Key Points
Compensation plans based solely on clinical productivity are associated with high burnout among hematologists and oncologists.
Increased utilization of advanced practice providers is inversely associated with high burnout among community hematologists and oncologists.
Abstract
Burnout is prevalent throughout medicine. Few large-scale studies have examined the impact of physician compensation or clinical support staff on burnout among hematologists and oncologists. In 2019, the American Society of Hematology conducted a practice survey of hematologists and oncologists in the AMA (American Medical Association) Masterfile; burnout was measured using a validated, single-item burnout instrument from the Physician Work–Life Study, while satisfaction was assessed in several domains using a 5-point Likert scale. The overall survey response rate was 25.2% (n = 631). Of 411 respondents with complete responses in the final analysis, 36.7% (n = 151) were from academic practices and 63.3% (n = 260) from community practices; 29.0% (n = 119) were female. Over one-third (36.5%; n = 150) reported burnout, while 12.0% (n = 50) had a high level of burnout. In weighted multivariate logistic regression models incorporating numerous variables, compensation plans based entirely on relative value unit (RVU) generation were significantly associated with high burnout among academic and community physicians, while the combination of RVU + salary compensation showed no significant association. Female gender was associated with high burnout among academic physicians. High advanced practice provider utilization was inversely associated with high burnout among community physicians. Distinct patterns of career dissatisfaction were observed between academic and community physicians. We propose that the implementation of compensation models not based entirely on clinical productivity increased support for women in academic medicine, and expansion of advanced practice provider support in community practices may address burnout among hematologists and oncologists.
Introduction
Burnout is prevalent in all fields of medicine, affecting about half of US physicians.1,2 Burnout is associated with adverse effects on patient care, healthcare quality and productivity, and physician health.3,4 Long work hours, use of electronic health record systems, and high administrative burdens are associated with burnout across different healthcare disciplines.4-8 An association with productivity-based compensation models, which incentivize payment based on numbers of patients seen or relative value units (RVUs) generated, has been suggested as well.9 While some analyses have observed an overall improvement in burnout rates in recent years, the specific trends differ according to medical specialty, practice setting, and gender, with female physicians demonstrating higher burnout rates than male physicians across multiple disciplines.3,10-13
Among internal medicine subspecialties, burnout rates vary considerably.14-17 In medical oncology, burnout rates of up to 70% globally have been reported, with 44.7% of US oncologists experiencing burnout according to a 2012-2013 survey conducted by ASCO (American Society of Clinical Oncology) and 71% of European oncologists ≤40 years of age reporting burnout in a 2013-2014 survey from the European Society for Medical Oncology.3,18,19 Factors associated with burnout in the oncology workforce include young age, increased work hours, poor work/life balance, and increased clerical burdens.3,19 Satisfaction measures are lower among oncologists in private practice than those at academic centers.3 The potential impact of advanced practice providers (APPs), including nurse practitioners and physician assistants, on physician burnout is unknown, although the incorporation of APPs into oncology practices is associated with improved physician and patient satisfaction as well as overall practice productivity.20-22 The emergence of the COVID-19 pandemic has exacerbated burnout among medical oncologists worldwide.23
Recent years have seen a rising emphasis on physician productivity in the clinical practice of hematology and oncology.24 APPs have been increasingly incorporated into both academic and community-based hematology and oncology practices as fellowships providing hematology (and oncology)-focused training for APPs have been created to augment the APP workforce.25,26 Few prior studies have explored in depth the impact of physician compensation or APP support on physician burnout or satisfaction, particularly among hematologists and oncologists; no studies have examined burnout specifically in practicing hematologists. In 2019, ASH (American Society of Hematology), together with the Fitzhugh Mullan Institute for Health Workforce Equity at GW (George Washington University), designed a survey to examine the practice patterns and experiences of practicing adult hematologists and oncologists with a specific focus on the potential impact of compensation models and APP utilization on physician well-being. Here, we report on practice characteristics, burnout, and satisfaction among academic and community hematologists and oncologists before the COVID-19 pandemic.
Methods
Survey development, study design, and participants
The Survey of Practicing Hematologists & Oncologists was developed by members of the Fitzhugh Mullan Institute for Health Workforce Equity at GW (L.E.M and C.E.) in collaboration with the ASH Recruitment and Retention Working Group (N.T.C., L.M.D.C., G.A.D., J.F., M.H., A.I.L., A.L.M., R.P.N., M.N., C.L.O., A.R., R.J.R., D.S., M.S., and L.D.W.). The survey included 27 multiple-choice and open-ended questions assessing the following domains: practice activities, practice satisfaction, participation in medical education and mentoring, compensation, practice setting, and practitioner demographics; individual survey questions included in this analysis are shown in the supplemental Figures, with specific study measures described below. We pilot-tested the survey with 14 attending physicians representing a mixture of academic and community practices. The final survey was distributed by mail (with an online response option) to a random sample of 2500 physicians listed in the AMA Masterfile as adult hematologists or oncologists. The survey was administered from May to July 2019 by the Healthforce Center at UCSF (University of California, San Francisco) using the Dillman method, consisting of a prenotification letter, initial survey mailing, and up to 4 follow-up notifications to nonrespondents.27 All survey respondents received a $10 Amazon gift card and were also entered in a random drawing for 1 of 4 $500 Amazon gift cards. All survey-related correspondence and the survey instrument itself were cobranded with ASH and UCSF logos. UCSF staff members entered and cleaned the survey data; all data analysis was conducted by GW team members. The study was reviewed and approved by the GW Office of Human Research and the UCSF Institutional Review Board and conducted according to the Declaration of Helsinki.
Study measures
Burnout
Burnout was measured using a single-item instrument from the Physician Work–Life Study, which asked respondents to rate their level of burnout on a 5-category ordinal scale (supplemental Figure 1). This approach was previously demonstrated to have similar performance characteristics as the Maslach Burnout Inventory Emotional Exhaustion subscale.28-32 In our analyses, we defined “any burnout” as a score of ≥3, with ≥1 symptom of burnout such as physical or emotional exhaustion, while “high burnout” was defined as a score of ≥4.29
Satisfaction
To assess career satisfaction, we included a question asking respondents to rate their satisfaction with career development opportunities, relationship with senior leadership at their organization, salary/compensation, patient volume/panel size, work/life balance, and overall career satisfaction on a 5-point Likert scale (supplemental Figure 2). Response options ranged from “very satisfied” (1) to “very dissatisfied” (5). We defined responses of ≥4 in the domains of work/life balance and overall career as “dissatisfied with work/life balance” and “dissatisfied overall,” respectively.
Work hours and call
We examined continuous responses to questions in which respondents indicated their typical number of work hours per week or call obligations per year (supplemental Figure 3). We used these responses to generate 4 dichotomous variables indicating the top quartile of respondents for each variable: “high work hours” (≥60 hours per week), “high home work hours” (≥11 hours per week), “high weekday call” (≥90 weekdays per year), and “high weekend call” (≥13 weekends per year).
