Key Points
Mosunetuzumab is active as a single agent and yields CRs in 24% of heavily pretreated patients with R/R DLBCL.
Step-up dosing mitigated CRS events with mosunetuzumab, which has a manageable tolerability profile in R/R DLBCL.
Abstract
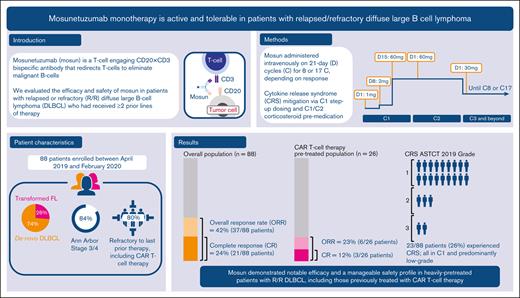
As part of a phase 1 or 2 study, this single-arm expansion cohort established the efficacy and safety of mosunetuzumab monotherapy in patients with relapsed/refractory (R/R) diffuse large B-cell lymphoma (DLBCL) (received ≥2 previous lines of therapy). Intravenous mosunetuzumab was administered with cycle (C) 1 step-up dosing for cytokine release syndrome (CRS) mitigation: C1 day (D) 1: 1 mg; C1D8 2 mg; C1D15 and C2D1: 60 mg; C3 + D1: 30 mg. Hospitalization was not mandatory. Patients with complete response (CR) completed treatment after C8; those with partial response or stable disease continued treatment for a total of 17 cycles. The primary end point was CR rate (best response), assessed against a historical control CR rate (20%) by independent review facility. Eighty-eight patients (73.9% de novo DLBCL; 26.1% transformed follicular lymphoma) were enrolled; all had received previous anthracycline and anti-CD20 therapy. Overall response and CR rates were 42.0% (95% confidence interval [CI], 31.6-53.1) and 23.9% (95% CI, 15.4-34.1), respectively; CR rate did not reach statistical significance vs the historical control (P = .36). Median time to first response was 1.4 months. Median progression-free survival was 3.2 months (95% CI, 2.2-5.3). The CR rate in 26 patients who received previous chimeric antigen receptor T-cell (CAR-T) therapy was 12%. CRS was one of the most common adverse events (26.1% of patients); predominantly grade 1 to 2 and primarily in C1. Four patients (4.5%) discontinued mosunetuzumab owing to adverse events. Mosunetuzumab demonstrated notable efficacy and a manageable safety profile in patients with R/R DLBCL, including those previously treated with CAR-Ts. This trial was registered at www.clinicaltrials.gov as #NCT02500407.
Introduction
Although ∼60% of patients with diffuse large B-cell lymphoma (DLBCL) may experience long-term survival after first-line immunochemotherapy with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP),1 ∼10% to 15% of patients are primary refractory to R-CHOP, and 20% to 25% experience relapse after an initial response.2
Salvage therapy with high-dose chemotherapy and autologous stem cell transplant (ASCT) has historically been the standard of care for patients with relapsed/refractory (R/R) DLBCL3-5; however, less than half of patients with R/R DLBCL will be suitable candidates for ASCT, and of those who are eligible, half will relapse after ASCT.6 Before the availability of anti-CD19 chimeric antigen receptor T-cell (CAR-T) therapy, survival outcomes for patients with R/R DLBCL who were unsuitable for second-line treatment with aggressive salvage chemotherapy and who had received at least 2 previous lines of therapy, were especially poor6-10; the SCHOLAR-1 study showed that the median overall survival (OS) duration for patients with refractory disease was 6.3 months from the start of salvage therapy.7 Furthermore, patients who were ineligible for a transplant had a median survival of 3.3 months.9
To address the need for more effective treatments, several classes of novel therapies have been developed and approved for R/R DLBCL after ≥2 lines of therapy. These include CD19-directed CAR-T therapies,11-13 the anti-CD79b antibody-drug conjugate polatuzumab vedotin in combination with bendamustine plus rituximab,14 the CD19-directed antibody-drug conjugate loncastuximab teserine,15 the oral exportin 1 inhibitor Selinexor,16 and the anti-CD19 monoclonal antibody tafasitamab in combination with lenalidomide (tafa-len).17 Furthermore, recent NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) indicate that tafa-len, as well as polatuzumab vedotin in combination with bendamustine plus rituximab, are among the preferred treatment options for patients with R/R DLBCL who are not candidates for ASCT.18 Ongoing studies are further exploring the use of approved therapies in the second-line treatment setting.
The development and approval of CAR-T therapies demonstrated the effectiveness of treatments that use T cells in the treatment of B-cell malignancies and represented a significant advance in the management of patients with R/R DLBCL. However, careful patient selection and extensive health care coordination are required with CAR-T therapies. Treatment may be complicated by the logistical challenges required to manufacture a patient-specific product and by restricted access to specialized treatment centers, as well as potential safety risks including high-grade cytokine release syndrome (CRS) and immune effector cell–associated neurotoxicity syndrome (ICANS).19 Therefore, a need remains for off-the-shelf therapies with durable remissions and improved tolerability. This is especially true for those patients with rapidly progressing disease who require immediate treatment and those of advanced age and/or with comorbidities, who may not tolerate intensive therapies.
Mosunetuzumab is a full-length, humanized immunoglobulin G1–based CD20×CD3 bispecific antibody that engages and redirects T cells to eliminate malignant B cells.20 It is being developed as a treatment option for R/R B-cell non-Hodgkin lymphomas as an off-the-shelf outpatient therapy and has been recently approved for the treatment of R/R follicular lymphoma in patients who have received ≥2 previous lines of therapy.
A phase 1 or 2 dose-escalation study of mosunetuzumab monotherapy in R/R B-cell lymphoma (ClinicalTrials.gov identifier: NCT02500407) recently demonstrated that mosunetuzumab has a promising risk-benefit profile and has the potential to address an unmet need for an effective and less toxic treatment option for R/R B-cell lymphoma.21 Administration of mosunetuzumab by cycle 1 step-up dosing provided effective mitigation of CRS and achieved durable complete responses (CRs) with a manageable safety profile; this was also demonstrated in those patients who had previously received CAR-T therapy.
