Key Points
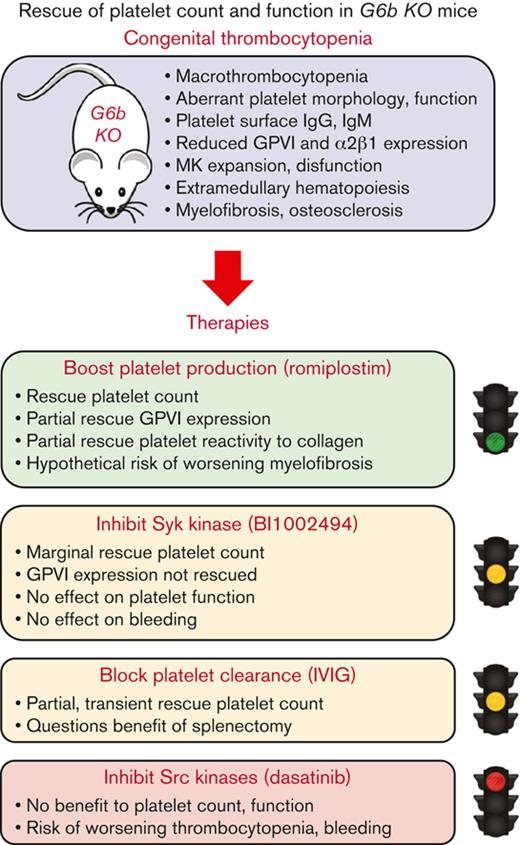
Romiplostim rescues thrombocytopenia, GPVI expression, and platelet collagen reactivity in G6b KO mice.
Intravenous immunoglobulin, Syk, and Src tyrosine kinase inhibitors have little or no benefit in rescuing the platelet phenotype in G6b KO mice.
Abstract
Mice lacking the immunoreceptor tyrosine-based inhibition motif-containing co-inhibitory receptor G6b-B (Mpig6b, G6b knockout, KO) are born with a complex megakaryocyte (MK) per platelet phenotype, characterized by severe macrothrombocytopenia, expansion of the MK population, and focal myelofibrosis in the bone marrow and spleen. Platelets are almost completely devoid of the glycoprotein VI (GPVI)-FcRγ-chain collagen receptor complex, have reduced collagen integrin α2β1, elevated Syk tyrosine kinase activity, and a subset has increased surface immunoglobulins. A similar phenotype was recently reported in patients with null and loss-of-function mutations in MPIG6B. To better understand the cause and treatment of this pathology, we used pharmacological- and genetic-based approaches to rescue platelet counts and function in G6b KO mice. Intravenous immunoglobulin resulted in a transient partial recovery of platelet counts, whereas immune deficiency did not affect platelet counts or receptor expression in G6b KO mice. Syk loss-of-function (R41A) rescued macrothrombocytopenia, GPVI and α2β1 expression in G6b KO mice, whereas treatment with the Syk kinase inhibitor BI1002494 partially rescued platelet count but had no effect on GPVI and α2β1 expression or bleeding. The Src family kinase inhibitor dasatinib was not beneficial in G6b KO mice. In contrast, treatment with the thrombopoietin mimetic romiplostim rescued thrombocytopenia, GPVI expression, and platelet reactivity to collagen, suggesting that it may be a promising therapeutic option for patients lacking functional G6b-B. Intriguingly, GPVI and α2β1 expression were significantly downregulated in romiplostim-treated wild-type mice, whereas GPVI was upregulated in romiplostim-treated G6b KO mice, suggesting a cell intrinsic feedback mechanism that autoregulates platelet reactivity depending on physiological needs.
Introduction
Platelets are essential for primary hemostasis, maintenance of vascular integrity and the innate immune response.1-3 They have also been implicated in many pathological conditions, including thrombosis, atherogenesis, and cancer metastasis.4,5 Reduced platelet counts, or thrombocytopenia, are defined by their cause, with the most common forms due to autoantibodies to platelet surface receptors, notably the integrin αIIbβ3 and GPIbα subunit, referred to as immune thrombocytopenia (ITP).6 Immune complex-mediated platelet activation can also lead to enhanced clearance and thrombocytopenia, as is the case in antiphospholipid syndrome,7 systemic lupus erythematosus,8 sepsis,9 heparin-induced thrombocytopenia and vaccine-induced immune thrombotic thrombocytopenia.10,11 Congenital thrombocytopenias caused by inherited mutations in genes regulating megakaryopoiesis and thrombopoiesis, including May-Hegglin anomaly, Bernard-Soulier syndrome and Gray platelet syndrome, are less prevalent, but clinically significant.12 Independent of bleeding complications, presence of thrombocytopenia secondary to other conditions is associated with poor prognosis and survival,13-16 making effective management essential.