Advanced practice provider support
We measured the extent of survey respondent collaboration with APPs using a question asking how frequently APPs provided services in their practices (“never,” “rarely,” “occasionally,” “often,” “always”) across 7 types of tasks (conducting or assisting with new patient consults, conducting hospital rounds, managing their own patient panels, managing palliative care, ordering routine chemotherapy, performing invasive procedures, or taking night or weekend calls) (supplemental Figure 4). We used responses across all 7 domains to create a single dichotomous variable called “often work with APPs,” indicating that respondents worked with APPs “often” in ≥1 task.
E-consults and telemedicine
We gauged respondent use of e-consults and telemedicine tools using a question asking whether they currently used or planned to use 4 types of information technology in their practice (provider-to-provider communication tools, video visits, text messaging, e-mailing with patients, or remote patient monitoring) (supplemental Figure 5). We then created a single dichotomous variable called “any e-consults and telemedicine tools,” indicating the use of ≥1 telemedicine tool.
Mentoring and research activities
We measured involvement in mentoring with a question asking respondents whether they were involved in mentoring medical students, residents, or fellows in any of the domains of coaching/career advice, networking, or research projects (supplemental Figure 6).33 We collapsed responses across all trainee groups and domains to create a single dichotomous variable called “any mentoring,” indicating that a respondent was involved in ≥1 mentoring relationship or activity. We assessed research involvement with a question asking respondents to report their percentage of time devoted to different practice activities, including administration, patient care, research, teaching, or other activities (supplemental Figure 7); from these responses, we created a dichotomous variable called “any research,” indicating that respondents spent at least some of their time (ie, >0%) in research. We also included a question asking respondents whether they would recommend a career in benign hematology, malignant hematology, or solid tumor oncology to medical students or trainees (supplemental Figure 8).
Compensation
We identified compensation models using a survey question asking how respondents were compensated for their professional activities, with response options of salary, RVU, or other (supplemental Figure 9); respondents had the option of checking all that applied. We used these responses to create 2 dichotomous variables: “RVU-only compensation,” defined by the RVU option being checked and all others unchecked, and “RVU + salary compensation,” defined as both RVU and salary options checked and the “other” option unchecked. The survey also asked respondents with wholly or partially RVU-based compensation to indicate their agreement on a 5-point Likert scale with the statement “I am easily able to meet my RVU targets”; we used responses to this question to create a dichotomous variable indicating disagreement or strong disagreement (representing provider perceptions that they were unable to meet their RVU targets).
Control variables
We included several control variables in the model to account for respondent demographic characteristics and clinical focus, as reported by each respondent. Control variables included age (categorized as ≤40, 41 to 55, or ≥56 years based on generational definitions), years in current job (<10 years vs ≥10 years), gender, race/ethnicity (underrepresented in medicine vs not, as defined by National Institutes of Health standards to include Black or African American, Hispanic or Latino, American Indian or Alaska Native, and Native Hawaiian or other Pacific Islander), and clinical focus (majority benign hematology, majority malignant hematology, majority oncology, vs not, based on >50% of clinical time spent in the corresponding subspecialty focus).34,35
Statistical analysis
We calculated descriptive statistics for all study variables (mean and standard deviation for continuous variables, frequency distribution for categorical variables) using unweighted data. We conducted bivariate analyses using unweighted data to compare means of continuous variables (using 2-sample t tests) and distribution of categorical variables (using Fisher’s exact tests) between respondents in academic and community practice settings. We also compared rates of satisfaction and dissatisfaction among respondents who reported high burnout with those who did not.
We used weighted logistic regression models to explore associations between respondent job characteristics and their likelihood of reporting high levels of burnout, dissatisfaction with work/life balance, and overall career dissatisfaction (holding demographic characteristics and clinical focus constant) for respondents in academic and community practice settings. Models were weighted by age category to align with the age distribution of all survey invitation recipients as recorded in the AMA Masterfile. The null hypothesis for each association tested in the logistic regression analyses was that there was no association between each characteristic and the likelihood of the respondent reporting high levels of burnout or dissatisfaction, holding other variables in the model constant (adjusted odds ratio [OR], 1). We used P < .05 as the cutoff for statistical significance. We conducted all statistical analyses in Stata 15 (StataCorp LLC, College Station, TX).
Results
Provider demographics
A total of 631 hematologists and oncologists responded to the survey for an overall response rate of 25.2%, including 441 paper survey responses (68.9%) and 190 online responses (31.1%) (supplemental Figure 10). Among 411 respondents who reported providing hematology or oncology patient care in academic or community practice settings and had complete responses for inclusion in the regression models, 36.7% (n = 151) worked in academic practices and 63.3% (n = 260) in community practices (Table 1); 29.0% (n = 119) were female, with a higher female representation in community vs academic practices (32.3% vs 23.2%, respectively; P = .06). Only 5.8% (n = 24) of respondents indicated that they were underrepresented in medicine. More academic than community respondents reported a specific clinical focus in malignant (35.8% vs 3.5%, respectively) or benign (15.9% vs 6.2%, respectively) hematology (P < .01).