On the basis of this dose-escalation study, a single-arm expansion cohort of patients with R/R DLBCL (including patients with transformed follicular lymphoma [trFL]) who had received ≥2 previous lines of therapy was enrolled to establish the efficacy and safety of fixed-duration intravenous mosunetuzumab in this patient population. Here, we report results from the primary analysis of this cohort.
Methods
Patients
Patients with DLBCL (including patients with trFL and high-grade B-cell lymphoma) were ≥18 years old and had an Eastern Cooperative Oncology Group performance status of 0 to 1. All patients were R/R to ≥2 previous lines of treatment, including an anti-CD20 monoclonal antibody and anthracycline. A baseline biopsy was required between the last dose of last prior anticancer therapy and the first dose of mosunetuzumab, if there was an accessible lesion. Patients considered eligible for an ASCT were excluded. Full details of the inclusion and exclusion criteria are presented in the supplemental Appendix.
Study design
This was a single-arm expansion cohort of the open-label phase 1 or 2 study. Patients received intravenous mosunetuzumab at the recommended phase 2 dose in 21-day cycles with cycle 1 step-up dosing to mitigate CRS as follows: cycle 1 day (D) 1: 1 mg; cycle 1 D8: 2 mg; cycle 1 D15 and cycle 2 D1: 60 mg each; cycle 3 D1 and beyond: 30 mg. Hospitalization was not mandatory for mosunetuzumab administration. Corticosteroid premedication (dexamethasone 20 mg or methylprednisolone 80 mg) was given intravenously 1-hour before each mosunetuzumab dose in cycle 1 and cycle 2 and was optional from cycle 3 onwards, unless the patient experienced a CRS event in the prior cycle. Patients who achieved a CR by cycle 8 completed treatment. Those who achieved a partial response (PR) or stable disease continued treatment for a total of 17 cycles, unless disease progression or unacceptable toxicity occurred.
All enrolled patients provided written informed consent. The protocol was approved by institutional review boards at each center and the trial was conducted in accordance with the Declaration of Helsinki, International Conference on Harmonisation Guidelines for Good Clinical Practice, and appropriate laws and regulations.
Study end points
The primary efficacy end point was independent review facility (IRF)–assessed CR (as best response) rate in all enrolled patients (efficacy-evaluable population). Patients with missing or no response assessments were classified as nonresponders. The safety and tolerability of mosunetuzumab was assessed by frequency, nature, and severity of adverse events (AEs) in all exposed patients (safety-evaluable population).
Secondary efficacy end points included CR rate assessed by investigators (INV), objective response rate (ORR; CR or PR) in all patients, ORR and CR rate in prespecified patient subgroups, duration of response (defined as time from initial occurrence of PR or CR until progressive disease or death) in all responders and in patients who achieved CR, duration of CR (defined as time from initial CR until progressive disease or death), in patients who achieved CR, progression-free survival (PFS; defined as time from first dose of study treatment to first occurrence of progressive disease or death), and OS (defined as time from first dose of study treatment to death) in all patients.
Assessments
Tumor assessments with computed tomography (CT) and positron emission tomography (PET)–CT scans were required at screening and during treatment; CT with or without PET was performed during posttreatment follow-up. Assessments were scheduled at 3 months and 6 months after the first mosunetuzumab dose, then every 3 months during the first 18 months on study, at 24 months, and then every 12 months thereafter. An early assessment at 6 weeks after the first mosunetuzumab dose was optional and these were included as part of the response rate assessment. Response was assessed by IRF- and INV-assessment of CT and PET-CT scans using standard response criteria.22 A repeat bone marrow assessment was required to confirm a CR in patients with trFL whose bone marrow was involved with lymphoma at baseline.
AEs were reported using the National Cancer Institute Common Terminology Criteria for Adverse Events, version 4.0. (CTCAE 2009). CRS grading was reported using American Society for Transplantation and Cellular Therapy (ASTCT) criteria.23
CD20 expression was retrospectively evaluated centrally by immunohistochemistry to determine its potential association with response. Tumor biopsies for baseline biomarker evaluation were collected as archival or fresh specimens at screening, which was required to be between the last dose of last prior anticancer therapy and the first dose of mosunetuzumab, if there was an accessible lesion. The biomarker-evaluable population comprised those patients with an available biopsy sample. The association of response with cell-of-origin prevalence (germinal center B-cell like [GCB] vs non-GCB), and double or triple-hit lymphoma status (MYC and BCL2 and/or BCL6) was also explored. Further details of these biomarker analyses are provided in the supplemental Appendix.
Statistical analysis
The CR rate was estimated, along with the Clopper-Pearson exact 95% confidence intervals (CIs). Comparisons of CR between the efficacy-evaluable population and historical controls were conducted using an exact binomial test with 2-sided α level of 5%. The historical control CR rate was assumed to be 20%, based on a meta-analysis of studies that enrolled a majority of patients with R/R DLBCL who had received ≥2 previous systemic therapies. Approximately 80 patients were planned to be enrolled during the R/R DLBCL or trFL expansion phase. This would provide an 85% power to detect a 15% increase in the CR rate from 20% to 35%, at the 5% 2-sided significance level. Further details of the historical control and sample size calculation are provided in the supplemental Statistical Analysis Plan.
The primary efficacy analysis was planned for at least 6 months after the last patient was enrolled into the phase 2 expansion cohort. The clinical cutoff date for this analysis was 15 March 2021.
Results
Patients
A total of 88 patients with R/R DLBCL were enrolled between April 2019 and February 2020. Sixty-five patients (73.9%) had de novo DLBCL, and 23 patients (26.1%) had trFL. Seventeen patients (19.3%) had double- or triple-hit lymphomas. The median age of patients was 66.5 years (range, 24-96), and they had received a median of 3 (range, 2-13) previous lines of therapy (Table 1). Twenty-six patients (29.5%) received prior treatment with CAR-T, and 15 patients (17.0%) had a history of ASCT. The majority of patients (79.5%) were refractory to their last prior therapy (defined as a lack of response during previous therapy or progressing within 6 months of the last treatment); 87.5% were refractory to any previous anti-CD20 therapy. In patients who received CAR-T therapy, 69.2% were refractory to previous CAR-T therapy. For 78 of 88 patients with cell-of-origin information available, 49 were classified as GCB and 29 as non-GCB by local assessment.
