TO THE EDITOR:
On 18 October 2021, retired General Colin Powell died of complications from a COVID-19 infection at age 84 years despite receiving 2 messenger RNA vaccines for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). General Powell had a compromised immune system due to multiple myeloma. He represents the growing number of medically vulnerable Americans who have died of severe COVID-19 infection or remain at risk. In a world where new variants continue to circulate, the ability of vaccines to keep up remains uncertain. Our duty to protect our patients with compromised immune system illustrates an essential need for a continuous pandemic preparedness network to respond to current and future pandemics.
The SARS-CoV-2 virus disproportionately affected individuals with medical and social vulnerability, including those with cancer or other immune compromises such as HIV, solid organ transplantation, congenital immunodeficiency, and old age. COVID-19–infected patients with cancer die at significantly higher rates than those without COVID-19.1 Patients with compromised immune systems are less likely to mount an adequate response to infection, leading to viral evolution and some have speculated, the emergence of variants such as Omicron.
In his book “Uncontrolled Spread,” the former US Food and Drug Administration commissioner Scott Gottlieb advocated for a more robust public health and medical system to protect us from future pandemics.2 He argued that “mothballed” efforts that sit in readiness should be replaced by systems that operate continuously. We extend this to advocate for a research and clinical care network that is always operating but capable of repurposing to focus on new priorities during emergencies. The network we propose here would function as an early warning system and exist as an embedded component of our health care delivery system.
Our national surveillance systems are insufficient to provide well-characterized, longitudinal, patient-specific exposures and outcomes with enough population coverage for real-time and generalizable early detection of emerging concerns. A paucity of patient-generated data has hampered our understanding of post viral syndromes, such as postacute sequelae of SARS-CoV-2 infection. During the pandemic, there were wide variations across care delivery sites related to anticoagulants, preventive treatments, and disease-modifying therapies. However, care variations were difficult to track because of the lack of linkages of existing clinical data systems, leading to limitations in visualizing and analyzing data in real-time to change practice.
A pandemic preparedness network for the immunocompromised must overcome these limitations to effectively respond to emerging future pandemics. It would contain multidimensional, continuous clinical data for artificial intelligence algorithms to detect unusual patterns in morbidity and mortality. If a signal with sufficient sensitivity were generated, the network would obtain specimens for sequencing, collect patient-generated survey and sensor data, directly engage practitioners in real-time practice improvement, and facilitate prospective evidence generation to address emerging questions in a timely fashion. Given the outsized impact of the COVID-19 pandemic upon Black, Indigenous, and people of color populations, the network would need to have specific recruitment procedures developed and include of sites with adequate minority populations to ensure representativeness and generalizability.
The network would identify and characterize risk and develop risk-mitigation strategies for special populations. The following questions would be addressed in real-time: (1) which specific exposures, such as B-cell depleting therapies, put immunocompromised patients at highest risk? (2) Can we identify and learn from exemplary care delivery organizations that successfully promoted vaccination uptake among highly vulnerable patients?
The network would collect genomic viral sequencing data from subpopulations of patients for the linkage of these data to other data sources. Monitoring pathogen variant strains and evolution in the immunocompromised population would help with the rapid understanding of new outbreaks and modes of transmission. Programs would incorporate response to vaccinations and effectiveness of therapeutic antibodies and oral agents as variants change.
Engaging clinicians in collaborative practice improvement is another critical component for the network. The proposed network would maintain a siteless data and trial ecosystem in which clinicians could directly opt in as individual participants. Physicians would verify their patients’ data quality while focusing on clinical outcomes and the overall public good, restoring their sense of autonomy and purpose by directly addressing societal issues for patient benefit. Network-provided third-party apps interoperable with large electronic health record systems, through application programming interfaces, would streamline data curation by embedding structured data elements within network note templates, thus improving the clinical documentation experience and incorporating clinician education and decision support. This reconfiguration of the relationship between clinicians and health care data would accelerate the long-sought National Academies of Sciences, Engineering, and Medicine goal of a national learning health system.3
A final but critical function of the network would be to prioritize newer forms of prospective evidence generation, such as pragmatic studies built upon a real-world data infrastructure, with individual clinicians as the primary engagement targets. A major shortcoming of our response to the COVID-19 pandemic was the proliferation of suboptimally designed and executed clinical trials that did not generate clinically actionable data. During a pandemic, the network could guide its siteless, unified community of clinicians and patients to agree upon the highest priority clinical studies that individual clinicians would rapidly implement throughout the network.