Bivariate analyses of practice characteristics, activities, and demographics by practice type
| . | Academic practice (n = 151) . | Community practice (n = 260) . | P value . |
|---|---|---|---|
| Work hr per wk, mean (SD) | |||
| Total work hr, excluding call and work at home | 52.4 (9.2) | 48.3 (11.5) | <.01 |
| Hr working at home | 10.4 (7.1) | 8.5 (9.0) | .02 |
| Number of calls per yr, mean (SD) | |||
| Weeknights | 51.8 (4.8) | 80.0 (4.8) | <.01 |
| Weekends | 7.8 (5.0) | 13.5 (10.7) | <.01 |
| Often work with APPs, n (%) | 112 (74.2) | 132 (50.8) | <.01 |
| Use of e-consults and/or telemedicine tools, n (%) | 117 (77.5) | 180 (69.2) | .09 |
| Mentoring of students or trainees, n (%) | |||
| Any mentoring | 143 (94.7) | 98 (37.7) | <.01 |
| Coaching/career advice | 135 (89.4) | 83 (32.6) | <.01 |
| Networking | 102 (71.3) | 45 (18.4) | <.01 |
| Research projects | 129 (86.6) | 40 (16.2) | <.01 |
| Research, n (%) | |||
| Any research | 137 (90.7) | 94 (36.2) | <.01 |
| Compensation models, n (%) | <.01 | ||
| RVU-only | 12 (8.0) | 79 (30.4) | |
| Salary-only | 77 (51.0) | 93 (35.7) | |
| RVU + salary | 49 (32.5) | 51 (19.6) | |
| Other | 13 (8.6) | 37 (14.2) | |
| Sex, n (%) | .06 | ||
| Female | 35 (23.2) | 84 (32.3) | |
| Male | 116 (76.8) | 176 (67.7) | |
| Age (yr), n (%) | .02 | ||
| ≤40 | 41 (27.2) | 43 (16.5) | |
| 41-55 | 60 (39.7) | 131 (50.4) | |
| ≥56 | 50 (33.1) | 86 (33.1) | |
| Yr in current job, n (%) | .41 | ||
| <10 | 76 (50.3) | 119 (45.7) | |
| ≥10 | 75 (49.7) | 141 (54.3) | |
| Race/ethnicity, n (%) | .28 | ||
| Underrepresented in medicine | 6 (4.0) | 18 (6.9) | |
| Not underrepresented | 145 (96.0) | 242 (93.1) | |
| Clinical focus, n (%) | <.01 | ||
| Benign hematology | 24 (15.9) | 16 (6.2) | |
| Malignant hematology | 54 (35.8) | 9 (3.5) | |
| Solid tumor oncology | 57 (37.8) | 110 (42.3) | |
| Combination or other | 16 (6.4) | 125 (48.1) |
| . | Academic practice (n = 151) . | Community practice (n = 260) . | P value . |
|---|---|---|---|
| Work hr per wk, mean (SD) | |||
| Total work hr, excluding call and work at home | 52.4 (9.2) | 48.3 (11.5) | <.01 |
| Hr working at home | 10.4 (7.1) | 8.5 (9.0) | .02 |
| Number of calls per yr, mean (SD) | |||
| Weeknights | 51.8 (4.8) | 80.0 (4.8) | <.01 |
| Weekends | 7.8 (5.0) | 13.5 (10.7) | <.01 |
| Often work with APPs, n (%) | 112 (74.2) | 132 (50.8) | <.01 |
| Use of e-consults and/or telemedicine tools, n (%) | 117 (77.5) | 180 (69.2) | .09 |
| Mentoring of students or trainees, n (%) | |||
| Any mentoring | 143 (94.7) | 98 (37.7) | <.01 |
| Coaching/career advice | 135 (89.4) | 83 (32.6) | <.01 |
| Networking | 102 (71.3) | 45 (18.4) | <.01 |
| Research projects | 129 (86.6) | 40 (16.2) | <.01 |
| Research, n (%) | |||
| Any research | 137 (90.7) | 94 (36.2) | <.01 |
| Compensation models, n (%) | <.01 | ||
| RVU-only | 12 (8.0) | 79 (30.4) | |
| Salary-only | 77 (51.0) | 93 (35.7) | |
| RVU + salary | 49 (32.5) | 51 (19.6) | |
| Other | 13 (8.6) | 37 (14.2) | |
| Sex, n (%) | .06 | ||
| Female | 35 (23.2) | 84 (32.3) | |
| Male | 116 (76.8) | 176 (67.7) | |
| Age (yr), n (%) | .02 | ||
| ≤40 | 41 (27.2) | 43 (16.5) | |
| 41-55 | 60 (39.7) | 131 (50.4) | |
| ≥56 | 50 (33.1) | 86 (33.1) | |
| Yr in current job, n (%) | .41 | ||
| <10 | 76 (50.3) | 119 (45.7) | |
| ≥10 | 75 (49.7) | 141 (54.3) | |
| Race/ethnicity, n (%) | .28 | ||
| Underrepresented in medicine | 6 (4.0) | 18 (6.9) | |
| Not underrepresented | 145 (96.0) | 242 (93.1) | |
| Clinical focus, n (%) | <.01 | ||
| Benign hematology | 24 (15.9) | 16 (6.2) | |
| Malignant hematology | 54 (35.8) | 9 (3.5) | |
| Solid tumor oncology | 57 (37.8) | 110 (42.3) | |
| Combination or other | 16 (6.4) | 125 (48.1) |
SD, standard deviation.
Among compensation models, “Other” includes compensation arrangements other than “RVU-only,” “Salary-only,” or “RVU + salary,” such as profit sharing and shareholder agreements, bonuses, medical director stipends, and grants.
The demographic data for survey respondents with complete responses were comparable to those for the entire cohort of survey respondents (respondents with complete responses vs entire cohort: female gender, 29.0% vs 28.8%; underrepresented in medicine, 5.8% vs 6.3%; clinical focus in benign hematology, 9.7% vs 9.6%; clinical focus in malignant hematology, 15.3% vs 14.6%; solid tumor oncology: 40.6% vs 40.6%, respectively). Additionally, the age distribution of survey respondents with complete responses was also comparable to the AMA Masterfile (respondents with complete responses vs AMA Masterfile: age ≤40 years, 20.4% vs 19.8%; age 41 to 55 years, 46.5% vs 42.7%; age ≥56 years, 33.1% vs 37.5%, respectively).
Provider activities, work hours, and compensation
Almost all respondents in academic practices (94.7%; n = 143) were involved in some form of mentoring of medical students or trainees, compared with 37.7% (n = 98) of community physicians (P < .01). Respondents from academic practices reported slightly higher mean work hours and hours worked at home than those from community practices, while community providers reported higher mean numbers of weekend and night calls (Table 1). Among all survey respondents, 22.1% (n = 91) were paid by an RVU-only compensation plan, while 24.3% (n = 100) were paid according to a mixture of an RVU-based compensation plan and salary; 12.2% (n = 50) reported having other compensation arrangements such as profit sharing and shareholder agreements, bonuses, medical director stipends, and grants. Respondents in community practices were significantly more likely than those in academic practices to report having RVU-only compensation (30.4% vs 8.0%), while those in academic practice were more likely to report salary-only compensation (51.0% vs 35.7%) (P < .01). Among respondents with wholly or partially RVU-based compensation, there was no significant difference in the inability to meet RVU targets according to practice setting (academic practices, 18.3%; community practices, 16.6%; P = .75).
Clinical support and telemedicine
Respondents in academic practices were significantly more likely than those in community practices to report often working with APPs on ≥1 task (Table 2). Hospital rounds and procedures were the most common activities performed by APPs; community practice respondents were significantly less likely to report working often with APPs on all of the activities queried in the survey. The majority of respondents (72.3%) in both academic and community practice used at least 1 form of telemedicine before the COVID-19 pandemic.
