Key Points
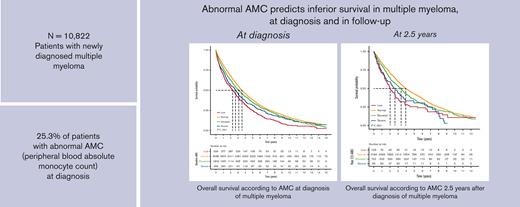
Abnormal AMC at diagnosis and follow-up predicts inferior OS in patients with MM.
This study highlights the role of AMC as a readily available prognostic biomarker throughout the course of MM.
Abstract
With the growing knowledge of multiple myeloma (MM) pathobiology and the introduction of novel therapies, risk stratification continues to evolve. Myeloid-derived suppressor cells and tumor-associated macrophages, derived from peripheral blood monocytes, support malignant plasma cell proliferation in the bone marrow. Because peripheral blood absolute monocyte count (AMC) is thought to reflect the bone marrow microenvironment, we sought to evaluate the prognostic significance of AMC in MM. We retrospectively analyzed 10 822 patients newly diagnosed with MM between 2000 and 2019 at Veteran’s Administration hospitals. We obtained AMC closest to diagnosis and every 3 months thereafter up to 2.5 years. Patients were stratified into 4 groups: low, normal, elevated, and severely elevated AMC (<0.2, 0.2-<0.8, 0.8-<1.25, and ≥1.25 × 103/mm3, respectively). Abnormal AMC at diagnosis was observed in 25.3% of the patients and was associated with an inferior overall survival (OS). In patients with low, severely elevated, elevated, and normal AMC, respectively, median OS at diagnosis was 2.3, 2.7, 3.1, and 3.6 years (P < .001) and at 2.5 years was 2.0, 2.6, 3.4, and 3.9 years (P < .001). Patients with normal AMC at diagnosis who developed an abnormal AMC >1 year after diagnosis also had an inferior OS relative to patients who maintained a normal AMC. Abnormal AMC was also associated with inferior OS independent of validated prognostic markers, including the international staging system and lactate dehydrogenase. Our findings provide novel clues for future prospective studies on the functional role of monocytes in MM, which could be a readily available metric for risk stratification.
Introduction
Multiple myeloma (MM) is a plasma cell malignancy accounting for ∼19% of newly diagnosed hematologic neoplasms.1 The median overall survival (OS) has improved with the advent of novel therapies.2,3 Nonetheless, a subset of patients with MM still experience early relapse and mortality.
Defining the risk and using risk-adapted treatment strategies in MM are areas of unmet need. The current standard for risk stratification, the revised international staging system (R-ISS) is applicable only at diagnosis.4 The R-ISS incorporates genetic and nongenetic features such as albumin, lactate dehydrogenase (LDH), and β-2-microglobulin (β2m). Although the development of adverse cytogenetic features at relapse or progression may predict high-risk disease and poor outcomes, redetermination would require invasive testing, which is not feasible at frequent intervals. Moreover, the use of redetermination of nongenetic risk factors from the R-ISS at follow-up is unclear.5 Dynamic prognostication and risk stratification is paramount in refining treatment strategies to improve outcomes in patients at high risk.
One major advancement in our knowledge of MM pathophysiology is an improved understanding of the interactions between MM cells with their bone marrow microenvironment. As the disease progresses, malignant plasma cells interact with the bone marrow microenvironment to form a complex ecosystem that promotes MM cell proliferation and survival and the development of drug resistance. Specifically, there is an increased number of monocytic myeloid-derived suppressor cells (MDSCs) in the blood and bone marrow of patients with MM, which interact with MM cells in a bidirectional manner.6 MM cells stimulate MDSC differentiation and function, whereas MDSCs promote immune escape, disease progression, and resistance to treatment. Tumor-associated macrophages (TAMs) are also fundamental elements of the tumor microenvironment and are derived from monocytes in the peripheral blood. TAMs migrate into the tumor microenvironment under the influence of tumor-derived chemotactic factors and complement MM cells by inhibiting MM cell death, supporting MM cell growth, and suppressing anti-MM immune responses.7
Given the need for improved prognostic tools throughout the course of MM disease as well as the associations between peripheral blood monocyte–derived TAMs, monocytic-MDSCs, and MM cell survival, we investigated whether the peripheral blood absolute monocyte count (AMC) may be used to predict survival of patients with MM.