Baseline patient and disease characteristics in all patients (clinical cutoff date 15 March 2021; safety evaluable population)
| N (%) of patients unless stated . | N = 88 . |
|---|---|
| Median age, y (range) | 66.5 (24-96) |
| Male | 60 (68.2) |
| ECOG PS | |
| 0 | 31 (35.2) |
| 1 | 57 (64.8) |
| Ann Arbor stage | |
| I | 4 (4.5) |
| II | 10 (11.4) |
| III | 19 (21.6) |
| IV | 55 (62.5) |
| NHL subtype | |
| DLBCL | 65 (73.9) |
| trFL | 23 (26.1) |
| Cell-of-origin | |
| GCB | 49 (55.7) |
| Non-GCB | 29 (33.0) |
| Unknown | 10 (11.4) |
| MYC and BCL2 and/or BCL6 translocation | 17 (19.3) |
| Bulky disease (>10 cm) | 8 (9.1) |
| Median number of prior lines of therapy, n (range) | 3 (2-13) |
| 2 previous lines, n (%) | 31 (35.2) |
| 3 previous lines, n (%) | 28 (31.8) |
| >3 previous lines, n (%) | 29 (33.0) |
| Prior cancer therapy | |
| Anti-CD20 antibody | 88 (100.0) |
| Anthracycline | 88 (100.0) |
| CAR-T cell therapy | 26 (29.5) |
| Prior ASCT | 15 (17.0) |
| R/R∗status | |
| Refractory to last prior therapy | 70 (79.5) |
| Refractory to any previous anti-CD20 | 77 (87.5) |
| Refractory to previous CAR-T cell therapy | 18/26 (69.2) |
| N (%) of patients unless stated . | N = 88 . |
|---|---|
| Median age, y (range) | 66.5 (24-96) |
| Male | 60 (68.2) |
| ECOG PS | |
| 0 | 31 (35.2) |
| 1 | 57 (64.8) |
| Ann Arbor stage | |
| I | 4 (4.5) |
| II | 10 (11.4) |
| III | 19 (21.6) |
| IV | 55 (62.5) |
| NHL subtype | |
| DLBCL | 65 (73.9) |
| trFL | 23 (26.1) |
| Cell-of-origin | |
| GCB | 49 (55.7) |
| Non-GCB | 29 (33.0) |
| Unknown | 10 (11.4) |
| MYC and BCL2 and/or BCL6 translocation | 17 (19.3) |
| Bulky disease (>10 cm) | 8 (9.1) |
| Median number of prior lines of therapy, n (range) | 3 (2-13) |
| 2 previous lines, n (%) | 31 (35.2) |
| 3 previous lines, n (%) | 28 (31.8) |
| >3 previous lines, n (%) | 29 (33.0) |
| Prior cancer therapy | |
| Anti-CD20 antibody | 88 (100.0) |
| Anthracycline | 88 (100.0) |
| CAR-T cell therapy | 26 (29.5) |
| Prior ASCT | 15 (17.0) |
| R/R∗status | |
| Refractory to last prior therapy | 70 (79.5) |
| Refractory to any previous anti-CD20 | 77 (87.5) |
| Refractory to previous CAR-T cell therapy | 18/26 (69.2) |
ECOG PS, Eastern Cooperative Oncology Group performance status; NHL, non-Hodgkin lymphoma.
Defined as not achieving a response (complete or partial) or progressing within ≤6 months of applicable treatment.
Overall, the demographics were similar between patients who received previous CAR-T therapy and those who did not (supplemental Table 1). However, at baseline, patients with prior CAR-T therapy appeared to have a slightly worse Eastern Cooperative Oncology Group performance status and more advanced disease, previous therapies, and disease refractory to previous anti-CD20 therapies.
At the data cutoff date of 15 March 2021, the median time on study was 10.1 months (range, 0.1-22.3). Patients received a median of 4 mosunetuzumab treatment cycles (range, 1-17). Median relative dose intensity was 100%, and 84.1% received >90% dose intensity.
At the data cutoff date, 18 patients had completed initial treatment, and 70 patients had discontinued initial treatment prematurely (supplemental Figure 1). Reasons for premature discontinuation from treatment were progressive disease (60 patients), withdrawal by the participant (3 patients), physician decision (3 patients), AE, and death (2 patients each). Twenty-seven patients (30.7%) were in follow-up for response durability or survival, and 61 patients (69.3%) discontinued the study.
Efficacy
The IRF-assessed ORR was 42.0% (37/88 patients; 95% CI, 31.6-53.1). The IRF-assessed CR rate was 23.9% (21/88 patients; 95% CI, 15.4-34.1), which was numerically greater than the 20% historical control CR rate but did not reach statistical significance (P = .36). Results by INV assessment were highly concordant with those by IRF assessment (Table 2).