Advanced practice provider activities conducted often, according to practice type
| . | Academic practice (n = 151), n (%) . | Community practice (n = 260), n (%) . | P value . |
|---|---|---|---|
| Often work with APPs, by type of activity | |||
| New patient consultations | 37 (24.5) | 24 (9.2) | <.01 |
| Hospital rounds | 69 (45.7) | 63 (24.2) | <.01 |
| Manage own patient panel | 49 (32.5) | 29 (11.2) | <.01 |
| Manage palliative care | 39 (25.8) | 41 (15.8) | .01 |
| Order chemotherapy | 35 (23.2) | 42 (16.2) | .09 |
| Perform invasive procedures (eg, bone marrow biopsies, lumbar punctures) | 59 (39.1) | 46 (17.7) | <.01 |
| Take night or weekend call | 18 (11.9) | 21 (8.4) | .22 |
| . | Academic practice (n = 151), n (%) . | Community practice (n = 260), n (%) . | P value . |
|---|---|---|---|
| Often work with APPs, by type of activity | |||
| New patient consultations | 37 (24.5) | 24 (9.2) | <.01 |
| Hospital rounds | 69 (45.7) | 63 (24.2) | <.01 |
| Manage own patient panel | 49 (32.5) | 29 (11.2) | <.01 |
| Manage palliative care | 39 (25.8) | 41 (15.8) | .01 |
| Order chemotherapy | 35 (23.2) | 42 (16.2) | .09 |
| Perform invasive procedures (eg, bone marrow biopsies, lumbar punctures) | 59 (39.1) | 46 (17.7) | <.01 |
| Take night or weekend call | 18 (11.9) | 21 (8.4) | .22 |
Physician burnout and career satisfaction
Over one-third of respondents with complete survey data (36.5%; n = 150) reported having burnout as measured using the single-item Physician Work–Life Study question (Table 3); 12.2% (n = 50) had high burnout, defined by a burnout score ≥4, with 7.8% (n = 32) having symptoms of burnout that would not go away, and 4.4% (n = 18) feeling completely burned out to the point that they felt they may need to seek professional help. By comparison, among total survey respondents, 32.7% (n = 185) had burnout and 9.9% (n = 56) high burnout. The rates of overall burnout or high burnout among respondents with complete data did not differ significantly between respondents in academic vs community practices (overall burnout, 35.1% vs 37.3%, respectively; high burnout, 7.3% vs 13.8%, respectively; P = .59).
Burnout and career satisfaction according to practice type
| . | Academic practice (n = 151), n (%) . | Community practice (n = 260), n (%) . | P value . |
|---|---|---|---|
| Physician Work–Life Study burnout score | .59 | ||
| 1 (no burnout) | 25 (16.6) | 35 (13.5) | |
| 2 (no burnout) | 73 (48.3) | 128 (49.2) | |
| 3 (burnout) | 39 (25.8) | 61 (23.5) | |
| 4 (high burnout) | 10 (6.6) | 22 (8.5) | |
| 5 (high burnout) | 4 (2.7) | 14 (5.4) | |
| Satisfaction | |||
| Career development opportunities | 97 (64.2) | 134 (51.7) | .02 |
| Relationship with senior leadership | 95 (62.9) | 138 (53.3) | .06 |
| Salary/compensation | 78 (51.7) | 158 (61.0) | .08 |
| Patient volume | 79 (52.7) | 130 (50.4) | .68 |
| Work/life balance | 63 (41.7) | 104 (40.2) | .76 |
| Overall career satisfaction | 104 (68.9) | 167 (64.5) | .39 |
| . | Academic practice (n = 151), n (%) . | Community practice (n = 260), n (%) . | P value . |
|---|---|---|---|
| Physician Work–Life Study burnout score | .59 | ||
| 1 (no burnout) | 25 (16.6) | 35 (13.5) | |
| 2 (no burnout) | 73 (48.3) | 128 (49.2) | |
| 3 (burnout) | 39 (25.8) | 61 (23.5) | |
| 4 (high burnout) | 10 (6.6) | 22 (8.5) | |
| 5 (high burnout) | 4 (2.7) | 14 (5.4) | |
| Satisfaction | |||
| Career development opportunities | 97 (64.2) | 134 (51.7) | .02 |
| Relationship with senior leadership | 95 (62.9) | 138 (53.3) | .06 |
| Salary/compensation | 78 (51.7) | 158 (61.0) | .08 |
| Patient volume | 79 (52.7) | 130 (50.4) | .68 |
| Work/life balance | 63 (41.7) | 104 (40.2) | .76 |
| Overall career satisfaction | 104 (68.9) | 167 (64.5) | .39 |
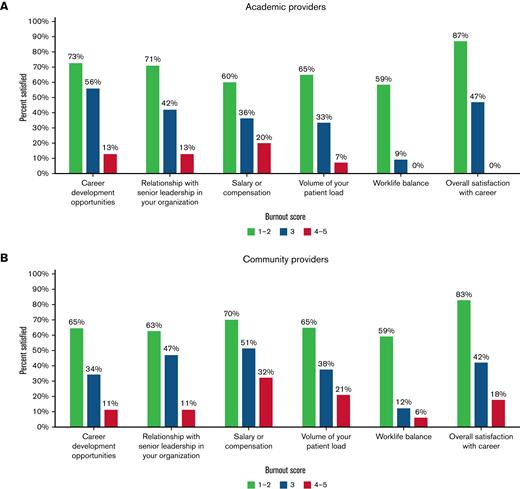
To explore provider perspectives that might contribute to burnout, we measured several markers of career satisfaction, which were generally associated with high burnout, although the extent of association differed for each satisfaction marker examined (Figure 1; supplemental File). Respondents from both academic and community practices who had high burnout reported higher dissatisfaction in all career domains (P < .01 for all comparisons), but key differences were noted between the 2 physician groups. A greater percentage of academic than community practice physicians were satisfied with overall career development opportunities, while a greater percentage of community practice physicians than academic physicians were satisfied with their compensation. Work/life balance had the lowest percentage of satisfaction among respondents from both academic and community practices, with less than half of all respondents being satisfied. No respondents from academic practices who had high burnout were satisfied with either their work/life balance or their overall career.
Markers of career satisfaction and high burnout. Shown are percentages of survey respondents who were satisfied in 6 different career dimensions as a function of burnout score using the single-question Physician Work–Life Study burnout measure. In this analysis, all respondents who answered questions on burnout and satisfaction were included. (A) Academic providers. (B) Community providers.
Markers of career satisfaction and high burnout. Shown are percentages of survey respondents who were satisfied in 6 different career dimensions as a function of burnout score using the single-question Physician Work–Life Study burnout measure. In this analysis, all respondents who answered questions on burnout and satisfaction were included. (A) Academic providers. (B) Community providers.
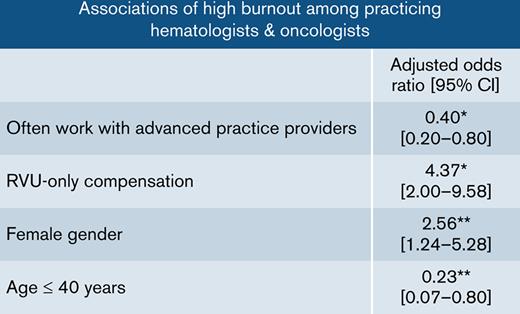
In weighted multivariate logistic regression models, RVU-only compensation and female gender were positively associated with high burnout, while often working with APPs and age <40 years were inversely associated with high burnout (Table 4). In models examining respondents from academic and community practices separately, RVU-only compensation was significantly associated with high burnout among respondents in both academic (adjusted OR, 11.09; 95% confidence interval [CI], 1.73-71.12; P = .01) and community (OR, 3.00; 95% CI, 1.14-7.90; P = .03) practices, with the association being particularly strong for academic providers (Table 5). Combined RVU + salary compensation was not significantly associated with high burnout among respondents from either academic (OR, 0.51; 95% CI 0.13-2.11; P = .35) or community (OR, 1.43; 95% CI 0.45-4.50; P = .54) practices. Among academic physicians, being female was significantly associated with high burnout (OR, 6.84; 95% CI 1.79-26.15; P < .01). Among community practice physicians, often working with APPs (OR, 0.28; 95% CI 0.12-0.65; P < .01) and age <40 years (OR, 0.10; 95% CI, 0.01-0.69; P = .02) were each inversely and independently associated with high burnout.
