266 (26.2%) |
| Solid tumors | 0 (0%) | 114 (50.4%) | 48.0 (49.0%) | 96.0 (39.3%) | 113 (63.1%) | 100 (48.8%) | — | 471 (46.4%) |
| Others | 0 (0%) | 0 (0%) | 8.00 (8.2%) | 7.00 (2.9%) | 7.00 (3.9%) | 10.0 (4.9%) | — | 32.0 (3.1%) |
| ABIM . | ASH (N = 64) . | B & MDA (N = 226) . | B & DF (N = 98) . | GW (N = 244) . | MSKCC (N = 179) . | SCCA (N = 2 05) . | P value . | Overall (N = 1016) . |
|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||
| Women | 36.0 (56.3%) | 80.0 (35.4%) | 34.0 (34.7%) | 66.0 (27.0%) | 64.0 (35.8%) | 89.0 (43.4%) | <0.001 | 369 (36.3%) |
| Men | 28.0 (43.8%) | 146 (64.6%) | 64.0 (65.3%) | 178 (73.0%) | 115 (64.2%) | 116 (56.6%) | — | 647 (63.7%) |
| Certification | ||||||||
| Heme | 19.0 (29.7%) | 28.0 (12.4%) | 12.0 (12.2%) | 52.0 (21.3%) | 21.0 (11.7%) | 23.0 (11.2%) | — | 155 (15.3%) |
| Oncology | 10.0 (15.6%) | 126 (55.8%) | 43.0 (43.9%) | 104 (42.6%) | 119 (66.5%) | 92.0 (44.9%) | — | 494 (48.6%) |
| Both | 32.0 (50.0%) | 66.0 (29.2%) | 36.0 (36.7%) | 79.0 (32.4%) | 39.0 (21.8%) | 78.0 (38.0%) | — | 330 (32.5%) |
| None | 3.00 (4.7%) | 6.00 (2.7%) | 7.00 (7.1%) | 9.00 (3.7%) | 0 (0%) | 12.0 (5.9%) | — | 37.0 (3.6%) |
| Role | ||||||||
| Benign hematology | 35.0 (54.7%) | 49.0 (21.7%) | 20.0 (20.4%) | 86.0 (35.2%) | 19.0 (10.6%) | 38.0 (18.5%) | — | 247 (24.3%) |
| Malignant hematology | 29.0 (45.3%) | 63.0 (27.9%) | 22.0 (22.4%) | 55.0 (22.5%) | 40.0 (22.3%) | 57.0 (27.8%) | — | 266 (26.2%) |
| Solid tumors | 0 (0%) | 114 (50.4%) | 48.0 (49.0%) | 96.0 (39.3%) | 113 (63.1%) | 100 (48.8%) | — | 471 (46.4%) |
| Others | 0 (0%) | 0 (0%) | 8.00 (8.2%) | 7.00 (2.9%) | 7.00 (3.9%) | 10.0 (4.9%) | — | 32.0 (3.1%) |
ABIM, American Board of Internal Medicine; SCCA, Seattle Cancer Care Alliance; ASH, American Society of Hematology; B & MDA, Baylor College of Medicine and M.D. Anderson Cancer Center; B&DF, The Brigham and Dana-Farber; GW, George Washington School of Medicine and Health Sciences; MSKCC, Memorial Sloan-Kettering Cancer Center.