Efficacy summary in all exposed patients by IRF and INV
| . | By IRF . | By INV . |
|---|---|---|
| ORR∗, n (%) (95% CI) | 37 (42.0) (31.6-53.1) | 37 (42.0) (31.6-53.1) |
| CR rate∗, n (%) (95% CI) | 21 (23.9) (15.4-34.1) | 21 (23.9) (15.4-34.1) |
| Median time to first response, mo (range) | 1.4 (1.1-11.5) | 1.4 (1.1-8.9) |
| Duration of response | ||
| Median, mo (95% CI) | 7.0 (4.2-NE) | 6.9 (4.4-NE) |
| 12-mo event-free rate | 44.1% (27.3-60.9) | 43.2% (26.8-59.6) |
| Median time to first CR, mo (range) | 2.8 (1.1-17.5) | 3.0 (1.2-20.8) |
| Duration of CR | ||
| Median, mo (95% CI) | NE (9.0-NE) | NE (7.0-NE) |
| 12-mo event-free rate | 68.1% (46.9-89.3) | 72.0% (48.5-95.5) |
| Duration of response in complete responders | ||
| Median, mo (95% CI) | NE (9.0-NE) | NE (13.8-NE) |
| 12-mo event-free rate | 69.7% (49.3-90.1) | 79.0% (60.6-97.3) |
| PFS | ||
| Median, mo (95% CI) | 3.2 (2.2-5.3) | 2.7 (1.4-4.1) |
| 12-mo event-free rate | 22.6% (13.0-32.2) | 20.4% (11.6-29.2) |
| OS | ||
| Median, mo (95% CI) | 11.5 (9.0-16.4) | |
| 12-mo event-free rate | 48.1% (37.1-59.2) | |
| . | By IRF . | By INV . |
|---|---|---|
| ORR∗, n (%) (95% CI) | 37 (42.0) (31.6-53.1) | 37 (42.0) (31.6-53.1) |
| CR rate∗, n (%) (95% CI) | 21 (23.9) (15.4-34.1) | 21 (23.9) (15.4-34.1) |
| Median time to first response, mo (range) | 1.4 (1.1-11.5) | 1.4 (1.1-8.9) |
| Duration of response | ||
| Median, mo (95% CI) | 7.0 (4.2-NE) | 6.9 (4.4-NE) |
| 12-mo event-free rate | 44.1% (27.3-60.9) | 43.2% (26.8-59.6) |
| Median time to first CR, mo (range) | 2.8 (1.1-17.5) | 3.0 (1.2-20.8) |
| Duration of CR | ||
| Median, mo (95% CI) | NE (9.0-NE) | NE (7.0-NE) |
| 12-mo event-free rate | 68.1% (46.9-89.3) | 72.0% (48.5-95.5) |
| Duration of response in complete responders | ||
| Median, mo (95% CI) | NE (9.0-NE) | NE (13.8-NE) |
| 12-mo event-free rate | 69.7% (49.3-90.1) | 79.0% (60.6-97.3) |
| PFS | ||
| Median, mo (95% CI) | 3.2 (2.2-5.3) | 2.7 (1.4-4.1) |
| 12-mo event-free rate | 22.6% (13.0-32.2) | 20.4% (11.6-29.2) |
| OS | ||
| Median, mo (95% CI) | 11.5 (9.0-16.4) | |
| 12-mo event-free rate | 48.1% (37.1-59.2) | |
NE, not estimable.
Best response.
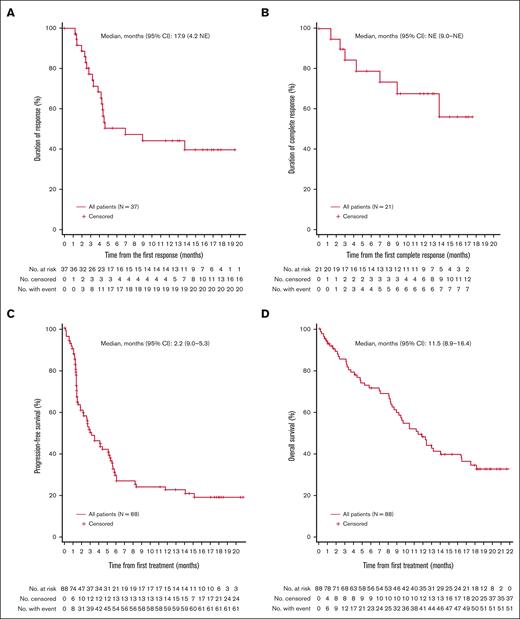
Median time to first response by IRF was 1.4 months (range, 1-12) and median time to first CR was 2.8 months (range, 1-17). Of the 37 patients who achieved a response (CR or PR) by IRF, the median duration of response was 7.0 months (95% CI, 4.2-not estimable). The Kaplan-Meier estimated event-free rate among responders at 12 months after the first response was 44.1% (95% CI, 27.3-60.9) (Figure 1A; data for complete responders is provided in Figure 1B). Of the 21 patients who achieved a CR, the median duration of response by IRF was not reached (95% CI, 9.0-not estimable). After an additional 5 months of follow-up (clinical cutoff date 27 August 2021), the median duration of response among responders by INV assessment was 6.9 months (95% CI, 4.4-not estimable).
Kaplan-Meier estimates. Kaplan-Meier plots of duration of response in responders (A), duration of CR in complete responders (B), PFS in all enrolled patients by IRF (C), and OS in all enrolled patients (D) are shown. NE, not estimable.
Kaplan-Meier estimates. Kaplan-Meier plots of duration of response in responders (A), duration of CR in complete responders (B), PFS in all enrolled patients by IRF (C), and OS in all enrolled patients (D) are shown. NE, not estimable.
With a median follow-up of 10.1 months, median PFS by IRF and OS were 3.2 months (95% CI, 2.2-5.3; Figure 1C) and 11.5 months (95% CI, 9.0-16.4; Figure 1D), respectively.
Prespecified subgroup analyses of ORR and CR rates demonstrated consistency of the treatment effect in relevant populations (supplemental Figure 2). CR rates observed in patients with GCB cell-of-origin (24%), trFL histology at study entry (26%), disease refractory to previous anti-CD20 therapies (21%), and patients aged ≥65 years (29%) were comparable with CR rates observed in the patient population overall. A higher ORR was observed in patients with trFL histology (61%) compared with those with de novo DLBCL (35%). Patients with double- or triple-hit lymphoma (n = 17) demonstrated an ORR (41%) that was comparable with the patient population overall, with a numerically lower CR rate (6%). The ORR and CR rates in the 26 patients who received previous CAR-T therapy were 23% and 12%, respectively. Median PFS in these patients was 1.4 months (95% CI, 1.3-5.3). Three patients with previous CAR T-cell therapy were free of a PFS event at 12 months.
Expression of CD20 by tumor cells was not required for study entry. A retrospective analysis of baseline CD20 expression levels by immunohistochemistry in the biomarker-evaluable population (54/88 patients; 39 with DLBCL and 15 with trFL) showed that responses were observed across a range of CD20 levels. The majority of these biopsies were collected <3 months before treatment (31/39 DLBCL biopsies and 10/15 trFL biopsies). Of these, 4 of 54 patients had CD20 expression on <50% of cells (1 patient <5%, 1 patient 7%, 2 patients 30%-35%) and failed to respond (supplemental Figure 3A). There was a general trend toward higher peripheral B-cell counts, but not for T-cell or natural killer cell counts at baseline and response; however, these differences may be driven by a few outliers (supplemental Figure 3B). Peripheral B-cell counts were depleted during treatment, but T-cell and natural killer cell counts remained unchanged from baseline (supplemental Figure 4).