Weighted logistic regression models of associations with high burnout
| . | Total respondents (n = 411), adjusted OR (95% CI) . |
|---|---|
| Work hr per wk | |
| High work hr (top quartile) | 2.14 (0.68-6.73) |
| High work at home hr (top quartile) | 0.87 (0.40-1.87) |
| Calls per yr | |
| High weeknight call (top quartile) | 0.49 (0.15-1.62) |
| High weekend call (top quartile) | 0.99 (0.33-2.92) |
| Often work with APPs | 0.40∗ (0.20-0.80) |
| Use of e-consults and/or telemedicine tools | 1.83 (0.82-4.08) |
| Mentoring of students or trainees | |
| Any mentoring | 0.75 (0.33-1.69) |
| Research | |
| Any research | 0.52 (0.22-1.22) |
| Compensation models | |
| RVU-only | 4.37∗ (2.00-9.58) |
| RVU + salary | 1.06 (0.41-2.75) |
| Salary-only + other (reference) | — |
| Sex | |
| Female | 2.56† (1.24-5.28) |
| Age, yr | |
| ≤40 | 0.23† (0.07-0.80) |
| 41-55 (reference) | — |
| ≥56 | 0.69 (0.33-1.46) |
| Yr in current job | |
| ≥10 | 1.52 (0.71-3.30) |
| Race/ethnicity | |
| Underrepresented in medicine | 1.56 (0.34-7.07) |
| Clinical focus | |
| Benign hematology | 0.86 (0.23-3.22) |
| Malignant hematology | 0.82 (0.19-3.57) |
| Solid tumor oncology | 1.55 (0.70-3.43) |
| Combination or other (reference) | — |
| . | Total respondents (n = 411), adjusted OR (95% CI) . |
|---|---|
| Work hr per wk | |
| High work hr (top quartile) | 2.14 (0.68-6.73) |
| High work at home hr (top quartile) | 0.87 (0.40-1.87) |
| Calls per yr | |
| High weeknight call (top quartile) | 0.49 (0.15-1.62) |
| High weekend call (top quartile) | 0.99 (0.33-2.92) |
| Often work with APPs | 0.40∗ (0.20-0.80) |
| Use of e-consults and/or telemedicine tools | 1.83 (0.82-4.08) |
| Mentoring of students or trainees | |
| Any mentoring | 0.75 (0.33-1.69) |
| Research | |
| Any research | 0.52 (0.22-1.22) |
| Compensation models | |
| RVU-only | 4.37∗ (2.00-9.58) |
| RVU + salary | 1.06 (0.41-2.75) |
| Salary-only + other (reference) | — |
| Sex | |
| Female | 2.56† (1.24-5.28) |
| Age, yr | |
| ≤40 | 0.23† (0.07-0.80) |
| 41-55 (reference) | — |
| ≥56 | 0.69 (0.33-1.46) |
| Yr in current job | |
| ≥10 | 1.52 (0.71-3.30) |
| Race/ethnicity | |
| Underrepresented in medicine | 1.56 (0.34-7.07) |
| Clinical focus | |
| Benign hematology | 0.86 (0.23-3.22) |
| Malignant hematology | 0.82 (0.19-3.57) |
| Solid tumor oncology | 1.55 (0.70-3.43) |
| Combination or other (reference) | — |
The model in this analysis included all survey respondents with complete responses (n = 411).
P ≤ .01.
P < .05.
Weighted logistic regression models of associations of high burnout, according to practice type
| . | Academic practice (n = 151) adjusted OR (95% CI) . | Community practice (n = 260) adjusted OR (95% CI) . |
|---|---|---|
| Work hr per wk | ||
| High work hr (top quartile) | 1.91 (0.24-15.22) | 2.37 (0.52-10.71) |
| High work at home hr (top quartile) | 0.50 (0.11-2.26) | 1.21 (0.45-3.22) |
| Calls per yr | ||
| High weeknight call (top quartile) | 2.34 (0.24-22.79) | 0.45 (0.11-1.80) |
| High weekend call (top quartile) | 3.70 (0.28-49.53) | 0.86 (0.25-3.04) |
| Often work with APPs | 1.21 (0.18-8.12) | 0.28∗ (0.12-0.65) |
| Use of e-consults and/or telemedicine tools | 4.43 (0.16-122.84) | 1.74 (0.72-4.23) |
| Mentoring of students or trainees | ||
| Any mentoring | 1.34 (0.03-53.39) | 0.78 (0.32-1.90) |
| Research | ||
| Any research | 0.14 (0.01-2.02) | 0.74 (0.30-1.82) |
| Compensation models | ||
| RVU-only | 11.09† (1.73-71.12) | 3.00† (1.14-7.90) |
| RVU + salary | 0.51 (0.13-2.11) | 1.43 (0.45-4.50) |
| Salary-only + other (reference) | — | — |
| Sex | ||
| Female | 6.84∗ (1.79-26.15) | 2.07 (0.84-5.10) |
| Age, yr | ||
| ≤40 | 0.39 (0.03-4.62) | 0.10† (0.01-0.69) |
| 41-55 (reference) | — | — |
| ≥56 | 0.91 (0.09-9.20) | 0.62 (0.25-1.55) |
| Yr in current job | ||
| ≥10 | 2.32 (0.20-27.38) | 1.27 (0.51-3.18) |
| Race/ethnicity | ||
| Underrepresented in medicine | 10.70 (0.51-226.46) | 1.27 (0.23-6.95) |
| Clinical focus | ||
| Benign hematology | 2.46 (0.14-42.85) | 0.43 (0.03-0.48) |
| Malignant hematology | 1.13 (0.06-20.75) | 2.14 (0.27-16.84) |
| Solid tumor oncology | 4.44 (0.27-72.90] | 1.66 (0.70-3.94) |
| Combination or other (reference) | — | — |
| . | Academic practice (n = 151) adjusted OR (95% CI) . | Community practice (n = 260) adjusted OR (95% CI) . |
|---|---|---|
| Work hr per wk | ||
| High work hr (top quartile) | 1.91 (0.24-15.22) | 2.37 (0.52-10.71) |
| High work at home hr (top quartile) | 0.50 (0.11-2.26) | 1.21 (0.45-3.22) |
| Calls per yr | ||
| High weeknight call (top quartile) | 2.34 (0.24-22.79) | 0.45 (0.11-1.80) |
| High weekend call (top quartile) | 3.70 (0.28-49.53) | 0.86 (0.25-3.04) |
| Often work with APPs | 1.21 (0.18-8.12) | 0.28∗ (0.12-0.65) |
| Use of e-consults and/or telemedicine tools | 4.43 (0.16-122.84) | 1.74 (0.72-4.23) |
| Mentoring of students or trainees | ||
| Any mentoring | 1.34 (0.03-53.39) | 0.78 (0.32-1.90) |
| Research | ||
| Any research | 0.14 (0.01-2.02) | 0.74 (0.30-1.82) |
| Compensation models | ||
| RVU-only | 11.09† (1.73-71.12) | 3.00† (1.14-7.90) |
| RVU + salary | 0.51 (0.13-2.11) | 1.43 (0.45-4.50) |
| Salary-only + other (reference) | — | — |
| Sex | ||
| Female | 6.84∗ (1.79-26.15) | 2.07 (0.84-5.10) |
| Age, yr | ||
| ≤40 | 0.39 (0.03-4.62) | 0.10† (0.01-0.69) |
| 41-55 (reference) | — | — |
| ≥56 | 0.91 (0.09-9.20) | 0.62 (0.25-1.55) |
| Yr in current job | ||
| ≥10 | 2.32 (0.20-27.38) | 1.27 (0.51-3.18) |
| Race/ethnicity | ||
| Underrepresented in medicine | 10.70 (0.51-226.46) | 1.27 (0.23-6.95) |
| Clinical focus | ||
| Benign hematology | 2.46 (0.14-42.85) | 0.43 (0.03-0.48) |
| Malignant hematology | 1.13 (0.06-20.75) | 2.14 (0.27-16.84) |
| Solid tumor oncology | 4.44 (0.27-72.90] | 1.66 (0.70-3.94) |
| Combination or other (reference) | — | — |
P < .05.