In its quest for optimizing efficiency while respecting the rights of participants, the network would include simple electronic consents for a portion of the population providing individually identifiable data, including Patient Reported Outcomes (PROs), alongside the ability to use limited datasets with a waiver of consent from the broader population.
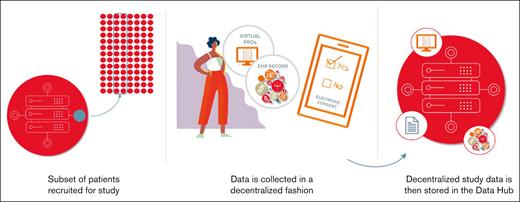
Gottlieb’s book2 also warns against preparing to fight the last war; a robust system would be able to detect the unexpected in a state of constant vigilance throughout a population of patients with compromised immune system, such as in cancer. The network would be developed as a public-private partnership with funding from multiple sources and benefits accrued to all. As primary data contributors, patients would be central stakeholders to help guide network activities and would need to be appropriately incentivized for their participation. Existing real-world evidence systems, such as the American Society of Hematology Research Collaborative could provide a foundation for building the proposed network. Current American Society of Hematology Research Collaborative projects include the development of a COVID-19 metric dashboard, and a decentralized study to examine real-world booster vaccine effectiveness in patients with multiple myeloma. The decentralized study (Figure 1) is an example of how a real-world data infrastructure can facilitate embedded prospective evidence generation studies that feed back to the network. The network could be extended to include other populations with immune compromises by sharing data across federal and nonfederal agencies working with these populations.
Decentralized study to examine COVID-19 vaccine booster effectiveness.
Currently, all surveillance systems that depend on real-world evidence suffer because of delays due to the time required for curation of data. To function with capabilities of an early warning system, the network must also seek ways to reduce the time required for data curation through the implementation of clinical data documentation templates and national data interoperability and standardization efforts. Tools such as ACE,4 mCODE,5 and OneSource6 are examples of how new technologies can efficiently improve data mining, documentation, and the point-of-care curation of electronic health record data.
As our national health care systems continue to deploy COVID-19 pandemic improvements, this proposed network should be considered part of the solution.7 New challenges from SARS-CoV-2 that threaten the immunocompromised and pose a risk to patients make clear that the need for this network is ongoing and not forgotten. Our patients with compromised immune system are at the epicenter of medical risk from pandemics and other emergencies; they deserve better than what we were able to provide for them this time around. A network that supports modernization efforts of our national biosurveillance capabilities and infectious disease data collection would provide an enduring rapid response data resource for the nation.
Contribution: W.A.W. designed and wrote the paper; and K.C.A., S.K.K., E.A.S., K.H., R.M.P., and G.P. provided critical edits and review and contributed meaningfully to the final draft.
Disclaimer: This article reflects the views of the authors and should not be construed to represent the views or policies of the Food and Drug Administration.
Conflict-of-interest disclosure: W.A.W. receives salary support from the American Society of Hematology (ASH) Research Collaborative. R.M.P. is an employee of ASH and has a supervisory role within the ASH Research Collaborative. K.H. and E.A.T. are employees of the ASH Research Collaborative. W.A.W., K.C.A., and S.K.K. have leadership positions in oversight groups or committees within the ASH Research Collaborative.
Correspondence: William A. Wood, Division of Hematology, Department of Medicine, University of North Carolina at Chapel Hill, Houpt Physician Office Bldg, Chapel Hill, NC 27599-7305; e-mail: wawood@med.unc.edu.