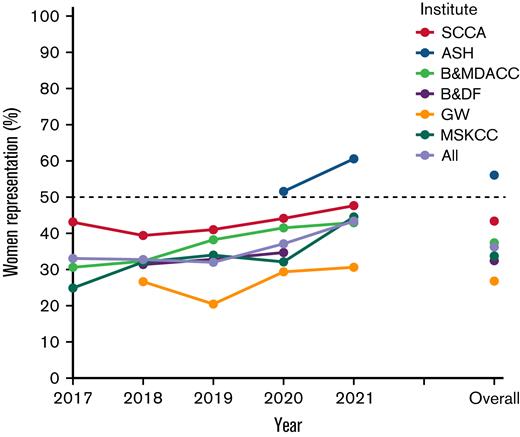
The lectures were presented by 386 speakers, 42.2% of which were women (Table 2). Our sample of interest contained 315 (81.6%) ABIM speakers, 40.3% of which were women. Oncology-boarded speakers constituted 45.1% of the sample. Maintenance of certification was active in 56.1% of the speakers, and this rate did not differ significantly across institutes (P = .33). Most of the speakers at GW were invited speakers from outside institutions, while B&DF, MKSCC, and SCCA hosted primarily local speakers. Baylor&MDA had a balanced distribution between local and invited outside speakers, while the ASH board review course was conducted as a virtual platform in the studied period. The mean number of lectures per speaker during the study period was 3.5 lectures (standard deviation: 3.0). The median number of lectures per speaker was four lectures at GW and Baylor&MDA, three lectures at B&DF, MSKCC, and SCCA, and one lecture at ASH. The median number of publications per speaker was 84, which was not significantly different between institutes (P = .11). The median years since initial certification was 12.5 years in hematology and 14.0 in medical oncology, which varied among different courses (P < .001). GW had the largest median years since initial certification, with 27 in hematology and 24 in medical oncology. Trend analysis showed an increase in representation of women across the studied years in all board reviews, with only ASH achieving more than 50% in their two courses (see Figure 1).
Characteristics of speakers across different board review lectures
| All specialties . | ASH (N = 38) . | B & MDA (N = 70) . | B & DF (N = 58) . | GW (N = 65) . | MSKCC (N = 62) . | SCCA (N = 93) . | P value . | Overall (N=386) . |
|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||
| Women | 24.0 (63.2%) | 30.0 (42.9%) | 20.0 (34.5%) | 21.0 (32.3%) | 25.0 (40.3%) | 43.0 (46.2%) | 0.041 | 163 (42.2%) |
| Men | 14.0 (36.8%) | 40.0 (57.1%) | 38.0 (65.5%) | 44.0 (67.7%) | 37.0 (59.7%) | 50.0 (53.8%) | — | 223 (57.8%) |
| Specialty | ||||||||
| ABIM | 33.0 (86.8%) | 52.0 (74.3%) | 48.0 (82.8%) | 53.0 (81.5%) | 56.0 (90.3%) | 73.0 (78.5%) | — | 315 (81.6%) |
| Pathology | 1.00 (2.6%) | 3.00 (4.3%) | 3.00 (5.2%) | 2.00 (3.1%) | 0 (0%) | 0 (0%) | — | 9.00 (2.3%) |
| Pediatrics | 4.00 (10.5%) | 4.00 (5.7%) | 4.00 (6.9%) | 1.00 (1.5%) | 0 (0%) | 0 (0%) | — | 13.0 (3.4%) |
| Others | 0 (0%) | 11.0 (15.7%) | 3.00 (5.2%) | 9.00 (13.8%) | 6.00 (9.7%) | 20.0 (21.5%) | — | 49.0 (12.7%) |
| All specialties . | ASH (N = 38) . | B & MDA (N = 70) . | B & DF (N = 58) . | GW (N = 65) . | MSKCC (N = 62) . | SCCA (N = 93) . | P value . | Overall (N=386) . |
|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||
| Women | 24.0 (63.2%) | 30.0 (42.9%) | 20.0 (34.5%) | 21.0 (32.3%) | 25.0 (40.3%) | 43.0 (46.2%) | 0.041 | 163 (42.2%) |