P < .01.
In models examining dissatisfaction, among respondents from academic practices, RVU-only compensation was significantly associated both with overall dissatisfaction (OR, 10.00; 95% CI, 1.65-60.69; P < .01) and with dissatisfaction with work/life balance (OR, 6.83; 95% CI, 1.21-38.58; P = .03) (Tables 6 and 7). Among academic respondents, combined RVU + salary compensation plans had an inverse association with work/life balance dissatisfaction compared with salary-only or other compensation models (OR, 0.38; 95% CI, 0.15-0.97; P = .04) (Table 7). Among community practice respondents, high overall work hours (OR, 5.12; 95% CI 1.91-13.72; P < .01) and high hours spent working at home (OR, 4.35; 95% CI, 2.13-8.88; P < .01) were each independently associated with dissatisfaction with work/life balance (Table 7). Age ≥56 years (vs 41 to 55 years) had an inverse association with work/life balance dissatisfaction among community practice providers (OR, 0.42; 95% CI, 0.22-0.81; P = .01), while age <40 approached statistical significance (OR, 0.41; 95% CI, 0.15-1.08; P = .07). Community practice providers who had worked in their current jobs for ≥10 years were also significantly more likely to report being dissatisfied with work/life balance (OR, 2.47; 95% CI, 1.20-5.05; P = .01).
Weighted logistic regression models of associations with overall career dissatisfaction, according to practice type
| . | Academic practice (n = 151) adjusted OR (95% CI) . | Community practice (n = 260) adjusted OR (95% CI) . |
|---|---|---|
| Work hr per wk | ||
| High work hr (top quartile) | 3.00 (0.76-11.79) | 1.29 (0.29-5.74) |
| High work at home hr (top quartile) | 0.86 (0.23-3.27) | 2.98∗ (1.20-7.44) |
| Calls per yr | ||
| High weeknight call (top quartile) | 0.62 (0.07-5.99) | 0.67 (0.21-2.12) |
| High weekend call (top quartile) | 3.03 (0.69-13.41) | 0.82 (0.27-2.54) |
| Often work with APPs | 1.31 (0.34-5.04) | 0.63 (0.27-1.47) |
| Use of e-consults and/or telemedicine tools | 1.44 (0.31-6.62) | 0.95 (0.42-2.17) |
| Mentoring of students or trainees | ||
| Any mentoring | 3.20 (0.05-202.40) | 0.95 (0.39-2.29) |
| Research | ||
| Any research | 0.49 (0.06-4.19) | 0.77 (0.31-1.96) |
| Compensation models | ||
| RVU-only | 10.00∗ (1.65-60.69) | 0.92 (0.37-2.33) |
| RVU + salary | 0.32 (0.08-1.27) | 1.35 (0.45-4.03) |
| Salary-only + other (reference) | — | — |
| Sex | ||
| Female | 0.87 (0.26-2.89) | 0.99 (0.40-2.44) |
| Age, yr | ||
| ≤40 | 2.93 (0.50-17.09) | 0.37 (0.08-1.63) |
| 41-55 (reference) | — | — |
| ≥56 | 1.61 (0.26-9.81) | 0.74 (0.29-1.88) |
| Yr in current job | ||
| ≥10 | 2.41 (0.35-16.78) | 2.14 (0.78-5.90) |
| Race/ethnicity | ||
| Underrepresented in medicine | 1.74 (0.05-59.34) | 0.75 (0.15-3.87) |
| Clinical focus | ||
| Benign hematology | 0.31 (0.03-3.20) | 1.47 (0.28-7.83) |
| Malignant hematology | 0.19 (0.02-1.98) | 0.95 (0.13-6.84) |
| Solid tumor oncology | 0.80 (0.08-7.83) | 0.97 (0.42-2.23) |
| Combination or other (reference) | — | — |
| . | Academic practice (n = 151) adjusted OR (95% CI) . | Community practice (n = 260) adjusted OR (95% CI) . |
|---|---|---|
| Work hr per wk | ||
| High work hr (top quartile) | 3.00 (0.76-11.79) | 1.29 (0.29-5.74) |
| High work at home hr (top quartile) | 0.86 (0.23-3.27) | 2.98∗ (1.20-7.44) |
| Calls per yr | ||
| High weeknight call (top quartile) | 0.62 (0.07-5.99) | 0.67 (0.21-2.12) |
| High weekend call (top quartile) | 3.03 (0.69-13.41) | 0.82 (0.27-2.54) |
| Often work with APPs | 1.31 (0.34-5.04) | 0.63 (0.27-1.47) |
| Use of e-consults and/or telemedicine tools | 1.44 (0.31-6.62) | 0.95 (0.42-2.17) |
| Mentoring of students or trainees | ||
| Any mentoring | 3.20 (0.05-202.40) | 0.95 (0.39-2.29) |
| Research | ||
| Any research | 0.49 (0.06-4.19) | 0.77 (0.31-1.96) |
| Compensation models | ||
| RVU-only | 10.00∗ (1.65-60.69) | 0.92 (0.37-2.33) |
| RVU + salary | 0.32 (0.08-1.27) | 1.35 (0.45-4.03) |
| Salary-only + other (reference) | — | — |
| Sex | ||
| Female | 0.87 (0.26-2.89) | 0.99 (0.40-2.44) |
| Age, yr | ||
| ≤40 | 2.93 (0.50-17.09) | 0.37 (0.08-1.63) |
| 41-55 (reference) | — | — |
| ≥56 | 1.61 (0.26-9.81) | 0.74 (0.29-1.88) |
| Yr in current job | ||
| ≥10 | 2.41 (0.35-16.78) | 2.14 (0.78-5.90) |
| Race/ethnicity | ||
| Underrepresented in medicine | 1.74 (0.05-59.34) | 0.75 (0.15-3.87) |
| Clinical focus | ||
| Benign hematology | 0.31 (0.03-3.20) | 1.47 (0.28-7.83) |
| Malignant hematology | 0.19 (0.02-1.98) | 0.95 (0.13-6.84) |
| Solid tumor oncology | 0.80 (0.08-7.83) | 0.97 (0.42-2.23) |
| Combination or other (reference) | — | — |
P < .05.