Safety
Apart from fatal progression of lymphoma (18.2%), which was a reportable event per protocol, the most common AEs (≥20%) were neutropenia (27.3%), CRS (ASTCT 2019 criteria; 26.1%), fatigue (26.1%), rash (21.6%), hypophosphatemia and anemia (17.0% each), and diarrhea (15.9%) (Table 3; supplemental Table 2).
AE summary in all exposed patients
| N (%) of patients with ≥1 AE . | N = 88 . |
|---|---|
| Any AE | 84 (95.5) |
| Most common AEs (≥20%) | |
| Neutropenia∗ | 24 (27.3) |
| CRS† | 23 (26.1) |
| Fatigue | 23 (26.1) |
| Rash | 19 (21.6) |
| Any mosunetuzumab-related AE | 69 (78.4) |
| Any grade 3 to 4 AE | 51 (58.0) |
| Most common grade 3 to 4 AEs (≥5%) | |
| Neutropenia∗ | 19 (21.6) |
| Hypophosphatemia | 10 (11.4) |
| Anemia | 8 (9.1) |
| Febrile neutropenia | 5 (5.7) |
| Any mosunetuzumab-related grade 3 to 4 AE | 37 (42.0) |
| Any grade 5 AEs (not including PD)‡ | 3 (3.4) |
| Any mosunetuzumab-related grade 5 AE | 1 (1.1) |
| Any AE leading to discontinuation of mosunetuzumab | 4 (4.5) |
| Any mosunetuzumab-related AE leading to discontinuation of mosunetuzumab | 2 (2.3) |
| Any AE leading to mosunetuzumab dose modification | 1 (1.1) |
| Any AE leading to mosunetuzumab dose interruption | 22 (25.0) |
| N (%) of patients with ≥1 AE . | N = 88 . |
|---|---|
| Any AE | 84 (95.5) |
| Most common AEs (≥20%) | |
| Neutropenia∗ | 24 (27.3) |
| CRS† | 23 (26.1) |
| Fatigue | 23 (26.1) |
| Rash | 19 (21.6) |
| Any mosunetuzumab-related AE | 69 (78.4) |
| Any grade 3 to 4 AE | 51 (58.0) |
| Most common grade 3 to 4 AEs (≥5%) | |
| Neutropenia∗ | 19 (21.6) |
| Hypophosphatemia | 10 (11.4) |
| Anemia | 8 (9.1) |
| Febrile neutropenia | 5 (5.7) |
| Any mosunetuzumab-related grade 3 to 4 AE | 37 (42.0) |
| Any grade 5 AEs (not including PD)‡ | 3 (3.4) |
| Any mosunetuzumab-related grade 5 AE | 1 (1.1) |
| Any AE leading to discontinuation of mosunetuzumab | 4 (4.5) |
| Any mosunetuzumab-related AE leading to discontinuation of mosunetuzumab | 2 (2.3) |
| Any AE leading to mosunetuzumab dose modification | 1 (1.1) |
| Any AE leading to mosunetuzumab dose interruption | 22 (25.0) |
PD, progression of disease.
Includes events with term reported as neutropenia or neutrophil count decrease.
According to ASTCT 2019 grade.23
Pneumonia, sepsis and cholangitis (1 patient each).
The most common grade 3 to 4 AEs (>5%) were neutropenia (21.6%), hypophosphatemia (11.4%, all resolved and without clinically significant sequelae), anemia (9.1%), and febrile neutropenia (5.7%) (Table 3; supplemental Table 3). AEs leading to mosunetuzumab discontinuation were uncommon (4 patients; unrelated to mosunetuzumab: cholangitis [grade 5] and lung neoplasm malignant [grade 2]; related to mosunetuzumab: sepsis [grade 5] and myocardial infarction [grade 3]) (Table 3). AEs led to mosunetuzumab dose reduction in 1 patient and dose interruption in 22 patients (25.0%), regardless of causality; although a high dose intensity was achieved. Excluding fatal progression of lymphoma (16 patients), grade 5 AEs occurred in 3 patients (pneumonia [1 patient, related to mosunetuzumab], sepsis [1 patient, unrelated to mosunetuzumab], cholangitis [1 patient, unrelated to mosunetuzumab; grade 3 febrile neutropenia reported concurrently]). AE rates were comparable in patients aged ≤65 years and >65 years (supplemental Table 4).
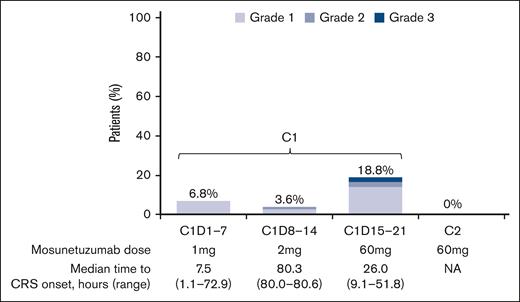
CRS (ASTCT 2019 criteria) was one of the most common AEs (23 patients [26.1%]) (Table 3). CRS was mostly low grade with 21 patients (23.9%) having CRS grade 1 or 2 (grade 1: 20.5%; grade 2: 3.4%). High-grade CRS was uncommon with only 2 patients (2.3%) experiencing grade 3 CRS. There were no grade 4 or 5 CRS events. CRS was confined to cycle 1 during step-up dosing, with the majority occurring with cycle 1 D15 dosing (15 events [grade 1, 11 events; grade 2, 2 events; grade 3, 2 events]; Figure 2), with a median time to CRS onset (cycle 1 D15) of 26.0 hours (range, 9.1-51.8). No CRS event occurred during cycle 2 or subsequent cycles. The most common symptoms of CRS were pyrexia (95.7% of patients), chills (30.4%), and hypotension (21.7%). Both patients with grade 3 CRS required hospitalization for CRS management, whereas 3 patients with grade 2 CRS and 9 patients with grade 1 CRS, were hospitalized for monitoring and management. In accordance with CRS management guidelines in the study protocol, 1 dose of tocilizumab was administered for CRS in 5 patients (3 grade 1, 1 grade 2, and 1 grade 3) and steroids were administered for CRS in 5 patients (4 grade 1 and 1 grade 3). An overview of CRS management by grade is provided (supplemental Table 5). Median duration of CRS events was 3 days (range, 1-19), and all CRS events were resolved.