Methods
Patients
Our retrospective study used data from the integrated nationwide Veterans Affairs (VA) electronic health records and the prospectively maintained VA Corporate Data Warehouse. We evaluated 10 822 patients diagnosed with MM between 1 January 2000 and 30 June 2019. Patients were identified using the 9th and 10th editions of the international classification of diseases (ICD) codes for MM and were required to have at least 3 visits with an MM ICD code on separate days. Eligible patients were followed through 31 January 2021. The date of diagnosis was the date of the first MM treatment. We included patients who received at least 1 MM drug (besides corticosteroids) on or after the date of diagnosis. Because other hematologic malignancies could cause an abnormal AMC, we excluded patients with acute and chronic leukemias, aplastic anemia, myelodysplastic syndrome, hairy cell leukemia, and myeloproliferative neoplasms before MM diagnosis. We also censored patients who developed such conditions during follow-up at the corresponding date of diagnosis of the confounding condition.
Study variables and assessments
Baseline data obtained included the date of diagnosis, age, sex, race, serum LDH, β2m, serum albumin, and serum creatinine. Stage was calculated using baseline data (serum albumin and β2m) and classified according to the ISS, which is known to be associated with OS in newly diagnosed MM.8 The time to follow-up was defined as the time from the date of diagnosis until development of another hematologic malignancy, death, truncation date (15 years after MM diagnosis), or the study end date, whichever came first.
Monocytosis was defined based on the institution’s cut-off as an AMC increase greater than 0.8 × 103 (800/mm3). We obtained baseline and follow-up AMC in patients whose AMC was measured using an automated or manual differential. We used the AMC closest to and within 90 days of MM diagnosis and at 3-month intervals until 2.5 years after diagnosis. We chose a cut-off of 2.5 years based on the median OS of our cohort. AMC at the timepoint of interest was used to assign patients to AMC categories for the final analysis. Patients were stratified into 4 AMC categories: low (<0.2), normal (0.2-<0.8), elevated (0.8-<1.25), and severely elevated (≥1.25). To avoid using treatment-related changes in AMC, we excluded any AMC obtained within 7 days of an abnormal neutrophil count. Survival analysis at each time interval included patients who had available laboratory data.
Statistical analysis
Descriptive statistics, including medians and interquartile ranges (IQRs), were used to summarize demographic and baseline characteristics of all patients. Age was used as a continuous variable. Race categories included Black, White, and other. We compared baseline characteristics between the 4 AMC groups using the nonparametric Kruskal-Wallis test for continuous variables and the χ2 test for categorical variables. The primary outcome was OS estimated using the Kaplan-Meier method and log-rank tests. We censored patients from the survival analysis who were lost to follow-up. We used Cox proportional hazard models, with adjustment for age, race, Charlson comorbidity index (CCI), smoking status, ISS, LDH, creatinine, and era of treatment (< 2007, ≥2007-< 2012, and ≥2012) to obtain hazard ratios (HRs). Missing data were imputed using the multiple imputation by chained equations method. The statistical analysis was performed using R version 4.0.3 software package. All statistical tests were two-sided and a P < .05 was considered statistically significant.
Study oversight
Our study had local institutional review board approval (3093) and was performed in accordance with the principles of the Declaration of Helsinki.
Results
We evaluated data from 10 822 patients who were newly diagnosed with MM at VA medical centers between 2000 and 2019, and their demographic and clinical characteristics are outlined in Table 1. The median age at diagnosis was 69.7 years (IQR 62.9-77.0 years), with 97.6% of patients being male. AMC did not vary significantly based on race. Abnormal AMC (including low, elevated, and severely elevated) was present in 25.3% of patients at diagnosis (2737 out of 10 822 patients); with 5% having low, 16.7% having elevated, and 3.6% having severely elevated AMC. Patients with monocytosis (elevated or severely elevated AMC) had higher median LDH (179 [IQR, 139-246] and 216 [IQR 161-345], respectively). Among evaluable patients, ISS stage 2 and 3 was present in 73.3% of the overall cohort and in 82.5%, 72.1%, 75.2%, and 77.5% of patients with low, normal, elevated, and severely elevated AMC, respectively.