Weighted logistic regression models of associations with dissatisfaction with work–life balance, according to practice type
| . | Academic practice (n = 151) adjusted OR (95% CI) . | Community practice (n = 260) adjusted OR (95% CI) . |
|---|---|---|
| Work hr per wk | ||
| High work hr (top quartile) | 1.77 (0.47-6.67) | 5.12∗ (1.91-13.72) |
| High work at home hr (top quartile) | 1.23 (0.55-2.77) | 4.35∗ (2.13-8.88) |
| Calls per yr | ||
| High weeknight call (top quartile) | 1.48 (0.39-5.66) | 1.11 (0.52-2.38) |
| High weekend call (top quartile) | 0.53 (0.13-2.27) | 0.72 (0.31-1.65) |
| Often work with APPs | 1.30 (0.50-3.37) | 0.88 (0.48-1.59) |
| Use of e-consults and/or telemedicine tools | 1.52 (0.56-4.13) | 0.97 (0.51-1.82) |
| Mentoring of students or trainees | ||
| Any mentoring | 1.79 (0.17-18.92) | 0.79 (0.42-1.49) |
| Research | ||
| Any research | 1.66 (0.33-8.47) | 1.15 (0.59-2.23) |
| Compensation models | ||
| RVU-only | 6.83† (1.21-38.58) | 0.77 (0.39-1.52) |
| RVU + salary | 0.38† (0.15-0.97) | 0.61 (0.26-1.42) |
| Salary-only + other (reference) | — | — |
| Sex | ||
| Female | 1.29 (0.53-3.11) | 1.29 (0.66-2.51) |
| Age, yr | ||
| ≤40 | 1.87 (0.62-5.59) | 0.41 (0.15-1.08) |
| 41-55 (reference) | — | — |
| ≥56 | 0.80 (0.26-2.51) | 0.42∗ (0.22-0.81) |
| Yr in current job | ||
| ≥10 | 0.98 (0.29-3.27) | 2.47∗ (1.20-5.05) |
| Race/ethnicity | ||
| Underrepresented in medicine | 3.50 (0.71-17.31) | 0.75 (0.24-2.32) |
| Clinical focus | ||
| Benign hematology | 1.68 (0.35-8.04) | 0.53 (0.11-2.51) |
| Malignant hematology | 0.84 (0.17-4.12) | 1.02 (0.20-5.32) |
| Solid tumor oncology | 1.14 (0.24-5.50) | 0.79 (0.43-1.46) |
| Combination or other (reference) | — | — |
| . | Academic practice (n = 151) adjusted OR (95% CI) . | Community practice (n = 260) adjusted OR (95% CI) . |
|---|---|---|
| Work hr per wk | ||
| High work hr (top quartile) | 1.77 (0.47-6.67) | 5.12∗ (1.91-13.72) |
| High work at home hr (top quartile) | 1.23 (0.55-2.77) | 4.35∗ (2.13-8.88) |
| Calls per yr | ||
| High weeknight call (top quartile) | 1.48 (0.39-5.66) | 1.11 (0.52-2.38) |
| High weekend call (top quartile) | 0.53 (0.13-2.27) | 0.72 (0.31-1.65) |
| Often work with APPs | 1.30 (0.50-3.37) | 0.88 (0.48-1.59) |
| Use of e-consults and/or telemedicine tools | 1.52 (0.56-4.13) | 0.97 (0.51-1.82) |
| Mentoring of students or trainees | ||
| Any mentoring | 1.79 (0.17-18.92) | 0.79 (0.42-1.49) |
| Research | ||
| Any research | 1.66 (0.33-8.47) | 1.15 (0.59-2.23) |
| Compensation models | ||
| RVU-only | 6.83† (1.21-38.58) | 0.77 (0.39-1.52) |
| RVU + salary | 0.38† (0.15-0.97) | 0.61 (0.26-1.42) |
| Salary-only + other (reference) | — | — |
| Sex | ||
| Female | 1.29 (0.53-3.11) | 1.29 (0.66-2.51) |
| Age, yr | ||
| ≤40 | 1.87 (0.62-5.59) | 0.41 (0.15-1.08) |
| 41-55 (reference) | — | — |
| ≥56 | 0.80 (0.26-2.51) | 0.42∗ (0.22-0.81) |
| Yr in current job | ||
| ≥10 | 0.98 (0.29-3.27) | 2.47∗ (1.20-5.05) |
| Race/ethnicity | ||
| Underrepresented in medicine | 3.50 (0.71-17.31) | 0.75 (0.24-2.32) |
| Clinical focus | ||
| Benign hematology | 1.68 (0.35-8.04) | 0.53 (0.11-2.51) |
| Malignant hematology | 0.84 (0.17-4.12) | 1.02 (0.20-5.32) |
| Solid tumor oncology | 1.14 (0.24-5.50) | 0.79 (0.43-1.46) |
| Combination or other (reference) | — | — |
P ≤ .01.
P < .05.
Discussion
In this national survey of US hematologists and oncologists, we found that RVU-only compensation plans were associated with high levels of physician burnout in both academic and community settings and that the incorporation of APPs into clinical practice was inversely associated with high burnout among community-based physicians. The association between RVU-only compensation plans and high burnout was particularly strong in academic settings: among the small number of academic providers in our study with RVU-only compensation plans, such plans were a significant risk factor for dissatisfaction with work/life balance and overall career dissatisfaction, independent of work hours, call responsibilities, or APP support. Among community providers, one-third of whom reported having RVU-only compensation plans, such plans were also significantly associated with high burnout, with high work hours and hours worked at home being independent risk factors for dissatisfaction with work/life balance.