The immunoreceptor tyrosine-based inhibition motif-containing co-inhibitory receptor G6b-B, also referred to as megakaryocyte (MK)/platelet inhibitor G6B (MPIG6B), has emerged as a critical regulator of platelet homeostasis.17 Targeted deletion of Mpig6b (G6b knockout, KO),18 or uncoupling G6b-B from Src homology 2 domain-containing tyrosine phosphatases 1 and 2 (Shp1 and Shp2),19-21 resulted in >75% reduction in platelet count and >35% increase in platelet volume. Thrombocytopenia was primarily because of reduced platelet production, although platelet clearance was also significantly increased in G6b KO mice.18 Marked MK expansion, secondary to elevated plasma thrombopoietin levels, was observed in G6b-B–deficient mice, with evidence of MK fragmentation and platelet release in the bone marrow. Focal myelofibrosis around clusters of MKs is a prominent feature, and the increased prevalence of osteosclerosis in aged mice is likely driven by elevated MK-derived TGF-β1 release and signaling.18,21,22 Platelets from these mice are almost completely devoid of the GPVI-FcR γ-chain collagen receptor complex, have reduced collagen integrin α2β1, elevated Syk tyrosine kinase activity, and a subset has increased surface immunoglobulins.18 Several patients from unrelated families have been reported with mutations in MPIG6B and little or no functional G6b-B.23-27 Homozygous patients presented with similar symptoms to G6b-B null and loss-of-function mouse models, including severe macrothrombocytopenia, MK expansion, and focal myelofibrosis from an early age. Successful treatment of the most severely affected family members required bone marrow transplantation.24-27
The overlapping phenotypes of G6b-B–deficient mice and humans demonstrate the importance of this receptor in both species and provide an animal model to investigate the molecular basis of the disease and the efficacy of therapies. Such a study is pertinent to the emergence of an increasing number of disease-causing mutations in MPIG6B. Standard clinical therapies for thrombocytopenia were investigated, including administration of intravenous immunoglobulin (IVIG) and Syk tyrosine kinase inhibition to block platelet clearance, and thrombopoietin mimetic romiplostim to boost MK/platelet production. Although IVIG and Syk inhibition had partial therapeutic benefits, romiplostim was the most efficacious in rescuing the platelet count, GPVI expression, and platelet reactivity to collagen in G6b KO mice. Intriguingly, romiplostim reduced the expression of GPVI and collagen integrin α2β1 in wild-type (WT) mice, suggesting a cell intrinsic feedback mechanism that autoregulates platelet reactivity depending on physiological needs.
Materials and methods
Mice
G6b KO (G6b-/-) mice were generated on a C57BL/6 background using Taconic Artemis as previously described.18 Recombination-activating gene 1 (Rag1) KO (B6.129S7-Rag1tm1Mom/J) mice were obtained from Jackson Laboratory. Cre-inducible Syk R41A knock-in (KI) mice (Syk R41Afl/fl) were generated by Ozgene (Bentley, Australia) and crossed with Pf4-Cre+ mice as described previously.28 G6b KO; Syk R41A KI; Pf4-Cre+mice and G6b/Rag1 double KO (DKO) mice were bred by crossing Syk R41A KI; Pf4-Cre+ and Rag1 KO mice, respectively, with G6b KO mice. The control mice were pure C57BL/6 (G6b+/+) mice, referred to as WT. All procedures were performed with the UK Home Office approval in accordance with the Animals Scientific Procedures Act of 1986 and with the French Ministry of Research, in accordance with the guidelines of the Regional Committee for Ethics in Animal Experimentation of Strasbourg (CREMEAS, CEEA-35).
Antibodies and reagents
Romiplostim and IVIG were purchased from the Pharmacy Department of University Hospital Birmingham, UK. BI1002494 was kindly provided by Boehringer Ingelheim via its open innovation platform opnMe.com.29 The rat-anti-mouse CLEC2 antibody (17D9) was obtained from Serotech (Oxford, United Kingdom). FITC-conjugated GPVI and α2 antibodies were obtained from Emfret Analytics (Eibelstadt, Germany). All other chemicals and antibodies were sourced as previously described.18
Blood sample collection and analysis
Whole blood was collected from the tail vein at the indicated time points during the experiments using 5 mM EDTA. At the end of the experiments, the mice were anesthetized using isoflurane, asphyxiated with CO2, and bled from the vena cava into 1:10 (v:v) acid-citrate-dextrose. Platelet counts and volumes were measured using an ABX Pentra 60 Hematology Analyzer (Block Scientific) and automatic cell counter (Scil Animal Care Company, Altorf, France).
Quantification of autoantibodies
Whole blood from WT and G6b KO mice was collected weekly from weeks 4 to 8. The blood was washed twice to eliminate plasma and circulating Ig. Autoantibodies fixed to the platelet surface were revealed by double staining with anti-GPIbα (Ram-1 coupled to Alexa 647) and either IgM (goat anti-mouse-IgM coupled to Alexa 488) or IgG (goat anti-mouse-IgG coupled to Alexa 488). Samples were analyzed using a flow cytometer (LSRFortessa cell analyzer; BD Biosciences, Oxford, United Kingdom), and data were analyzed using the BD FACS Diva software.
Administration of IVIG
Ten-week-old WT and G6b KO mice received intravenous injections of 2 g/kg body weight.30 Blood samples were collected at day 15 from the tail veins and day 20 from the vena cava for analysis of blood parameters.
Administration of romiplostim
Ten-week-old WT and G6b KO mice received subcutaneous injections of either vehicle (saline) or romiplostim (100 μg/kg body weight; Amgen) every 3 days for 3 weeks. The doses and administration schedules were selected according to previous studies on mice.31 Blood samples were analyzed for platelet count and volume before the onset of the experiment and on days 8 and 15. On day 21, the mice were culled and blood was drawn from the vena cava for platelet isolation.
Administration of BI2002494
BI1002494 (C23H24N3O5)29 was dissolved in Natrosol 0.5% (Natrosol 250 HX Pharma) and administered by oral gavage to ten-week-old G6b KO mice at 30 mg/kg body weight twice a day for 5 days. Blood samples were collected daily from the tail veins and vena cava on day 5 before hematology analysis.