Demographics and clinical characteristics of patients with MM at diagnosis included in the study (n = 10 822)
| . | Overall . | AMC (× 103/mm3) . | P value . | |||
|---|---|---|---|---|---|---|
| Low (<200) . | Normal (200 to <800) . | Elevated (800 to <1250) . | Severely elevated (≥1250) . | |||
| Number of patients, n (%) | 10 822 | 539 (5.0) | 8085 (74.7) | 1803 (16.7) | 395 (3.6) | |
| Age at diagnosis, median [IQR] | 69.7 [62.9-77.0] | 72.6 [65.4-78.6] | 69.7 [62.9-77.0] | 69.1 [62.5-76.3] | 68.7 [61.8-76.2] | <.001 |
| Median follow up, median [IQR] | 2.92 [1.33-5.26] | 2.20 [0.70-4.29] | 3.03 [1.47-5.36] | 2.67 [1.16-5.05] | 2.47 [0.93-4.63] | <.001 |
| Male sex, n (%) | 10562 (97.6) | 525 (97.4) | 7880 (97.5) | 1767 (98.0) | 390 (98.7) | .247 |
| Race, n (%) | .027 | |||||
| Black | 2701 (25.0) | 119 (22.1, 4.4∗) | 2052 (25.4, 76.0∗) | 415 (23.0, 15.4∗) | 115 (29.1, 4.3∗) | |
| White | 6546 (60.5) | 327 (60.7, 5.0∗) | 4851 (60.0, 74.1∗) | 1130 (62.7, 17.3∗) | 238 (60.3, 3.6∗) | |
| Other/Unknown | 1575 (14.5) | 93 (17.3, 5.9∗) | 1182 (14.6, 75.0∗) | 258 (14.3, 16.4∗) | 42 (10.6, 2.7∗) | |
| Smoking status† (%) | 0.144 | |||||
| Never | 2411 (22.3) | 114 (4.7)∗ | 1816 (75.3)∗ | 388 (16.1)∗ | 93 (3.9)∗ | |
| Current/ Former | 6893 (63.7) | 327 (4.7)∗ | 5147 (74.7)∗ | 1171 (17.0)∗ | 248 (3.6)∗ | |
| Charlson Comorbidity Index (CCI score) | 0.157 | |||||
| No comorbidities | 466 (4.3) | 22 (4.7)∗ | 332 (71.2)∗ | 95 (20.4)∗ | 17 (3.7)∗ | |
| Mild (1 - 2) | 5998 (55.4) | 289 (4.8)∗ | 4546 (75.8)∗ | 946 (15.8)∗ | 217 (3.6)∗ | |
| Moderate (3 - 4) | 3198 (29.6) | 166 (5.2)∗ | 2353 (73.6)∗ | 566 (17.7)∗ | 113 (3.5)∗ | |
| Severe (>5) | 1160 (10.7) | 62 (5.3)∗ | 854 (73.6)∗ | 196 (16.9)∗ | 48 (4.1)∗ | |
| Distribution of ISS stages across the 4 AMC groups, n (%)† | <.001 | |||||
| Stage 1 | 1304 (26.7) | 43 (3.3)∗ | 1037 (79.5)∗ | 190 (14.6)∗ | 34 (2.6)∗ | |
| Stage 2 | 2243 (45.9) | 123 (5.5)∗ | 1697 (75.7)∗ | 363 (16.2)∗ | 60 (2.7)∗ | |
| Stage 3 | 1338 (27.4) | 80 (6.0)∗ | 987 (73.8)∗ | 214 (16.0)∗ | 57 (4.3)∗ | |
| β2m† | <.001 | |||||
| β2m, median [IQR] | 3.9 [2.7-5.7] | 4.4 [3.1-6.0] | 3.8 [2.7-5.6] | 4.0 [2.7-5.8] | 4.8 [2.8-6.8] | |
| Serum albumin† | <.001 | |||||
| Low albumin, n (%) | 4938 (45.6) | 288 (5.8)∗ | 3579 (72.5)∗ | 855 (17.3)∗ | 216 (4.4)∗ | |