| Men | 14.0 (36.8%) | 40.0 (57.1%) | 38.0 (65.5%) | 44.0 (67.7%) | 37.0 (59.7%) | 50.0 (53.8%) | — | 223 (57.8%) |
| Specialty | ||||||||
| ABIM | 33.0 (86.8%) | 52.0 (74.3%) | 48.0 (82.8%) | 53.0 (81.5%) | 56.0 (90.3%) | 73.0 (78.5%) | — | 315 (81.6%) |
| Pathology | 1.00 (2.6%) | 3.00 (4.3%) | 3.00 (5.2%) | 2.00 (3.1%) | 0 (0%) | 0 (0%) | — | 9.00 (2.3%) |
| Pediatrics | 4.00 (10.5%) | 4.00 (5.7%) | 4.00 (6.9%) | 1.00 (1.5%) | 0 (0%) | 0 (0%) | — | 13.0 (3.4%) |
| Others | 0 (0%) | 11.0 (15.7%) | 3.00 (5.2%) | 9.00 (13.8%) | 6.00 (9.7%) | 20.0 (21.5%) | — | 49.0 (12.7%) |
| ABIM . | ASH (N = 33) . | B & MDA (N = 52) . | B & DF (N = 48) . | GW (N = 53) . | MSKCC (N = 56) . | SCCA (N = 73) . | P value . | Overall (N = 315) . |
|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||
| Women | 20.0 (60.6%) | 21.0 (40.4%) | 18.0 (37.5%) | 16.0 (30.2%) | 21.0 (37.5%) | 31.0 (42.5%) | 0.136 | 127 (40.3%) |
| Men | 13.0 (39.4%) | 31.0 (59.6%) | 30.0 (62.5%) | 37.0 (69.8%) | 35.0 (62.5%) | 42.0 (57.5%) | — | 188 (59.7%) |
| Certification | ||||||||
| Hematology | 6.00 (18.2%) | 3.00 (5.8%) | 6.00 (12.5%) | 13.0 (24.5%) | 5.00 (8.9%) | 7.00 (9.6%) | — | 40.0 (12.7%) |
| Oncology | 6.00 (18.2%) | 26.0 (50.0%) | 18.0 (37.5%) | 19.0 (35.8%) | 38.0 (67.9%) | 35.0 (47.9%) | — | 142 (45.1%) |
| Both | 20.0 (60.6%) | 22.0 (42.3%) | 20.0 (41.7%) | 18.0 (34.0%) | 13.0 (23.2%) | 23.0 (31.5%) | — | 116 (36.8%) |
| None | 1.00 (3.0%) | 1.00 (1.9%) | 4.00 (8.3%) | 3.00 (5.7%) | 0 (0%) | 8.00 (11.0%) | — | 17.0 (5.4%) |
| MOC∗ | ||||||||
| Yes | 20.0 (62.5%) | 25.0 (52.1%) | 26.0 (55.3%) | 26.0 (51.0%) | 24.0 (48.0%) | 44.0 (66.7%) | 0.334 | 165 (56.1%) |
| No | 12.0 (37.5%) | 23.0 (47.9%) | 21.0 (44.7%) | 25.0 (49.0%) | 26.0 (52.0%) | 22.0 (33.3%) | — | 129 (43.9%) |
| Location | ||||||||
| External | 33.0 (100%) | 23.0 (44.2%) | 0 (0%) | 49.0 (92.5%) | 0 (0%) | 10.0 (13.7%) | — | 115 (36.5%) |
| Local | 0 (0%) | 29.0 (55.8%) | 48.0 (100%) | 4.00 (7.5%) | 56.0 (100%) | 63.0 (86.3%) | — | 200 (63.5%) |
| Lectures given | ||||||||
| Mean (SD) | 1.30 (0.467) | 3.87 (2.40) | 2.94 (1.81) | 6.08 (4.96) | 3.05 (1.77) | 3.05 (2.15) | <0.001 | 3.50 (2.99) |
| Median [min, max] | 1.00 [1.00, 2.00] | 4.00 [1.00, 10.0] | 3.00 [1.00, 11.0] | 4.00 [1.00, 18.0] | 3.00 [1.00, 7.00] | 3.00 [1.00, 14.0] | — | 3.00 [1.00, 18.0] |
| Hematology experience (y) | ||||||||
| Mean (SD) | 13.9 (9.89) | 14.4 (9.31) | 19.7 (11.6) | 25.2 (13.3) | 16.9 (8.95) | 10.4 (8.93) | <0.001 | 16.9 (11.6) |
| Median [min, max] | 10.0 [4.00, 39.0] | 12.0 [2.00, 38.0] | 17.0 [2.00, 45.0] | 27.0 [2.00, 48.0] | 14.5 [4.00, 30.0] | 9.00 [2.00, 35.0] | — | 12.5 [2.00, 48.0] |
| Missing | 7.00 (21.2%) | 27.0 (51.9%) | 22.0 (45.8%) | 22.0 (41.5%) | 40.0 (71.4%) | 43.0 (58.9%) | — | 161 (51.1%) |
| Oncology experience (y) | ||||||||
| Mean (SD) | 16.6 (12.0) | 16.3 (9.00) | 18.8 (9.81) | 23.4 (10.7) | 16.2 (9.31) | 11.2 (8.63) | <0.001 | 16.6 (10.3) |