Flow cytometry
ACD anticoagulated whole blood was incubated with FITC-conjugated rat-anti-mouse antibodies for GPVI and α2β1 (Emfret, Wurzburg, Germany) and analyzed using an Accuri C6 and Fortessa flow cytometers (BD Biosciences), as previously described.18
Analysis of platelet aggregation and secretion of adenosine triphosphate (ATP)
Washed mouse platelets (2 × 108/mL) were prepared and analyzed for aggregation and ATP secretion with a lumi-aggregometer (Chrono-Log, Havertown, PA), as previously described.18
Tail bleeding assay
Tail bleeding experiments were performed on 20 to 30 g male and female mice anesthetized with isoflurane and intraperitoneally injected with buprenorphine. The terminal 3 mm of the tail was cut transversally using a sharp razor blade, and immediately immersed in isotonic saline at 37°C. Mice were allowed to bleed for a maximum of 30 minutes. The bleeding time was defined as the time required for the complete arrest of bleeding. If bleeding did not cease after 30 minutes, the tail was cauterized and the bleeding time was 30 minutes. The amount of blood lost was estimated by measuring hemoglobin levels using a colorimetric method.
Statistical analysis
Data are presented as mean ± standard error of the mean (SEM). Student t-test was used to compare sample means and determine statistical significance between pairs of samples. One-way or two-way analysis of variance (ANOVA) followed by post hoc tests was used to compare differences between multiple observations of more than one variable. P < .05 was considered statistically significant in all cases.
Results
IVIG partially rescues macrothrombocytopenia in G6b KO mice
We previously showed that G6b KO mice exhibit thrombocytopenia,18 which is more severe in females.22 We demonstrated here that this is the case from 4 weeks of age (Figure 1A). Furthermore, the previous characterization of G6bKO mice identified 2 potential mechanisms for reduced platelet count, increased platelet clearance, and reduced platelet production. Evidence of increased platelet clearance was supported by high levels of IgM and IgG bound to the surface of G6b KO platelets.18 This was further confirmed to be the case from 4 weeks old mice, with G6b KO mice exhibiting higher level of IgM and IgG bound to their platelet surface compared with WT (Figure 1B-C). Therefore, we first investigated common treatments for ITP. A common first line treatment is administration of IVIG, which predominantly blocks Fc-receptors on phagocytosing cells and reduces platelet clearance. In this study, WT and G6b KO mice were treated with 2 g/kg IVIG, and platelet counts and volumes were monitored 15 and 20 days after treatment. We showed that administration of IVIG had no effect on platelet count in WT mice but partially rescued the macrothrombocytopenia observed in G6b KO mice 15 days after treatment (Figure 2A-B), with this effect being reduced by day 20. The recovery of platelet counts correlated with marginal recovery of GPVI and α2β1 expression (Figure 2C-D). Nevertheless, the platelet count of G6b KO mice remained significantly lower than that observed in WT mice following IVIG treatment.
G6b-B–deficient platelets have increased surface IgM and IgG abundance. (A) Whole blood platelet counts from young, 4 to 8 weeks WT, and male and female G6b KO mice were measured. (B-C) Platelets from WT and G6b KO mice were double-stained for GPIbα and either IgM (B) or IgG (C). Flow cytometry analysis revealed that G6b KO mice exhibit higher level of IgM and IgG bound to their platelet surface than WT. Data are means ± SEM. n = 12 per condition.
G6b-B–deficient platelets have increased surface IgM and IgG abundance. (A) Whole blood platelet counts from young, 4 to 8 weeks WT, and male and female G6b KO mice were measured. (B-C) Platelets from WT and G6b KO mice were double-stained for GPIbα and either IgM (B) or IgG (C). Flow cytometry analysis revealed that G6b KO mice exhibit higher level of IgM and IgG bound to their platelet surface than WT. Data are means ± SEM. n = 12 per condition.
IVIG rescues partially macrothrombocytopenia in G6b-deficient mice.WT and G6b KO mice received 2 g/kg IVIG intravenously once a day for 20 days. (A) Platelet counts and (B) volumes were measured before (day 0), and 15 and 20 days after IVIG administration. IVIG partially rescued the macrothrombocytopenia observed in G6b KO mice 15 days after treatment (A-B), with this effect being reduced by day 20. (C) GPVI and (D) α2β1 platelet surface expression in WT and G6b KO mice measured using flow cytometry after 15 days of 2 g/kg IVIG administration. A marginal recovery of GPVI and α2β1 expression was observed in G6b-deficient treated mice. n = 4 mice per genotype per condition. ∗P < .05, ∗∗∗P < .001, 2-way ANOVA with Tukey’s test, mean ± SEM.
IVIG rescues partially macrothrombocytopenia in G6b-deficient mice.WT and G6b KO mice received 2 g/kg IVIG intravenously once a day for 20 days. (A) Platelet counts and (B) volumes were measured before (day 0), and 15 and 20 days after IVIG administration. IVIG partially rescued the macrothrombocytopenia observed in G6b KO mice 15 days after treatment (A-B), with this effect being reduced by day 20. (C) GPVI and (D) α2β1 platelet surface expression in WT and G6b KO mice measured using flow cytometry after 15 days of 2 g/kg IVIG administration. A marginal recovery of GPVI and α2β1 expression was observed in G6b-deficient treated mice. n = 4 mice per genotype per condition. ∗P < .05, ∗∗∗P < .001, 2-way ANOVA with Tukey’s test, mean ± SEM.