| Albumin, median [IQR] (g/dL) | 3.50 [3.00-3.90] | 3.30 [2.90-3.80] | 3.50 [3.00-3.90] | 3.48 [2.90-3.90] | 3.30 [2.80-3.80] | |
| Creatinine, median [IQR] (mg/dL) | 1.2 [1.0-1.8] | 1.3 [1.0-1.7] | 1.2 [1.0-1.7] | 1.3 [1.0-2.0] | 1.3 [1.0-2.3] | <.001 |
| Serum LDH† | <.001 | |||||
| High LDH, n (%) | 1228 (21.3) | 85 (6.9)∗ | 825 (67.2)∗ | 239 (19.5)∗ | 79 (6.4)∗ | |
| LDH, median [IQR] (U/L) | 169 [132-228] | 168 [123-246] | 166 [130-220] | 179 [139-246] | 216 [161-345] | |
| TP53 Deletion† | 163 (9.2) | 25 (15.3)∗ | 104 (63.8)∗ | 26 (15.9)∗ | 8 (4.9)∗ | <.001 |
| MM diagnosis date, n (%) | .002 | |||||
| <2007 | 2783 (25.7) | 174 (6.3)∗ | 2034 (73.1)∗ | 456 (16.4)∗ | 119 (4.3)∗ | |
| ≥2007 to <2012 | 2723 (25.2) | 133 (4.9)∗ | 2050 (75.3)∗ | 457 (16.8)∗ | 83 (3.0)∗ | |
| ≥2012 | 5316 (49.1) | 232 (4.4)∗ | 4001 (75.3)∗ | 890 (16.7)∗ | 193 (3.6)∗ | |
| . | Overall . | AMC (× 103/mm3) . | P value . | |||
|---|---|---|---|---|---|---|
| Low (<200) . | Normal (200 to <800) . | Elevated (800 to <1250) . | Severely elevated (≥1250) . | |||
| Number of patients, n (%) | 10 822 | 539 (5.0) | 8085 (74.7) | 1803 (16.7) | 395 (3.6) | |
| Age at diagnosis, median [IQR] | 69.7 [62.9-77.0] | 72.6 [65.4-78.6] | 69.7 [62.9-77.0] | 69.1 [62.5-76.3] | 68.7 [61.8-76.2] | <.001 |
| Median follow up, median [IQR] | 2.92 [1.33-5.26] | 2.20 [0.70-4.29] | 3.03 [1.47-5.36] | 2.67 [1.16-5.05] | 2.47 [0.93-4.63] | <.001 |
| Male sex, n (%) | 10562 (97.6) | 525 (97.4) | 7880 (97.5) | 1767 (98.0) | 390 (98.7) | .247 |
| Race, n (%) | .027 | |||||
| Black | 2701 (25.0) | 119 (22.1, 4.4∗) | 2052 (25.4, 76.0∗) | 415 (23.0, 15.4∗) | 115 (29.1, 4.3∗) | |
| White | 6546 (60.5) | 327 (60.7, 5.0∗) | 4851 (60.0, 74.1∗) | 1130 (62.7, 17.3∗) | 238 (60.3, 3.6∗) | |
| Other/Unknown | 1575 (14.5) | 93 (17.3, 5.9∗) | 1182 (14.6, 75.0∗) | 258 (14.3, 16.4∗) | 42 (10.6, 2.7∗) | |
| Smoking status† (%) | 0.144 | |||||
| Never | 2411 (22.3) | 114 (4.7)∗ | 1816 (75.3)∗ | 388 (16.1)∗ | 93 (3.9)∗ | |
| Current/ Former | 6893 (63.7) | 327 (4.7)∗ | 5147 (74.7)∗ | 1171 (17.0)∗ | 248 (3.6)∗ | |
| Charlson Comorbidity Index (CCI score) | 0.157 | |||||
| No comorbidities | 466 (4.3) | 22 (4.7)∗ | 332 (71.2)∗ | 95 (20.4)∗ | 17 (3.7)∗ | |
| Mild (1 - 2) | 5998 (55.4) | 289 (4.8)∗ | 4546 (75.8)∗ | 946 (15.8)∗ | 217 (3.6)∗ | |
| Moderate (3 - 4) | 3198 (29.6) | 166 (5.2)∗ | 2353 (73.6)∗ | 566 (17.7)∗ | 113 (3.5)∗ | |