| Median [min, max] | 11.5 [4.00, 40.0] | 16.0 [0, 37.0] | 17.0 [2.00, 45.0] | 24.0 [8.00, 44.0] | 16.0 [3.00, 39.0] | 9.00 [2.00, 36.0] | — | 14.0 [0, 45.0] |
| Missing | 7.00 (21.2%) | 4.00 (7.7%) | 10.0 (20.8%) | 16.0 (30.2%) | 7.00 (12.5%) | 15.0 (20.5%) | — | 59.0 (18.7%) |
| ABIM . | ASH (N = 33) . | B & MDA (N = 52) . | B & DF (N = 48) . | GW (N = 53) . | MSKCC (N = 56) . | SCCA (N = 73) . | P value . | Overall (N = 315) . |
|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||
| Women | 20.0 (60.6%) | 21.0 (40.4%) | 18.0 (37.5%) | 16.0 (30.2%) | 21.0 (37.5%) | 31.0 (42.5%) | 0.136 | 127 (40.3%) |
| Men | 13.0 (39.4%) | 31.0 (59.6%) | 30.0 (62.5%) | 37.0 (69.8%) | 35.0 (62.5%) | 42.0 (57.5%) | — | 188 (59.7%) |
| Certification | ||||||||
| Hematology | 6.00 (18.2%) | 3.00 (5.8%) | 6.00 (12.5%) | 13.0 (24.5%) | 5.00 (8.9%) | 7.00 (9.6%) | — | 40.0 (12.7%) |
| Oncology | 6.00 (18.2%) | 26.0 (50.0%) | 18.0 (37.5%) | 19.0 (35.8%) | 38.0 (67.9%) | 35.0 (47.9%) | — | 142 (45.1%) |
| Both | 20.0 (60.6%) | 22.0 (42.3%) | 20.0 (41.7%) | 18.0 (34.0%) | 13.0 (23.2%) | 23.0 (31.5%) | — | 116 (36.8%) |
| None | 1.00 (3.0%) | 1.00 (1.9%) | 4.00 (8.3%) | 3.00 (5.7%) | 0 (0%) | 8.00 (11.0%) | — | 17.0 (5.4%) |
| MOC∗ | ||||||||
| Yes | 20.0 (62.5%) | 25.0 (52.1%) | 26.0 (55.3%) | 26.0 (51.0%) | 24.0 (48.0%) | 44.0 (66.7%) | 0.334 | 165 (56.1%) |
| No | 12.0 (37.5%) | 23.0 (47.9%) | 21.0 (44.7%) | 25.0 (49.0%) | 26.0 (52.0%) | 22.0 (33.3%) | — | 129 (43.9%) |
| Location | ||||||||
| External | 33.0 (100%) | 23.0 (44.2%) | 0 (0%) | 49.0 (92.5%) | 0 (0%) | 10.0 (13.7%) | — | 115 (36.5%) |
| Local | 0 (0%) | 29.0 (55.8%) | 48.0 (100%) | 4.00 (7.5%) | 56.0 (100%) | 63.0 (86.3%) | — | 200 (63.5%) |
| Lectures given | ||||||||
| Mean (SD) | 1.30 (0.467) | 3.87 (2.40) | 2.94 (1.81) | 6.08 (4.96) | 3.05 (1.77) | 3.05 (2.15) | <0.001 | 3.50 (2.99) |
| Median [min, max] | 1.00 [1.00, 2.00] | 4.00 [1.00, 10.0] | 3.00 [1.00, 11.0] | 4.00 [1.00, 18.0] | 3.00 [1.00, 7.00] | 3.00 [1.00, 14.0] | — | 3.00 [1.00, 18.0] |
| Hematology experience (y) | ||||||||
| Mean (SD) | 13.9 (9.89) | 14.4 (9.31) | 19.7 (11.6) | 25.2 (13.3) | 16.9 (8.95) | 10.4 (8.93) | <0.001 | 16.9 (11.6) |
| Median [min, max] | 10.0 [4.00, 39.0] | 12.0 [2.00, 38.0] | 17.0 [2.00, 45.0] | 27.0 [2.00, 48.0] | 14.5 [4.00, 30.0] | 9.00 [2.00, 35.0] | — | 12.5 [2.00, 48.0] |
| Missing | 7.00 (21.2%) | 27.0 (51.9%) | 22.0 (45.8%) | 22.0 (41.5%) | 40.0 (71.4%) | 43.0 (58.9%) | — | 161 (51.1%) |
| Oncology experience (y) | ||||||||
| Mean (SD) | 16.6 (12.0) | 16.3 (9.00) | 18.8 (9.81) | 23.4 (10.7) | 16.2 (9.31) | 11.2 (8.63) | <0.001 | 16.6 (10.3) |
| Median [min, max] | 11.5 [4.00, 40.0] | 16.0 [0, 37.0] | 17.0 [2.00, 45.0] | 24.0 [8.00, 44.0] | 16.0 [3.00, 39.0] | 9.00 [2.00, 36.0] | — | 14.0 [0, 45.0] |
| Missing | 7.00 (21.2%) | 4.00 (7.7%) | 10.0 (20.8%) | 16.0 (30.2%) | 7.00 (12.5%) | 15.0 (20.5%) | — | 59.0 (18.7%) |