The most recent American Society of Hematology guidelines recommend splenectomy,32 which removes both the site of platelet clearance and the site of anti-platelet antibody production, as a second-line treatment for congenital thrombocytopenia.33 We therefore genetically ablated immune responses by crossing G6b KO mice with immune compromised Rag1 KO mice, which lack mature B- and T-cells.34 Rag1 KO mice exhibit normal platelet counts and volumes, as shown in Figure 3A and B. However, deficiency of the immune response did not rescue the phenotype in G6b KO mice, as G6b/Rag1 DKO mice exhibited severe macrothrombocytopenia (Figure 3A-B) and decreased GPVI and α2β1 expression, similar to G6b KO mice (Figure 3C-D). Therefore, targeting immune-mediated platelet clearance is not effective in ameliorating thrombocytopenia in G6b KO mice.
Ablation of the immune system does not rescue the macrothrombocytopenia in G6b-deficient mice. (A) Platelet counts and (B) volumes of WT, G6b KO, Rag1 KO, and G6b/Rag1 double-knockout (DKO) mice were measured, n = 10 to 26 mice per genotype. Rag1 KO mice exhibited normal platelet counts and volumes. However, deficiency of the immune response did not rescue the phenotype in G6b KO mice, as G6b/Rag1 DKO mice exhibited severe macrothrombocytopenia (A-B). (C) GPVI and (D) α2β1 platelet surface expression in WT, G6b KO, Rag1 KO, and G6b/Rag1 DKO mice was measured by flow cytometry, n = 8 to 10 mice per genotype. G6b/Rag1 DKO mice exhibited decreased GPVI and α2β1 expression, similar to those observed in G6b KO mice. ∗∗∗P < .001, 1-way ANOVA with Dunnett’s test, mean ± SEM.
Ablation of the immune system does not rescue the macrothrombocytopenia in G6b-deficient mice. (A) Platelet counts and (B) volumes of WT, G6b KO, Rag1 KO, and G6b/Rag1 double-knockout (DKO) mice were measured, n = 10 to 26 mice per genotype. Rag1 KO mice exhibited normal platelet counts and volumes. However, deficiency of the immune response did not rescue the phenotype in G6b KO mice, as G6b/Rag1 DKO mice exhibited severe macrothrombocytopenia (A-B). (C) GPVI and (D) α2β1 platelet surface expression in WT, G6b KO, Rag1 KO, and G6b/Rag1 DKO mice was measured by flow cytometry, n = 8 to 10 mice per genotype. G6b/Rag1 DKO mice exhibited decreased GPVI and α2β1 expression, similar to those observed in G6b KO mice. ∗∗∗P < .001, 1-way ANOVA with Dunnett’s test, mean ± SEM.
Syk loss-of-function rescues macrothrombocytopenia and GPVI expression
We previously demonstrated that G6b-B inhibits constitutive signaling from GPVI and CLEC-2 in transiently transfected DT40 cells.35 In addition, we also showed that G6b KO platelets have higher basal Syk activity than WT platelets,18 and that G6b-B-Shp2 targets either Syk recruitment or activation downstream of CLEC-2.20 We, therefore, investigated whether inhibiting Syk might rescue the thrombocytopenia in G6b KO mice. First, using a genetic approach, we utilized a platelet-specific Syk R41A KI mouse model,28 which exhibited reduced Syk activity, specifically downstream of immunoreceptor tyrosine-based activation motif (ITAM)-mediated signaling. Syk R41A KI mice were crossed with G6b KO mice to investigate potential rescue of the G6b KO phenotype. We showed that reducing ITAM-mediated Syk activity successfully restored both platelet counts and volumes in G6b KO mice to those observed in WT mice (Figure 4A-B), suggesting that G6b-B-mediated Syk inhibition may be essential for normal platelet production. Importantly, GPVI and α2β1 surface expression was also fully restored in G6b KO mice on the Syk R41A background (Figure 4C-D), implicating increased Syk activity as an underlying cause of the downregulation of these receptors in G6b KO mice.
Reduced Syk activity rescues macrothrombocytopenia and GPVI expression in G6b-deficient mice. (A) Platelet counts and (B) volumes of WT, G6b KO, G6b-/-R41A+/+Cre+, and G6b-/-R41Afl/flCre+ mice were measured, n = 9 to 43 mice/genotype. (C) GPVI and (D) α2β1 platelet surface expression of WT, G6b KO, G6b-/-R41A+/+Cre+, and G6b-/-R41Afl/flCre+ mice were measured by flow cytometry n = 5 to 18 mice per genotype. ∗∗∗P < .001, 1-way ANOVA with Dunnett’s test, mean ± SEM. (E-J) G6b KO mice received BI1002494 (30 mg/kg per bid) orally via gavage twice a day for 5 days. (E) Platelet counts and (F) volumes of G6b KO mice were monitored before (day 0) and every day for 5 days, n = 10 to 15 mice per genotype. ∗∗P < .01, ∗∗∗P < .001, 2-way ANOVA Tukey’s test, mean ± SEM. (G) GPVI and (H) α2β1 platelet surface expression of WT and G6b KO mice were measured 5 days after BI1002494 administration (30 mg/kg per bid) by flow cytometry, n = 6 to 10 mice per genotype. (I) Hemostatic response was measured 5 days after BI1002494 administration, in saline tail bleeding assay by an excision of a 3 mm portion of the tail tip followed by immersion of the tail in 0.9% isotonic saline at 37 °C. Plotted is the time to complete the arrest of bleeding. Each symbol represents 1 animal. (J) Blood loss was measured using colorimetric dosage of hemoglobin. Experiments were conducted in a double-blinded manner, n = 7 mice per genotype per condition. 1-way ANOVA with Sidak’s test, mean ± SD. ns, non-significant.