| Severe (>5) | 1160 (10.7) | 62 (5.3)∗ | 854 (73.6)∗ | 196 (16.9)∗ | 48 (4.1)∗ | |
| Distribution of ISS stages across the 4 AMC groups, n (%)† | <.001 | |||||
| Stage 1 | 1304 (26.7) | 43 (3.3)∗ | 1037 (79.5)∗ | 190 (14.6)∗ | 34 (2.6)∗ | |
| Stage 2 | 2243 (45.9) | 123 (5.5)∗ | 1697 (75.7)∗ | 363 (16.2)∗ | 60 (2.7)∗ | |
| Stage 3 | 1338 (27.4) | 80 (6.0)∗ | 987 (73.8)∗ | 214 (16.0)∗ | 57 (4.3)∗ | |
| β2m† | <.001 | |||||
| β2m, median [IQR] | 3.9 [2.7-5.7] | 4.4 [3.1-6.0] | 3.8 [2.7-5.6] | 4.0 [2.7-5.8] | 4.8 [2.8-6.8] | |
| Serum albumin† | <.001 | |||||
| Low albumin, n (%) | 4938 (45.6) | 288 (5.8)∗ | 3579 (72.5)∗ | 855 (17.3)∗ | 216 (4.4)∗ | |
| Albumin, median [IQR] (g/dL) | 3.50 [3.00-3.90] | 3.30 [2.90-3.80] | 3.50 [3.00-3.90] | 3.48 [2.90-3.90] | 3.30 [2.80-3.80] | |
| Creatinine, median [IQR] (mg/dL) | 1.2 [1.0-1.8] | 1.3 [1.0-1.7] | 1.2 [1.0-1.7] | 1.3 [1.0-2.0] | 1.3 [1.0-2.3] | <.001 |
| Serum LDH† | <.001 | |||||
| High LDH, n (%) | 1228 (21.3) | 85 (6.9)∗ | 825 (67.2)∗ | 239 (19.5)∗ | 79 (6.4)∗ | |
| LDH, median [IQR] (U/L) | 169 [132-228] | 168 [123-246] | 166 [130-220] | 179 [139-246] | 216 [161-345] | |
| TP53 Deletion† | 163 (9.2) | 25 (15.3)∗ | 104 (63.8)∗ | 26 (15.9)∗ | 8 (4.9)∗ | <.001 |
| MM diagnosis date, n (%) | .002 | |||||
| <2007 | 2783 (25.7) | 174 (6.3)∗ | 2034 (73.1)∗ | 456 (16.4)∗ | 119 (4.3)∗ | |
| ≥2007 to <2012 | 2723 (25.2) | 133 (4.9)∗ | 2050 (75.3)∗ | 457 (16.8)∗ | 83 (3.0)∗ | |
| ≥2012 | 5316 (49.1) | 232 (4.4)∗ | 4001 (75.3)∗ | 890 (16.7)∗ | 193 (3.6)∗ | |
Denotes row percentages.
Data available on 9304 (86.0%) patients on smoking status, 4885 (45.1%) patients on ISS Staging, 4944 (46.1%) patients on β2m, 5763 (53.3%) patients on LDH >243 U/L and 1783 (16.4%) patients on TP53 deletion.
Inferior OS with abnormal AMC at diagnosis
Median OS of the entire population was 3.36 years (95% confidence interval [CI], 3.26-3.47). The OS of patients with abnormal AMC at diagnosis was significantly inferior than that of patients with normal AMC. Median OS of patients with low, severely elevated, elevated, and normal AMC at diagnosis was 2.3, 2.7, 3.1, and 3.6 years (P < .001), respectively (Figure 1).
OS based on AMC at the diagnosis of MM. Kaplan-Meier curves of OS based on AMC at the diagnosis of MM.
OS based on AMC at the diagnosis of MM. Kaplan-Meier curves of OS based on AMC at the diagnosis of MM.