Our findings raise a concern about the state of wellness of the hematology/oncology workforce and suggest that compensation systems focused exclusively on clinical productivity in either academic or community practices may be exacerbating physician burnout at a time when increasing emphasis is being placed on physician productivity in the clinical practice of hematology and oncology. A 2012-2013 ASCO survey also reported an association of burnout with exclusively productivity-based compensation models in univariable analyses.3 Our study extends the earlier ASCO study findings by including both hematologists and oncologists, focusing specifically on physicians with the highest levels of burnout, and demonstrating a significant association of high burnout with productivity-only compensation plans among both academic and community practice physicians in multivariable analyses. While only a minority of academic physicians in our 2019 survey had RVU-only compensation plans, we wonder whether such plans, over time, may become more prevalent among academic providers, particularly as large academic institutions acquire clinical practices and new clinically-oriented faculty are given academic appointments. As such, the potential negative impact of RVU-only compensation models on academic physicians may be greater than what the small proportion of affected respondents in our survey might otherwise suggest.
It is possible that pressure to meet RVU targets at the expense of other individual physician goals may lead to dissatisfaction in numerous career domains, impairing productivity and further worsening burnout. In our survey, 18.3% of academic physicians and 16.6% of community providers with wholly or partially RVU-only compensation plans indicated that they could not meet their RVU targets, and other previous studies of the oncology workforce have reported negative effects of burnout on physician productivity.3,36,37 Importantly, in our study, compensation plans that included a mixture of RVU generation and salary did not demonstrate a significant association with high burnout. These findings suggest that the incorporation of metrics other than clinical productivity into physician compensation plans may be beneficial in fostering physician well-being and supporting the hematology/oncology workforce.9,38-40
Our study findings also imply that increased utilization of APPs in clinical practice may mitigate high burnout, specifically among community hematologists and oncologists. The potential impact of APPs on physician burnout has not been previously examined to our knowledge, although prior studies have reported positive effects of APPs on physician and patient satisfaction and overall productivity in medical oncology practices.20-22 Paradoxically, in our study, while academic physicians had greater utilization of APPs than community providers, such APP support did not significantly mitigate the risk of high burnout among academic providers. This may reflect intrinsic differences in the responsibilities of academic and community physicians, as academic providers in our survey spent much more of their time involved in mentoring and research, where APP support would likely have a lesser role.
In our analysis, we observed a number of differences in practice characteristics between academic and community hematologists and oncologists, which may underlie some of the distinctions in high burnout and satisfaction between these 2 physician groups. Academic physicians more often were specialized in their clinical focus, had greater involvement in research and in mentoring of students and trainees, and reported slightly higher work hours, while community physicians took more weeknight and weekend calls. Despite these differences, apart from APP utilization, none of these specific factors had any significant association with high burnout in our analysis, and overall burnout rates were similar between the 2 groups, in keeping with prior literature.3
In our study, female gender was an independent risk factor for high burnout among academic hematologists and oncologists, while younger age was a negative risk factor for high burnout in community providers, with both younger and older community physicians demonstrating inverse associations with dissatisfaction with work/life balance. An association of female gender with physician burnout has been reported in numerous prior studies in oncology and other fields of medicine, as women often report lower career satisfaction and lower satisfaction with work/life integration than men.3,10-13,41 The reasons for such gender differences are complex and may be related to factors such as practice setting, income, age, and relationship status, among others.10,11 In academic medicine, gender disparities in faculty promotion, compensation, and mentorship may also be at play.42 Our finding of a protective effect of younger age on high burnout in community hematology/oncology physicians stands in contrast to previous studies identifying young age as a predictor of burnout among oncologists.3,19 Some of this age discrepancy may be specialty-specific or reflect generational changes over time, as survey studies not limited to the oncology workforce have reported higher burnout rates among mid-career than younger age physicians.43,44 Further studies are needed to more fully explore the impact of gender and age on burnout and satisfaction among practicing hematologists and oncologists.
The overall rate of burnout of 36.5% in our study, as defined by a Physician Work–Life Study score of ≥3 (with “any burnout” represented by a score of ≥3 and “high burnout” by a score of ≥4), is similar to other recent survey studies of the oncology workforce in the United States. These burnout rates are lower than recent survey findings reporting ∼50% burnout rates in other internal medicine subspecialties such as critical care, rheumatology, and infectious disease, although comparative rates of high burnout are uncertain.10,45 Further studies of burnout rates among hematologists and oncologists in comparison with other fields, the differences in factors impacting burnout among distinct specialties, and the potential implications of burnout on job retention and retirement, are indicated in order to better identify specialty-specific solutions for addressing burnout.
Our study has several limitations. While the overall response rate for our survey was 25.2% (n = 631), a smaller number of respondents were active in clinical care (n = 525) with complete data for inclusion in the regression models (n = 411), which may limit the generalizability of some of our findings. However, our response rates were comparable to those reported in other previously published survey studies of physician burnout utilizing the AMA Masterfile.10,46 Our use of the validated single-item Physician Work–Life Study burnout question rather than the complete Maslach Burnout Inventory may have impacted our analysis, and it is possible that the participants most affected by burnout could have been either less or more inclined to respond to our survey because of burnout itself. Among practices that implement RVU-only compensation plans, it is possible that certain practice characteristics (eg, leadership style, practice oversight, or other patient support services) may have unique contributions to high burnout that were not explored in our analysis. We did not specifically examine the effect of electronic medical record use on burnout despite increasing evidence in the literature linking the two.5,6 We were similarly unable to examine any potential associations of a specific race and ethnicity categories on burnout or satisfaction as only a small number of survey respondents identified as underrepresented minorities. In addition, our study was conducted before the COVID-19 pandemic, so we are unable to comment on the impact of COVID-19 on burnout and satisfaction.
In summary, we performed a survey of US hematologists and oncologists in academic and community practices and found that RVU-only compensation plans were significantly associated with high burnout in both practice settings. We also found female gender to be independently associated with high burnout among academic physicians, and we observed an inverse association of APP utilization with high burnout among community physicians. We propose that the implementation of compensation models that rely less on RVU generation and more on alternate metrics for both academic and community physicians, an expansion of APPs in community hematology and oncology practices, and increased recognition and support for women in academic medicine may reduce burnout and dissatisfaction and support health and longevity among practicing hematologists and oncologists. Further studies are needed to explore these trends.
Authorship
Contribution: L.E.M. and C.E.E. performed the data analyses; A.I.L. and L.E.M. wrote the initial draft of the manuscript; L.M.D.C., A.L.M., N.T.C., G.A.D., J.F., M.H., T.L.L., R.P.N., M.N., C.L.O., A.R., R.J.R., D.S., M.S., and L.D.W. contributed to editing the manuscript; and all authors designed the study and interpreted the data.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Alfred Ian Lee, 333 Cedar St, Yale School of Medicine, New Haven, CT 06510; e-mail: alfred.lee@yale.edu.
References
Author notes
∗A.I.L. and L.E.M. contributed equally as first authors.
Data can be shared upon request by e-mailing the corresponding author, Alfred Ian Lee (alfred.lee@yale.edu).
The full-text version of this article contains a data supplement.