Patients (%) with CRS events by cycle and grade. C, cycle; D, day; NA, not available.
Patients (%) with CRS events by cycle and grade. C, cycle; D, day; NA, not available.
Common (≥10%) hematological AEs were neutropenia (27.3% of patients) and anemia (17.0%). Neutropenia was mostly grade 3 (8.0%) or grade 4 (13.6%). Median time to first neutropenia onset was 40.5 days (range, 1-280) and median duration was 8 days (range, 2-173). Nineteen patients received granulocyte–colony stimulating factor treatment for neutropenia; 86.8% of neutropenia events had resolved by the data cutoff date. Overall, grade 3 or higher infections occurred in 12.5% of patients. Two patients had sepsis (1 grade 4 and 1 grade 5) concurrent with grade 4 events of neutropenia. Febrile neutropenia occurred in 5.7% of patients.
Tumor flare events, likely because of the influx of T cells into tumor sites, occurred in 3 patients with a median onset of 11 days (range, 7-84). One grade 2 tumor flare event (swelling and pain at tumor site) occurred in 1 patient. Two pleural effusion events occurred in 2 patients and were reported as suspected tumor flare events. No tumor lysis syndrome events occurred in this cohort of patients.
Neurological events, potentially consistent with ICANS assessed as related to study treatment, were uncommon (occurred in 2 patients), including confusional state (grade 1, 1.1%) and disturbance in attention (grade 1, 1.1%). Both events were resolved. There were no grade ≥3 mosunetuzumab–related neurological events and no cases of aphasia, seizures, encephalopathy, or cerebral edema. The AE profile of patients who had received prior CAR-T therapy is provided in supplemental Table 6.
Discussion
This dose-expansion cohort evaluated the efficacy and safety of mosunetuzumab monotherapy in patients with R/R DLBCL who had received ≥2 previous lines of therapy. The study included patients with R/R DLBCL or trFL who were heavily pretreated; most were refractory to previous anti-CD20 therapy (88%), 30% had received previous CAR-T therapy (most of whom were refractory to this treatment). The IRF-assessed ORR and CR rates were 42.0% and 23.9%, respectively. Approximately 70% of complete responders maintained complete remission at 12 months after the first response, although the duration of follow-up was limited. Comparable CR rates were observed in the subgroup of patients with non-GCB cell-of-origin (n = 28; 28%) and patients with GCB (n = 49; 24%). Comparable ORR but a lower CR rate was observed in patients with double- or triple-hit lymphomas (n = 17; ORR 41%, CR rate 6%). Although responses were observed across a range of CD20 levels, in the small number of patients with CD20 levels <35% (4 patients), responses to mosunetuzumab were not seen. This is consistent with the mechanism of action of mosunetuzumab and observations from studies with rituximab, a monoclonal anti-CD20 antibody, in patients with DLBCL.24,25 Consistent with the previous report on the dose-escalation experience,21 CRs were observed with mosunetuzumab in patients with prior CAR-T therapies albeit at a lower rate, for whom limited options for effective treatment are available.
Although our results are not directly comparable with those from previous phase 2 studies in patients with R/R DLBCL, owing to the differing patient populations enrolled across studies, the observed CR rate for mosunetuzumab was similar to that achieved with approved therapies, such as loncastuximab teserine (CR rate 24%).15 CR rates of 40% were achieved with polatuzumab-bendamustine and rituximab (at end of treatment) and with tafa-len in a population that also included patients who had received only 1 previous line of therapy. Because of the heterogeneity of DLBCL, there are also a number of factors that may influence outcome of treatment with mosunetuzumab monotherapy in patients with DLBCL, in contrast to patients with FL,26 including cell-of-origin phenotype and tumor biology (such as MYC and/or BCL2 protein overexpression).27 Therefore, mosunetuzumab is being explored in combination with other therapies, such as polatuzumab vedotin for patients with R/R DLBCL; this combination has previously shown CR rates of 48%.28
CR rates of 40% to 58% were achieved in phase 2 studies with CAR-Ts.12,13,29 However, CAR-T efficacy needs to be balanced with the potential for severe toxicities, particularly ICANS, for which the pathophysiology and management are not well-established and may require prolonged hospitalization for observation or management in a specialized treatment center.30,31 Therefore, there remains an unmet need in patients with R/R DLBCL, who have limited treatment options, for alternative therapies with favorable safety profiles that can be immediately available and managed in an outpatient setting.
The excellent tolerability of mosunetuzumab monotherapy in this study was evidenced by the high proportion of patients (84.1%) receiving >90% dose intensity and the low proportion of patients withdrawing from treatment owing to AEs (4.5%; 4 patients). The type, incidence, and severity of AEs with mosunetuzumab in this study (ie, CRS, neutropenia, and infections) were manageable and consistent with those observed in the dose-escalation phase of the study in patients with B-cell lymphomas.21 No events of tumor lysis syndrome occurred in this cohort. Taken together, the safety profile of mosunetuzumab supports its future use beyond specialized comprehensive treatment centers. No firm conclusions could be made regarding differences in the safety profile of patients who received previous CAR-T therapy because of imbalances in baseline characteristics, the small sample sizes, and the exploratory nature of these analyses.
CRS was a common AE with mosunetuzumab monotherapy, which is consistent with findings from the phase 1 study with mosunetuzumab21 and studies with other T-cell engaging therapies.32-35 Our study showed that the CRS events with mosunetuzumab were mostly low grade, confined to the first cycle of treatment. Only 5.7% of patients required treatment with tocilizumab, and all CRS events were resolved and did not lead to treatment discontinuation. This further demonstrates that the recommended phase 2 dose schedule, with step-up dosing, provides effective mitigation for CRS. There were no cases of the severe neurological AEs that have been previously observed with CAR-Ts in patients with lymphoma,30,31 further validating the feasibility of outpatient treatment for patients receiving mosunetuzumab. This may be advantageous given the ongoing competing pressures on health care resources.