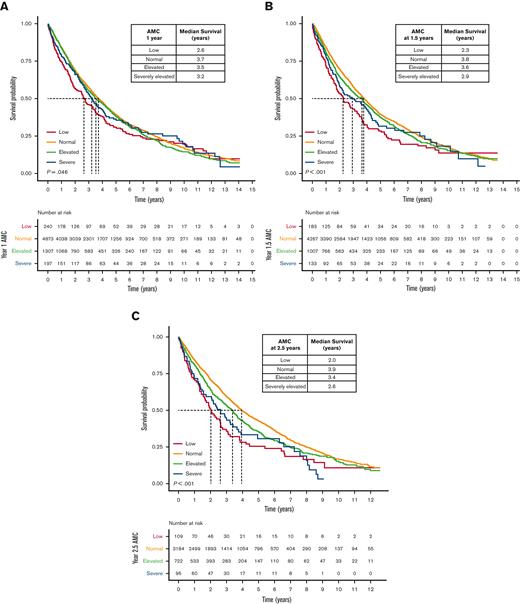
Abnormal AMC after diagnosis is associated with poor OS
We next evaluated AMC at follow-up time points after induction therapy. Abnormal AMC (low, elevated, and severely elevated) at multiple subsequent time points indicated poor OS (Figure 2; supplemental Figure 1). We focused on later time points when the direct impact of induction regimen might have been less. As seen in Figure 2A-B, abnormal AMC at 1 and 2.5 years after MM diagnosis was associated with significantly lower OS at both the time points. Median OS at 1 year was 2.6, 3.2, 3.5, and 3.7 years (P = .046), whereas the median OS at 2.5 years was 2.0, 2.6, 3.4, and 3.9 years (P < .001) in patients with low, severely elevated, elevated, and normal AMC, respectively.
OS based on AMC during follow-up of MM, independent of baseline AMC. (A-C) Kaplan-Meier curves of OS based on AMC (A) 1 year after MM diagnosis, (B) 1.5 years after MM diagnosis, and (C) 2.5 years after MM diagnosis.
OS based on AMC during follow-up of MM, independent of baseline AMC. (A-C) Kaplan-Meier curves of OS based on AMC (A) 1 year after MM diagnosis, (B) 1.5 years after MM diagnosis, and (C) 2.5 years after MM diagnosis.
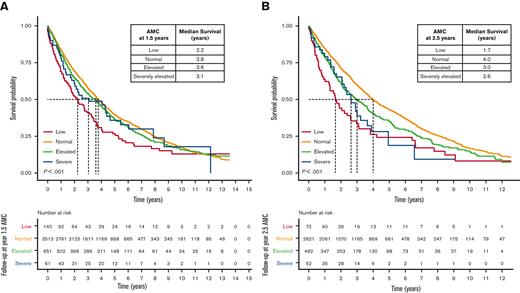
Developing an abnormal AMC during follow-up is associated with poor OS
We further investigated whether a change in AMC category at follow-up from AMC at diagnosis was predictive of outcome. Patients with normal AMC at diagnosis who developed abnormal AMC >1 year after MM diagnosis experienced inferior outcomes compared with patients who maintained a normal AMC (Figure 3A-B). In contrast, patients with monocytosis at diagnosis (both elevated and severely elevated) had no significant change in survival irrespective of whether the abnormal AMC persisted or normalized (supplemental Figure 3C-E). We did not have an adequate number of patients with low AMC at diagnosis to study the impact of change in AMC at follow-up.
OS based on AMC during follow-up of MM for patients with a normal AMC at baseline. (A-B) Kaplan-Meier curves of OS in patients with normal AMC at diagnosis (baseline) based on AMC (A) 1.5 years after MM diagnosis and (B) at 2.5 years after MM diagnosis.
OS based on AMC during follow-up of MM for patients with a normal AMC at baseline. (A-B) Kaplan-Meier curves of OS in patients with normal AMC at diagnosis (baseline) based on AMC (A) 1.5 years after MM diagnosis and (B) at 2.5 years after MM diagnosis.