ABIM, American Board of Internal Medicine; SCCA, Seattle Cancer Care Alliance; ASH, American Society of Hematology; B & MDA, Baylor College of Medicine and M.D. Anderson Cancer Center; B & DF, The Brigham and Dana-Farber; GW, George Washington School of Medicine and Health Sciences; MOC, maintenance of certification; MSKCC, Memorial Sloan-Kettering Cancer Center; SD, standard deviation.
21 entries are missing.
Trend in the representation of women across different courses. SCCA, Seattle Cancer Care Alliance; ASH, American Society of Hematology; B&MDACC, the Brigham and M.D. Anderson Cancer Center; B&DF, the Brigham and Dana-Farber; GW, George Washington School of Medicine and Health Sciences; MSKCC, Memorial Sloan-Kettering Cancer Center.
Trend in the representation of women across different courses. SCCA, Seattle Cancer Care Alliance; ASH, American Society of Hematology; B&MDACC, the Brigham and M.D. Anderson Cancer Center; B&DF, the Brigham and Dana-Farber; GW, George Washington School of Medicine and Health Sciences; MSKCC, Memorial Sloan-Kettering Cancer Center.
Representation of women was the lowest in malignant hematology lectures (24.8%), followed by solid tumors (38.9%) and benign hematology lectures (44.1%). Women presented 44.2% of the 208 lectures by non-ABIM speakers (including pediatrics, pathology, and others).
Most speakers had >15 years’ experience since initial certification in both lectures presented by hematology- or medical oncology-boarded speakers (54.5% and 55.6%, respectively). Only 5.6% had fewer than 5 years of hematology experience, and 19.3% had between 5 and 10 years of experience; the respective rates for oncology experience were only 4.7% and 20.3%.
We also investigated how frequently the same speaker gave lectures. Thirteen men conducted ≥10 lectures across all the courses, whereas only two women conducted ≥10 lectures across all the courses. The maximum number of lectures given by a speaker was 18 for men and 17 for women. Thirty-five men and 12 women gave ≥6 lectures across all the courses.
Discussion
Our study provides the first analysis of gender and early-career faculty disparities in speakers at hematology and medical oncology board review meetings. We covered six major board reviews over the last 5 years that are either conducted yearly or every other year. The general trend across all meetings showed skewness toward men speakers. The better representation of the ASH hematology review series proves that equal representation between men and women is possible. As for the speakers’ clinical experience in their respective fields (hematology and medical oncology), more than half of the given board review lectures were given by faculty with more than 15 years’ experience since initial certification, which reflects a lack of appropriate involvement of early-career faculty who, arguably, may have more recent experience with board certification.