Several phase 1 or 2 trials with other CD20×CD3 bispecific antibodies (glofitamab, odronextamab, and epcoritamab) are ongoing, with initially observed promising antilymphoma activity.32-35 However, it is difficult to make cross-trial comparisons because of differences in patient populations, trial designs, and antibody format. The treatment regimens also vary among these bispecific antibodies. Although mosunetuzumab is administered for a fixed duration of treatment, some agents are given as treat-to-progression regimens and may require patients to be hospitalized for treatment initiation.
In summary, mosunetuzumab monotherapy is a well-tolerated, off-the-shelf agent that can be delivered in an outpatient setting, with activity in patients with R/R DLBCL, including those with trFL. Its administration as a fixed-duration regimen minimizes the potential for long-term or cumulative safety risks. This manageable safety profile makes it appealing for specific patient groups, such as elderly or unfit patients with previously untreated DLBCL,36 patients who are not candidates for ASCT or CAR-T therapy, or for use in combination with other therapies, such as polatuzumab vedotin28 or chemotherapy.37 Treatment-free intervals have also been shown to ameliorate T-cell exhaustion by bispecific molecules.38 In patients with R/R B-cell non-Hodgkin lymphoma, mosunetuzumab retreatment was effective and well-tolerated with a safety profile consistent with that observed with initial treatment.39 Further study is warranted to evaluate the potential use of mosunetuzumab in earlier lines of therapy and the optimal sequencing of treatment with other agents, including CAR-T therapies.
Acknowledgments
The authors thank the patients and their families, as well as the study investigators, study coordinators, nurses, and representatives of the sponsor who were involved in data collection and analyses.
NCT02500407 is sponsored by Genentech, Inc. Third party medical writing assistance, under the direction of N.B. and I.T., was provided by Scott Malkin and Louise Profit, of Ashfield MedComms, an Inizio company, and was funded by F. Hoffmann-La Roche Ltd.
Authorship
Contribution: L.E.B., M.C.W., N.L.B., and S.Y developed the concept and designed the study; A.J., C.P., C.Y.C., D.H.Y., F.B., G.P.G., I.F., K.F., N.L.B., L.E.B., M.C.W., M.M., M.S., P.G., S.A., S.J.S., and S.S.Y. provided study materials or patients; A.J., C.P., C.Y.C., D.H.Y., G.P.G., I.F., K.F., N.L.B., M.C.W., M.M., M.S., P.G., S.A., S.J.S., and S.S.Y. collected the data; A.J., A.K., C.C.L., E.P., I.T., H.H., M.C.W., and S.Y. analyzed the data; A.J., A.K., C.C.L., H.H., I.F., I.T., G.P.G., M.C.W., S.J.S., S.Y. interpreted the data; and all authors contributed in drafting and critically reviewing the article, and are accountable for all aspects of the work.
Conflict-of-interest disclosure: N.L.B. reports employment with Washington University School of Medicine; research funding from ADC Therapeutics, Autolus, Bristol Myers Squibb (BMS), Celgene, Forty Seven, Janssen, Kite Pharma, Merck, Millennium, and Seattle Genetics; and membership on an entity’s Board of Directors or advisory committees with ADC Therapeutics, F. Hoffmann-La Roche Ltd/Genentech, Inc., and Seattle Genetics. S.A. reports a consulting role with and honoraria from Genentech, Inc./F. Hoffmann-La Roche Ltd, AstraZeneca, Novartis, BMS, Jazz, Gilead, Amgen, BeiGene, AbbVie, and Paladin; and research funding from Novartis. P.G. reports employment with Royal Adelaide Hospital; honoraria from an education session organized by F. Hoffmann-La Roche Ltd in 2021; and membership on a F. Hoffmann-La Roche Ltd Advisory Committee in 2019. S.J.S. reports a consulting or advisory role with Celgene, Nordic Nanovector, Novartis, and Pfizer; honoraria from AbbVie, Acerta, Alimera Sciences, BeiGene, AstraZeneca, Celgene, Juno Therapeutics, Genentech, Inc./F. Hoffmann-La Roche Ltd, Loxo Oncology, Nordic Nanovector, Novartis, Pfizer, and Tessa Therapeutics; research funding from AbbVie, Acerta, Adaptive Biotechnologies, Celgene/Juno, DTRM, Genentech, Inc./F. Hoffmann-La Roche Ltd, Gilead, Incyte, Merck, Novartis, Pharmacyclics, and TG Therapeutics; and a patent for combination therapies of CAR-T and PD-1 inhibitors with royalties to Novartis. C.Y.C. reports a consulting and/or advisory role and honoraria from F. Hoffmann-La Roche Ltd, Janssen, MSD, Gilead, AstraZeneca, Lilly, TG Therapeutics, BeiGene, Novartis, and BMS and research funding from BMS, F. Hoffmann-La Roche Ltd, AbbVie, and MSD. M.M. reports employment with Memorial Sloan Kettering Cancer Centre; a consulting role with ADC Therapeutics, AstraZeneca, Bayer, Daiichi Sankyo, Epizyme, F. Hoffmann-La Roche Ltd, Genentech, Inc., IMV Therapeutics, Juno Therapeutics, Karyopharm, Merck, MEI Pharma, Rocket Medical, Seattle Genetics, TG Therapeutics, Teva, and Bayer; and holds stocks in Merck. G.P.G. reports a consulting and/or advisory role and honoraria from F. Hoffmann-La Roche Ltd, Janssen, MSD, Gilead, Novartis, AstraZeneca and LINK Clinigen and research funding from MSD, BeiGene, Janssen and AbbVie. D.H.Y. reports a consulting role with GI cell, AB clone, and Pharos iBio; research funding from Samyang, Boryung, BeiGene, Sanofi, Celltrion, and Janssen; and honoraria from F. Hoffmann-La Roche Ltd, Janssen, Amgen, BMS, Novartis, Celltrion, Samyang, Boryung, Kirin Pharm, Takeda, GlaxoSmithKline, and Janssen. M.S. reports a consulting and/or advisory role with AbbVie, Genentech, Inc., AstraZeneca, Sound Biologics, Pharmacyclics, BeiGene, BMS, MorphoSys/Incyte, TG Therapeutics, Innate Pharma, Kite Pharma, Adaptive Biotechnologies, Epizyme, Eli Lilly, Adaptimmune, Mustang Bio, Regeneron, Merck, Fate Therapeutics, MEI Pharma, and Atara Biotherapeutic; and research funding from Mustang Bio, Celgene, BMS, Pharmacyclics, Gilead, Genentech, Inc., AbbVie, TG Therapeutics, BeiGene, AstraZeneca, Sunesis, Atara Biotherapeutics, Genmab, MorphoSys/Incyte, and Vincrex. K.F. reports employment with St. Vincent’s Hospital, Sydney, Australia. S.