Abnormal AMC is associated with adverse outcomes in the era of novel therapies
With the availability of novel agents, there have been significant advances in the standard of care for patients with MM, improving the OS. We evaluated whether abnormal AMC had a similar effect on the outcome with the use of novel therapies. We compared the impact of abnormal AMC on the OS in patients treated before or after 2012 when novel agents were universally used in VA health care system. The median OS improved across all AMC groups in patients with MM diagnosed after 2012. However, the adverse effect of AMC on survival of patients with low, elevated, or severely elevated AMC persisted across treatment eras (Figure 4A-B). The median OS at 2.5 years for patients diagnosed before 2012 versus ≥ 2012 was 1.9 vs 2.4, 2.3 vs 2.9, 3.1 vs 3.6, and 3.6 vs 5.0 years for low, severely elevated, elevated, and normal AMC groups, respectively.
OS based on AMC 2.5 years after MM diagnosis with respect to the era of diagnosis and treatment (< 2012 and > 2012). (A-B) Kaplan-Meier curves of OS in patients with MM diagnosed and treated (A) before the year 2012 and (B) in the year 2012 or later.
OS based on AMC 2.5 years after MM diagnosis with respect to the era of diagnosis and treatment (< 2012 and > 2012). (A-B) Kaplan-Meier curves of OS in patients with MM diagnosed and treated (A) before the year 2012 and (B) in the year 2012 or later.
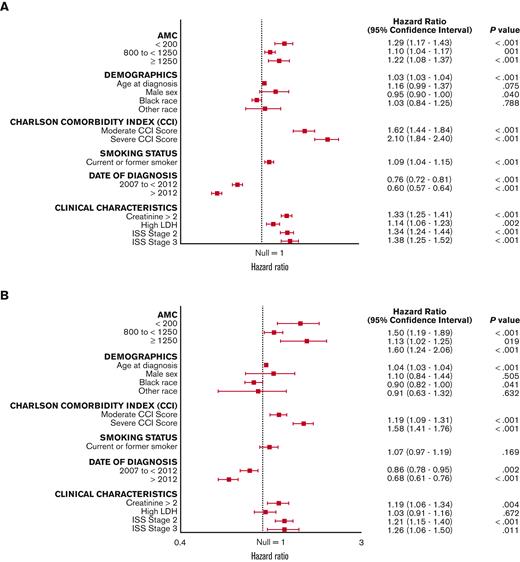
Inferior OS with abnormal AMC independent of validated prognostic factors
Multivariable analyses were done including validated significant predictors of OS at MM diagnosis (Figure 5). We observed that abnormal baseline AMC predicts poor outcomes even after adjusting for validated prognostic factors in MM, such as age, high ISS stage, and elevated LDH (Figure 5A). Specifically, severely elevated AMC portends the highest risk of death (HR 1.89; 95% CI, 1.43-2.49; P < .001). For low and elevated AMC, the magnitude of the effect on OS was similar to that of other prognostic factors. The significant association of AMC with OS was maintained even 2.5 years after MM diagnosis (Figure 5B).
Multivariable analysis of the main prognostic factors for OS. (A-B) Forest plot for subgroup analysis of OS (A) at diagnosis of MM and (B) 2.5 years after diagnosis of MM.
Multivariable analysis of the main prognostic factors for OS. (A-B) Forest plot for subgroup analysis of OS (A) at diagnosis of MM and (B) 2.5 years after diagnosis of MM.