Reduced Syk activity rescues macrothrombocytopenia and GPVI expression in G6b-deficient mice. (A) Platelet counts and (B) volumes of WT, G6b KO, G6b-/-R41A+/+Cre+, and G6b-/-R41Afl/flCre+ mice were measured, n = 9 to 43 mice/genotype. (C) GPVI and (D) α2β1 platelet surface expression of WT, G6b KO, G6b-/-R41A+/+Cre+, and G6b-/-R41Afl/flCre+ mice were measured by flow cytometry n = 5 to 18 mice per genotype. ∗∗∗P < .001, 1-way ANOVA with Dunnett’s test, mean ± SEM. (E-J) G6b KO mice received BI1002494 (30 mg/kg per bid) orally via gavage twice a day for 5 days. (E) Platelet counts and (F) volumes of G6b KO mice were monitored before (day 0) and every day for 5 days, n = 10 to 15 mice per genotype. ∗∗P < .01, ∗∗∗P < .001, 2-way ANOVA Tukey’s test, mean ± SEM. (G) GPVI and (H) α2β1 platelet surface expression of WT and G6b KO mice were measured 5 days after BI1002494 administration (30 mg/kg per bid) by flow cytometry, n = 6 to 10 mice per genotype. (I) Hemostatic response was measured 5 days after BI1002494 administration, in saline tail bleeding assay by an excision of a 3 mm portion of the tail tip followed by immersion of the tail in 0.9% isotonic saline at 37 °C. Plotted is the time to complete the arrest of bleeding. Each symbol represents 1 animal. (J) Blood loss was measured using colorimetric dosage of hemoglobin. Experiments were conducted in a double-blinded manner, n = 7 mice per genotype per condition. 1-way ANOVA with Sidak’s test, mean ± SD. ns, non-significant.
Syk inhibition partially restores platelet counts in G6b KO mice
To further characterize the contribution of Syk kinase to platelet recovery, we used the selective small-molecule Syk kinase inhibitor BI1002494.29 Mice were administered twice a day for 5 days with 30 mg/kg BI1002494 per dose. A trend toward increased platelet count was observed in BI1002494-treated male G6b KO mice compared with vehicle-treated mice under these conditions, which was more prominent and significant in female G6b KO mice (Figure 4E). Platelet volumes were unaltered under these conditions (Figure 4F), as was platelet GPVI and α2β1 surface expression (Figure 4G-H). Platelet aggregation and P-selectin expression were also normal in response to PAR-4 peptide and anti-CLEC-2 antibody in BI1002494-treated mice compared with vehicle-treated mice (supplemental Figure 1), as was blood loss measured by tail bleeding (Figure 4I-J).
We also sought to assess whether Src family kinase inhibition, which lies upstream of Syk, might also be effective in rescuing the thrombocytopenia observed in G6b KO mice. The effect of in vivo administration of dasatinib (5 mg/kg per day for 7 days) on platelet count was investigated. Treatment with dasatinib caused a reduction in the platelet number in WT mice, as previously described,36 however, no significant effect was observed in G6b KO mice (supplemental Figure 2A-B).
Collectively, these results demonstrated that macrothrombocytopenia and aberrant platelet function exhibited by G6b KO mice can only be partially rescued by reducing Syk kinase activity, as summarized in supplemental Table 1.
Romiplostim rescues thrombocytopenia in G6b-B–deficient mice
Thrombopoietin receptor agonists, including romiplostim and eltrombopag, which drive MK expansion are increasingly utilized in the treatment of thrombocytopenia, while splenectomies have declined.37-39 Romiplostim is a peptibody administered subcutaneously to treat chronic ITP.37,40 It mimics thrombopoietin binding to its receptor, Mpl, therefore driving differentiation and maturation of MKs.40 100 μg/kg of romiplostim was injected into WT mice every 3 days, leading to a 4-fold increase in platelet count 8 days after the beginning of the protocol (Figure 5A). The platelet count further increased after 21 days of treatment, reaching a 5-fold increase (Figure 5A). Romiplostim also increased platelet counts in G6b KO mice, with a 5-fold increase by day 8 and vehicle-treated WT levels (Figure 5A), and an 8-fold increase by day 21, but significantly below romiplostim-treated WT levels (Figure 5A). A minor increase in mean platelet volume was observed in romiplostim-treated WT mice, which was marginally more prominent in female mice, but no further increase was observed with time (Figure 5B). Platelet volume was significantly higher in G6b KO mice at baseline but did not increase significantly in romiplostim-treated G6b KO mice (Figure 5B).
Romiplostim rescues thrombocytopenia in G6b-deficient mice. (A) Platelet counts and (B) volumes of WT and G6b KO mice were measured before (day 0) and after 8, 15, and 21 days of administration of 100 μg/kg body weight romiplostim. Romiplostim increased platelet counts in G6b KO mice but did not affect platelet volume. (C) GPVI and (D) α2β1 platelet surface expression in WT and G6b KO mice measured by flow cytometry before (vehicle) and after 21 days of romiplostim administration. Results are expressed as the mean fluorescent intensity (MFI) ± SEM. In WT mice, romiplostim induces a 40% reduction in GPVI expression and 25% reduction in α2β1 expression. However, romiplostim induced a 5-fold increase in GPVI expression in G6b KO mice but had no effect on α2β1 expression. n = 8 mice per condition. ∗P < .05, ∗∗∗P < .001, 2-way ANOVA Tukey’s test.