The proportion of women entering the field of oncology has increased significantly in recent years, and women currently make up approximately 35% of the clinical workforce in the United States.3 Although the percentage of women who present at these conferences should be at least as high as the percentage of women in the general workforce, we believe that a 50:50 women/men representation is more appropriate. According to a 2019 Association of American Medical Colleges report,19 women constituted 45% of hematology/medical oncology trainees. With the growing numbers of women medical students, residents, and fellows, gender disparities may worsen if not addressed promptly.
The incremental increase in the percentage of women presenting in board review series from 2017 through 2021 was observed at all institutes and is encouraging, although only one board review course was more than half women.
We found that representation of women was the lowest in malignant hematology lectures, followed by solid tumors and benign hematology lectures. This important finding may help in focusing efforts to target malignant hematology women representation. One example that can help in this initiative is the Women in Hematology Working Group, a dedicated group of ASH members, with multiple efforts to strengthen the visibility of and recognition for the contributions of women hematologists.
The lack of women presenting at oncological conferences is not limited to oncology conferences, as it does exist in other fields such as otolaryngology conferences, head and neck meetings,20 radiation oncology,21 emergency medicine,15 and research conferences.22 A plethora of factors were found to affect the decision of women oncologists to leave academia, which worsens gender inequality. These factors include difficulty combining job and family responsibilities, frustrations with research, a biased institutional environment,23 and encountering unwanted sexual comments at work.24 Additionally, women are less likely to be promoted to the rank of associate or full professor or to be appointed to department chair.25,26 Another factor to consider when attempting to understand barriers to women’s active participation in academic events requiring travel is the burden of childcare, as addressed in a previous study on early-career oncologists and conferences attendance.27
We found that more than half of the lectures were presented by faculty with more than 15 years from initial certification in hematology and/or medical oncology with an insufficient number of early-career faculty. Such limited opportunity to speak at such conferences may lead to lower engagement of early-career faculty in academic activities and may ultimately lead to loss of interest in pursuing academic jobs. Efforts to recruit junior faculty members in hematology/medical oncology board review lecture series will serve as a “double duty” of both improving career advancement opportunities for junior faculty and also likely improve the representation of women in these positions.
The lack of gender equity in academia has been highlighted in previous studies indicating that women received lower wages, delayed promotions, and less research funding.28-30 Gender disparities are also prevalent in academic conferences.31 Academics can advance their careers by giving invited seminars and practicing active networking at universities and international conferences.29 Assuming the work is well presented, interesting, and scientifically rich, these activities can positively increase the visibility of a speaker. Researchers with increased visibility are expected to be more likely invited back as speakers, further enhancing their visibility.32
Limitations
Our study was limited to US-based board review lecture series; thus, future studies should consider assessing the gender and early-career faculty disparities on an international scale. In addition, it is worth noting that gender may not be accurate in all studied subjects, and in our analysis, we could not assess the percentage of invited speakers or if any invitation denials occurred. We also did not include peer-reviewed scientific oncology conferences such as those held by the American Society of Clinical Oncology and the European Society of Medical Oncology, which could have yielded important findings. Nevertheless, our study provides a robust analysis of all board review lecture series in the United States, which may help in improving the disparities experienced by women and early-career faculty in the field of hematology and medical oncology.
Conclusions
Women and early-career faculty are underrepresented in board review lecture series in hematology and medical oncology. Efforts should be made to ensure equal participation of women and early-career faculty in such important activities needed to advance academic careers.
Authorship
Contribution: S.A.H. conceived the research idea; S.A.H., S.S., L.A.-K., M.A., and H.A. collected data, performed statistical analyses, and wrote the initial draft of the manuscript; R.M. provided critical input on the methodology and analyses; and all authors reviewed and approved the final version of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Samer Al Hadidi, Myeloma Center, Winthrop P. Rockefeller Cancer Institute, University of Arkansas for Medical Sciences, Little Rock, AR; e-mail: salhadidi@uams.edu.
References
Author notes
This paper was presented at the 2022 Annual Meeting of the American Society for Clinical Oncology, 3–7 June 2022, Chicago, IL.
For data sharing, contact Samer Al Hadidi (salhadidi@uams.edu).