Discussion
Despite marked improvement in outcomes of patients with MM, patients with high-risk disease experience early relapse and mortality. With the identification of newer genomic and clinical markers of high-risk MM, risk-adapted treatment strategies continue to evolve with the introduction of novel therapies. Risk stratification has been developed for MM at diagnosis but needs to be refined as our knowledge of disease pathobiology evolves. Based on previous results suggesting the tumor-promoting biological role of MDSCs and TAMs, we have explored the impact of AMC, a widely available peripheral blood test indirectly reflecting the supportive tumor microenvironment, on the outcome in MM. We report abnormal AMC both at diagnosis and subsequently at 1 and 2.5 years of follow-up to predict survival. At MM diagnosis, a low or high AMC is associated with poor OS. For patients with normal AMC at diagnosis, developing an abnormal AMC (low or high) after the first year of diagnosis (the period of induction and consolidation treatment) also confers inferior survival compared with those who maintain a normal AMC. AMC also predicts an adverse outcome independent of validated prognostic markers (ISS and high LDH) and other predictors such as age and CCI. Thus, AMC can serve as a biomarker for risk stratification in MM at diagnosis and follow-up. The association between AMC and inferior clinical outcomes has been proposed in several studies of both hematologic and solid organ malignancies.9-15 However, limited information is available regarding the prognostic significance of AMC in MM.9 The association of poor clinical outcomes with high AMC at diagnosis and follow-up highlights AMC as a possible surrogate for the tumor microenvironment.7,16-19
Our observations raise questions about the mechanism driving the impact of increased AMC on the outcome. This is especially intriguing because both high and low AMC have similar adverse effects on the outcome. Peripheral blood monocyte–derived TAMs are cellular components of the bone marrow niche that promote MM cell survival and resistance to drug-induced apoptosis by complex interactions.7,16-19 High AMC at diagnosis or its occurrence later in follow-up could potentially reflect their direct or indirect effects on MM cells through various cell surface receptors or soluble factors. Importantly, we also found that low AMCs at diagnosis and follow-up were predictive of poor survival. The mechanism driving this effect is unlikely to be the same as that described for patients with increased AMCs. Monocytopenia has been reported in the context of leukemia, lymphoma, and MM as an immune system biomarker. Although the exact mechanism is unknown, studies suggest that there could be defective hematopoiesis because of high tumor burden within the bone marrow.20 Functional impairment of hematopoietic stem cells results in immunosuppression and evasion of the immune system by MM cells, which could possibly lead to more aggressive disease, susceptibility to infections, and poorer clinical outcomes. We have also investigated whether the impact of abnormal AMC is still observed with the use of novel agents. Inferior outcomes in patients with abnormal AMC diagnosed after 2012 when the use of novel agents became universal suggests a broader significance of abnormal AMC in myeloma pathobiology. Overall, our findings emphasize the need to study the role of macrophage-monocyte interactions in MM pathobiology.
Our study results have several implications. Firstly, the time-varying prognostication afforded by the AMC is an inexpensive addition to the standard of care and may complement current tools used for risk stratification and treatment optimization. Secondly, our observations could provide insights into potential therapeutic targets for a subset of patients at high risk. Prospective studies would still be needed to examine the effect of specific therapies that may modulate monocyte function and its consequent effect on MM cell growth and survival. A further characterization of the monocyte population is warranted to determine if any specific monocytic subpopulation may be driving the poor outcome.
In addition, there are some limitations of our study, including its retrospective nature and the lack of data on other cytogenetics besides del 17p. Because this is a veteran’s hospital study, the cohort described is predominantly male. Moreover, the method of excluding AMC values within 7 days of neutropenia may not reliably predict treatment-related changes in AMC. We observed small but statistically significant associations between AMC levels and in both age and race and therefore adjusted for these variables in our multivariable analysis, but future work can shed additional light on these relationships. Finally, while our epidemiologic study is based on a large database of real-world data, future work is needed to confirm these findings, such as prospective studies including functional assays.
Overall, we report that the peripheral blood AMC is an inexpensive, widely available, and easily interpretable risk stratification tool with clinical use that is not limited to the time of diagnosis. Based on the results of our study, AMC measured every 3 months during the initial 2.5 years of MM treatment could identify patients at high risk and predict OS. The findings could support the use of AMC for MM prognostication and highlight the potential to develop targeted therapies.
Acknowledgment
The authors thank the National Institutes of Health, Department of VA (research funding 1I01BX001584; NIH grant number P01-155258-07 including supplements 3P01CA155258-07S1 and 3P01CA155258-07S2) for funding this research.
Authorship
Contribution: C.V.E. and N.C.M. designed research, performed research, analyzed data, interpreted results, and wrote and edited the manuscript; C.Y. and N.R.F. performed research, analyzed data, interpreted results, and edited the manuscript; H.H., K.P.V., and G.F. analyzed data, interpreted results, and edited the manuscript; and M.E.M.H. interpreted results and edited the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Nikhil C. Munshi, VA Boston Healthcare System, Dana-Farber Cancer Institute, Harvard Medical School, Jerome Lipper Multiple Myeloma Center, 450 Brookline Ave, Boston, MA 02215; e-mail: nikhil_munshi@dfci.harvard.edu.
References
Author notes
Original data are available on request from Nikhil Munshi (nikhil_munshi@dfci.harvard.edu).
The full-text version of this article contains a data supplement.