Romiplostim rescues thrombocytopenia in G6b-deficient mice. (A) Platelet counts and (B) volumes of WT and G6b KO mice were measured before (day 0) and after 8, 15, and 21 days of administration of 100 μg/kg body weight romiplostim. Romiplostim increased platelet counts in G6b KO mice but did not affect platelet volume. (C) GPVI and (D) α2β1 platelet surface expression in WT and G6b KO mice measured by flow cytometry before (vehicle) and after 21 days of romiplostim administration. Results are expressed as the mean fluorescent intensity (MFI) ± SEM. In WT mice, romiplostim induces a 40% reduction in GPVI expression and 25% reduction in α2β1 expression. However, romiplostim induced a 5-fold increase in GPVI expression in G6b KO mice but had no effect on α2β1 expression. n = 8 mice per condition. ∗P < .05, ∗∗∗P < .001, 2-way ANOVA Tukey’s test.
Romiplostim increases GPVI expression and collagen reactivity in G6b KO mice
We next investigated the effect of romiplostim on the expression of collagen receptors GPVI and α2β1 in G6b KO mice. Romiplostim induced a 40% reduction in GPVI expression in WT mice as previously shown,31 and a 25% reduction in α2β1 expression. Unexpectedly, romiplostim induced a 5-fold increase in GPVI expression in G6b KO mice (Figure 5C) but had no effect on α2β1 expression (Figure 5D). Although GPVI levels remained significantly lower in romiplostim-treated G6b KO mice than in their WT counterparts, they were much closer than those in untreated mice (Figure 5C), and α2β1 levels were the same (Figure 5D).
We also performed platelet function testing in vitro by measuring platelet aggregation and ATP secretion to determine whether romiplostim treatment could rescue other platelet defects observed in G6b KO mice. As previously described,18 platelets from G6b KO mice did not aggregate or secrete ATP in response to the GPVI-specific agonist, collagen-related peptide (CRP, 30 and 3 μg/mL), and significantly diminished the response to collagen (3 μg/mL) (Figure 6A-C, supplemental Figure 3A-C), consistent with a reduction in GPVI expression. However, following romiplostim administration, platelets from G6b KO mice aggregated normally in response to 30 μg/mL CRP and 3 μg/mL collagen compared with those from treated WT mice (Figure 6A,C, supplemental Figure 3A,C). An increased response to 3 μg/mL CRP was also observed in treated vs untreated G6b KO mouse platelets, but this was still reduced compared with WT (Figure 6B, supplemental Figure 3B). ATP secretion, a marker of platelet dense-granule secretion, was partially rescued by all concentrations of CRP and collagen tested (Figure 6A-C, supplemental Figure 3A-C).
Romiplostim rescues platelet reactivity in G6b-deficient mice. Washed platelet aggregation and ATP secretion of WT and G6b KO mice before and after 21 days after romiplostim administration were measured using lumi-aggregometry in response to (A-B) 30 and 3 μg/mL collagen-related peptide (CRP), (C) 3 μg/mL collagen, (D) 3 μg/mL CLEC2 Ab and (E) 0.06 U/mL thrombin. Following romiplostim administration, platelets from G6b KO mice aggregated normally in response to 30 μg/mL CRP and 3 μg/mL collagen, compared with treated WT mice (A,C) and an increased response to 3 μg/mL CRP was observed in treated vs untreated G6b KO mouse platelets (B). Romiplostim treatment also partially attenuates the response of WT and G6b KO platelets to anti-CLEC-2 antibody (D) and fully restores reversible aggregation and reduced ATP secretion in response to 0.06 U/mL thrombin in G6b KO mice (E). Representative traces are shown, n = 5 to 8 mice per genotype per condition.
Romiplostim rescues platelet reactivity in G6b-deficient mice. Washed platelet aggregation and ATP secretion of WT and G6b KO mice before and after 21 days after romiplostim administration were measured using lumi-aggregometry in response to (A-B) 30 and 3 μg/mL collagen-related peptide (CRP), (C) 3 μg/mL collagen, (D) 3 μg/mL CLEC2 Ab and (E) 0.06 U/mL thrombin. Following romiplostim administration, platelets from G6b KO mice aggregated normally in response to 30 μg/mL CRP and 3 μg/mL collagen, compared with treated WT mice (A,C) and an increased response to 3 μg/mL CRP was observed in treated vs untreated G6b KO mouse platelets (B). Romiplostim treatment also partially attenuates the response of WT and G6b KO platelets to anti-CLEC-2 antibody (D) and fully restores reversible aggregation and reduced ATP secretion in response to 0.06 U/mL thrombin in G6b KO mice (E). Representative traces are shown, n = 5 to 8 mice per genotype per condition.
In contrast to GPVI stimulation, platelets from G6b KO mice exhibit enhanced reactivity to an activating anti-CLEC-2 antibody (Figure 6D, supplemental Figure 3D). This was because of increased signaling in the absence of inhibition by G6b-B.18,20 Romiplostim treatment also partially rescued this phenotype, by marginally attenuating the response of WT and G6b KO platelets to the anti-CLEC-2 antibody (Figure 6D, supplemental Figure 3D). In addition, reversible aggregation and reduced ATP secretion in response to 0.06 U/mL thrombin in G6b KO mice was restored following romiplostim treatment (Figure 6E). These data indicate that romiplostim is effective in rescuing both the platelet count and reactivity to various agonists in G6b KO mice, as summarized in supplemental Table 2.