-S.Y. reports a consulting or advisory role with Amgen, Antengene, Astellas, Celgene, Janssen, Novartis, and Takeda; honoraria from Novartis; and research funding from Kyowa Kirin, F. Hoffmann-La Roche Ltd/Genentech, Inc., and Yuhan Pharmaceutical. C.P. reports a consulting or advisory role with F. Hoffmann-La Roche Ltd, Janssen, Gilead, Incyte, and BeiGene. I.F. reports a consulting role with AbbVie, AstraZeneca, BeiGene, Century Therapeutics, Genentech, Inc., Genmab, Gilead Sciences, Great Point Partners, Hutchison MediPharma, Iksuda Therapeutics, InnoCare Pharma, Janssen, Juno Therapeutics, Kite Pharma, MorphoSys, Novartis, Nurix Therapeutics, Pharmacyclics, F. Hoffmann-La Roche Ltd, Seattle Genetics, Servier Pharmaceuticals, Takeda, TG Therapeutics, Unum Therapeutics, Verastem, Vincerx Pharma, and Yingli Pharmaceuticals; and research funding from AbbVie, Acerta Pharma, Agios, ArQule, AstraZeneca, BeiGene, Biopath, BMS, CALIBR, CALGB, Celgene, City of Hope National Medical Center, Constellation Pharmaceuticals, Curis, CTI Biopharma, Fate Therapeutics, Forma Therapeutics, Forty Seven, Genentech, Inc., Gilead Sciences, InnoCare Pharma, IGM Biosciences, Incyte, Infinity Pharmaceuticals, Janssen, Kite Pharma, Loxo, Merck, Millennium Pharmaceuticals, MorphoSys, Myeloid Therapeutics, Novartis, Nurix, Pfizer, Pharmacyclics, Portola Pharmaceuticals, Rhizen Pharmaceuticals, F. Hoffmann-La Roche Ltd, Seattle Genetics, Tessa Therapeutics, TCR2 Therapeutics, TG Therapeutics, Trillium Therapeutics, Triphase Research & Development Corp, Unum Therapeutics, and Verastem (payments made to Sarah Cannon Research Institute for all consulting and research funding). A.J. reports a consulting or advisory role with F. Hoffmann-La Roche Ltd, BeiGene, Novartis, and Sanofi. F.B. reports employment with Vall D’Hebron University Hospital, Barcelona; a consulting role with F. Hoffmann-La Roche Ltd, Genentech, Inc., Novartis, Janssen, AbbVie, Gilead/Kite, Mundipharma, Takeda, Celgene/BMS, AstraZeneca, Lilly, BeiGene, TG Therapeutics, Advantage Allogene, Lava Therapeutics, and Enterome; research funding from F. Hoffmann-La Roche Ltd, Genentech, Inc., AbbVie, Janssen, Lilly, AstraZeneca, Novartis, Kite, BMS, Takeda, TG Therapeutics, BeiGene, Advantage, Allogene, Lava Therapeutics, and Enterome; honoraria from F. Hoffmann-La Roche Ltd, Genentech, Inc., Novartis, Janssen, AbbVie, Gilead/Kite, Mundipharma, Takeda, Celgene/BMS, AstraZeneca, Lilly, BeiGene, TG Therapeutics, Advantage, Allogene, Lava Therapeutics, and Enterome; speaker's bureaus with F. Hoffmann-La Roche Ltd, Genentech, Inc., Novartis, Janssen, AbbVie, Gilead/Kite, Mundipharma, Takeda, Celgene/BMS, AstraZeneca, Lilly, BeiGene, TG Therapeutics, Advantage, Allogene, Lava Therapeutics, and Enterome; and other from F. Hoffmann-La Roche Ltd, Novartis, Janssen, AbbVie, Gilead, Mundipharma, Celgene/BMS, Takeda, and AstraZeneca. M.C.W. and S.Y. report employment with Genentech, Inc.; meeting attendance and/or travel support from F. Hoffmann-La Roche Ltd/Genentech, Inc.; and stocks and stock options in F. Hoffmann-La Roche Ltd. I.T. and E.P. report employment with and are equity holders in Genentech, Inc. C.-C.L. reports employment with and stocks and stock options in F. Hoffmann-La Roche Ltd, and a patent for dosing for treatment with anti-CD20/anti-CD3 bispecific antibodies. H.H. reports employment with F. Hoffmann-La Roche Ltd. A.K. reports employment with and holds stocks in F. Hoffmann-La Roche Ltd. L.E.B. reports consulting fees from Genentech, Inc., ADC Therapeutics, Merck, AstraZeneca and Amgen, and participation on a Data Safety Monitoring Board for Ziopharm Oncology. L.H.S. declares no competing financial interests.
The current affiliation for M.M. is Rutgers Cancer Institute of New Jersey, New Brunswick, NJ.
Correspondence: Lihua E. Budde, City of Hope National Medical Center, 1500 E Duarte Rd, Duarte, CA 91010; e-mail: ebudde@coh.org.
References
Author notes
∗N.L.B. and S.A. are joint lead authors.
Qualified researchers may request access to individual patient level data through the clinical study data request platform (https://vivli.org/). Further details on Roche’s criteria for eligible studies are available at https://vivli.org/members/ourmembers/. For further details on Roche’s Global Policy on the Sharing of Clinical Information and how to request access to related clinical study documents, refer to the following URL: (https://www.roche.com/research_and_development/who_we_are_how_we_work/clinical_trials/our_commitment_to_data_sharing.htm).
The full-text version of this article contains a data supplement.