Discussion
The results of this study demonstrated that romiplostim was effective in boosting platelet counts and rescuing platelet function in mice lacking the co-inhibitory receptor G6b-B. In contrast, inhibiting or ablating the immune response to prevent platelet clearance is less effective in rescuing the platelet phenotype in G6b-B–deficient mice. Surprisingly, GPVI and α2β1 were downregulated in romiplostim-treated WT mice, whereas GPVI was upregulated in G6b KO mice following the same treatment, resulting in more comparable platelet responses to collagen and CRP than in untreated mice (Figure 7). Furthermore, platelets from romiplostim-treated WT and G6b KO mice responded similarly to anti-CLEC-2 antibody and thrombin compared with untreated mice, suggesting a cell intrinsic feedback mechanism that autoregulates platelet reactivity depending on physiological needs.
Effects of romiplostim in WT and G6b-B–deficient mice. Romiplostim is a thrombopoietin receptor agonist clinically used to treat chronic ITP. It mimics thrombopoietin binding to its receptor, Mpl, therefore driving differentiation and maturation of MKs. In this study, we demonstrate that (A) treatment of WT mice with romiplostim leads to an 8-fold increase in platelet counts to supraphysiological levels. It also reduces GPVI and α2β1 expression in WT mice. We hypothesize that romiplostim drives a cell intrinsic negative feedback pathway that autoregulates platelet reactivity to collagen depending, suppressing their thrombotic capacity. (B) Romiplostim successfully rescued thrombocytopenia in G6b KO mice, with an increase in the platelet counts to physiological levels. It also partially rescued GPVI expression and platelet reactivity to collagen in G6b KO mice, suggesting a loss of negative feedback. Romiplostim proved to be the most effective therapy tested for rescuing the platelet phenotype in G6b KO mice.
Effects of romiplostim in WT and G6b-B–deficient mice. Romiplostim is a thrombopoietin receptor agonist clinically used to treat chronic ITP. It mimics thrombopoietin binding to its receptor, Mpl, therefore driving differentiation and maturation of MKs. In this study, we demonstrate that (A) treatment of WT mice with romiplostim leads to an 8-fold increase in platelet counts to supraphysiological levels. It also reduces GPVI and α2β1 expression in WT mice. We hypothesize that romiplostim drives a cell intrinsic negative feedback pathway that autoregulates platelet reactivity to collagen depending, suppressing their thrombotic capacity. (B) Romiplostim successfully rescued thrombocytopenia in G6b KO mice, with an increase in the platelet counts to physiological levels. It also partially rescued GPVI expression and platelet reactivity to collagen in G6b KO mice, suggesting a loss of negative feedback. Romiplostim proved to be the most effective therapy tested for rescuing the platelet phenotype in G6b KO mice.
The use of thrombopoietin receptor agonists increases platelet counts and decreases the risk of bleeding in patients with ITP.41 Two such thrombopoietin receptor agonists, romiplostim and eltrombopag, have been approved by the US Food and Drug Administration for the treatment of thrombocytopenia.32 In this study, we showed that administration of romiplostim successfully restored platelet counts to physiological levels in G6b KO mice, but not to the same extent as in WT mice, despite G6b KO mice having significantly more MKs. This correlates with the severe impairment in proplatelet formation and platelet production by G6b-B–deficient MKs, which is the primary cause of thrombocytopenia in these mice.18 Mean platelet volumes were marginally increased in romiplostim-treated WT mice, presumably because more young platelets were released into the circulation, but remained unaltered in G6b KO mice, which were already enlarged. In addition, GPVI and α2β1 expression, platelet aggregation, and ATP secretion were rescued in response to collagen and thrombin. This improved thrombin response was surprising, as it acts via G protein-coupled receptors that are not typically regulated by immunoreceptor tyrosine-based inhibition motif -containing receptors. Because G6b KO mice have a broad spectrum of morphologically diverse platelets as assessed by electron microscopy,18 ranging from platelets with few if any granules to those with a normal complement of granules, we speculate that these findings may be because of skewing of the platelet population toward more biologically active platelets in response to romiplostim. Further preclinical testing is needed to determine effects of G6b-B–deficient MKs, mechanism of action, and therapeutic window at which the platelet phenotype and bleeding diathesis are resolved, but myelofibrosis and osteosclerosis associated with G6b-B-deficiency are not exacerbated.22,41
One of the most intriguing and unexpected findings of this study was the inverse effect of romiplostim on platelet receptor expression and reactivity in WT and G6b KO mice (Figure 7). Our working hypothesis was that MKs and platelets possess cell intrinsic feedback mechanisms that autoregulate platelet reactivity, depending on what is needed for survival. If platelets are biologically normal and their counts increase to supraphysiological levels, as is the case in romiplostim-treated WT mice, less active platelets are preferred to guard against unwarranted thrombosis. The opposite is true in G6b KO mice, which require more active platelets to compensate for functional deficits and to prevent bleeding. This corresponds to a growing body of evidence that the platelet phenotype is dictated by the pathological context.42-46 The underlying mechanisms remain undefined.
Based on our initial characterization of G6b KO mice, auto-antibodies have been proposed to contribute to the phenotype.18 Currently, one of the recommended first line treatments advised by the American Society of Hematology is the administration of IVIG,32 which blocks Fc receptors on phagocytes and prevents platelet clearance. Administration of IVIG only transiently and partially rescued the platelet count, whereas ablation of B- and T-cell populations using Rag1 KO mice proved ineffective in increasing the G6b KO platelet count, demonstrating that anti-platelet auto-antibodies play little or no role in inducing thrombocytopenia in these mice and arguing against splenectomy as a therapeutic option. The lack of efficacy in inhibiting platelet clearance mechanisms is supported by recent findings from a G6b-B loss-of-function mouse model (G6b-B diY/F KI),20 which recapitulates most aspects of the G6b KO phenotype, but presents with no clearance defect when platelet kinetics are modeled.20 In addition to the partial increase in platelet count and reduction in platelet volume with IVIG, the expression of GPVI and collagen integrin α2β1 was also marginally increased, which may reflect the rescue of a subpopulation of platelets targeted for destruction.
Syk inhibitors were recently US Food and Drug Administration approved for the treatment of ITP, by inhibiting phagocytosis. As we previously showed that Syk activity is elevated in resting G6b KO platelets,18 we tested the effect of Syk loss-of-function and inhibition in G6b KO mice, which may contribute to increased clearance owing to pre-activation and GPVI-FcR γ-chain down-regulation, due to tonic signaling. Indeed, Syk loss-of-function rescued the platelet count, volume, GPVI, and α2β1 expression in G6b KO mice. However, the Syk inhibitor BI1002494 had a much milder effect, only partially rescuing the platelet count but not GPVI and α2β1 expression or bleeding. Although this is likely because of the dosing regimen, finding a therapeutic window that corrects the platelet count without severely compromising the hemostatic activity of platelets or immune response is questionable.
We hypothesized that elevated Syk activity in G6b-B–deficient platelets results in tonic GPVI-FcR γ-chain signaling, triggering negative feedback and downregulation of the entire complex. This explains why Syk loss-of-function rescued GPVI expression in G6b KO mice. We have previously reported increased ADAM-10 levels on the surface of G6b KO mouse platelets,18 which causes shedding of the GPVI ectodomain. We also observed a concomitant reduction in FcR γ-chain expression, which is required for GPVI expression. Hence, the downregulation of the GPVI-FcR γ-chain complex in G6b KO platelets is multifactorial, and the predominant underlying mechanism is likely context dependent.
Interestingly, expression of the hemITAM-containing receptor CLEC-2, which also signals via Syk, albeit with different kinetics and stoichiometry compared with GPVI-FcR γ-chain,28,47 was not downregulated in G6b KO platelets, despite elevated Syk activity. This may be partially because of the stability of the GPVI-FcR γ-chain-Syk complex compared with the CLEC-2-Syk complex, which comprises 2 phosphorylated CLEC-2 receptors and 1 Syk molecule. The tandem SH2 domains of Syk contribute cooperatively to the high affinity binding to the tandem phospho-tyrosine residues of the FcR γ-chain ITAM, compared with the substantially lower affinity of a single Syk SH2 domain binding to monophosphorylated ITAM,48,49 or 1 vs 2 phosphorylated hemITAM CLEC-2 receptors.47,50 Therefore, the strength and duration of signaling from the GPVI-FcR γ-chain might be greater than that from CLEC-2, thus eliciting a more robust negative feedback signal.
In conclusion, boosting platelet production using thrombopoietin mimetics rescued platelet counts and partially rescued platelet reactivity in G6b-B–deficient mice. Further research is required to determine the therapeutic window and potential adverse side-effects, particularly regarding the exacerbation of myelofibrosis and osteosclerosis, as well as to investigate the cell intrinsic feedback mechanisms that autoregulate platelet reactivity in response to romiplostim in the presence and absence of G6b-B.
Acknowledgments
A.M. was a BHF Intermediate Basic Science Research Fellow (FS/15/58/31784), and a research fellow at the Etablissement Français du Sang (EFS). A.M. is currently an INSERM Researcher. B.M. is a researcher at the EFS. A.B. is currently a postdoctoral researcher funded by the University of Strasbourg Initiative of Excellence (IdEx) and Gutenberg Chaire. M.J.G. was funded by a Medical Research Council PhD studentship (GBT1564) and is currently a postdoctoral fellow at New York University. C.W.S. is a postdoctoral researcher at the University of Birmingham. S.P.W. is a BHF Chair (CH03/003), and Y.A.S. was a BHF Senior Basic Science Research Fellow (FS/13/1/29894), and is currently an INSERM Director of Research.
The authors thank Caroline Chadwick (Birmingham) and Monique Freund, Catherine Ziessel, and colleagues (EFS) for exceptional animal husbandry and technical assistance.
This work was funded by BHF Programme Grant RG/15/13/31673 (Y.A.S.), INSERM, EFS, and Association de Recherche et Développement en Médecine et Santé Publique (ARMESA).
Authorship
Contribution: A.M. conceptualized, designed and performed the experiments, analyzed the data, wrote and revised the manuscript; B.M., A.B., D.H., M.L.R, M.J.G., C.W.S., and S.H. performed experiments, analyzed the data, and revised the manuscript; H.d.l.S. designed experiments, analyzed the data, and revised the manuscript; C.G. discussed the study and revised the manuscript; L.S.K.W. provided Rag1 KO mice, discussed the study, and revised the manuscript; S.P.W. provided Syk R41A KI mice, discussed the study, and revised the manuscript; Y.A.S. conceptualized, designed, and performed experiments, analyzed data, wrote and revised the manuscript.
Conflict-of-interest disclosure: The authors have no competing financial interests to declare.
Correspondence: Alexandra Mazharian, UMR-S 1255 INSERM, Université de Strasbourg, EFS Grand-Est, 10 rue Spielmann, F-67065, Strasbourg Cedex, France; e-mail: alexandra.mazharian@efs.sante.fr.
References
Author notes
Data are available on request from the corresponding author, Alexandra Mazharian (Alexandra.Mazharian@efs.sante.fr).
The full-text version of this article contains a data supplement.