Key Point
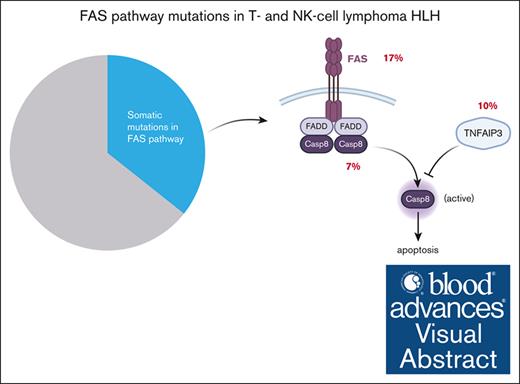
Somatic mutations in FAS pathway are associated with HLH in T- and/or natural killer–cell lymphoma.
Visual Abstract
Although significant progress has been made in understanding the genetic basis of primary hemophagocytic lymphohistiocytosis (HLH), the pathogenesis of secondary HLH, the more prevalent form, remains unclear. Among the various conditions giving rise to secondary HLH, HLH in patients with lymphoma (HLH-L) accounts for a substantial proportion. In this study, we investigated the role of somatic mutations in the pathogenesis of HLH-L in a cohort of patients with T- and/or natural killer–cell lymphoma. We identified a 3-time higher frequency of mutations in FAS pathway in patients with HLH-L. Patients harboring these mutations had a 5-time increased HLH-L risk. These mutations were independently associated with inferior outcome. Hence, our study demonstrates the association between somatic mutations in FAS pathway and HLH-L. Further studies are warranted on the mechanistic role of these mutations in HLH-L.
Introduction
Hemophagocytic lymphohistiocytosis (HLH) is a severe hyperinflammatory syndrome caused by abnormal systemic activation of macrophages and cytotoxic T cells.1 Primary (inherited/familial) HLH, most common in children, is caused by germline mutations affecting lymphocyte cytotoxicity and immune regulation.2,3 Secondary HLH (sHLH) usually affects adults and is commonly triggered by infections, malignancies, and/or other conditions, resulting in macrophage hyperactivation.3 Lymphoma is among the most frequent malignancies associated with HLH, with T- and/or natural killer (NK)-cell (T/NK-cell) lymphoma being more common than B-cell lymphoma.4,5 HLH-L has a poor prognosis, underscoring the need to improve the prediction and management of this condition.6,7 However, the pathogenesis of HLH-L remains poorly understood.6 Besides infections such as the Epstein-Barr virus (EBV), the underlying malignancy itself, and therapeutic interventions as known sHLH triggers, variants in genes involving familial HLH have recently been reported by a few groups in adult patients with sHLH, but the pathogenicity of these variants remains inconclusive,8-10 suggesting different pathogenesis between familial HLH and adult-onset sHLH.10 A recent study demonstrated high prevalence of clonal hematopoiesis in sHLH,11 implicating that somatic mutations in blood cells may lead to hyperinflammatory responses, a critical feature of HLH. There is lack of studies on the association between somatic mutations in neoplastic cells and sHLH. Germline and somatic FAS mutations, which lead to defective activation-induced cell death and the accumulation of self-reactive T cells, are the most common cause of autoimmune lymphoproliferative syndrome (ALPS).12-14 ALPS and HLH have many overlapping clinical and laboratory features,15 raising the possibility of a shared etiology, for example, FAS mutations. In this study, we set out to investigate the frequency of somatic mutations including FAS and its association with sHLH in patients with T/NK-cell lymphomas.
Methods and patients
Patients
The pathology archives between January 2016 and August 2023 at Memorial Sloan Kettering (MSK) Cancer Center were searched to identify patients with a diagnosis of a T/NK-cell lymphoma/lymphoproliferative disorder (LPD). The key words “non-Hodgkin” or “NK cell lymphoma or leukemia” or “T cell lymphoma (TCL)” or “mature T cell lymphoma” or “atypical NK cell” or “atypical T cell” or “T cell LPD” were used to identify patients. Only patients who had next-generation sequencing (NGS) studies with matched germline DNA control for analysis (see below) were further reviewed. A detailed chart review was performed to obtain clinical and laboratory parameters, to confirm the diagnosis and to identify patients with HLH. Diagnosis of HLH was made according to the HLH-2004 criteria.16 In addition, a positive or negative optimized HLH inflammatory (OHI) index17 based on elevated soluble CD25 (>3900 U/mL) and ferritin (>1000 ng/mL) was also assigned to each patient at the time of their lymphoma diagnosis or during treatment courses. Informed consent was obtained from patients. This study was approved by the MSK Institutional Review Board.
NGS and analysis
Mutational profiling was performed on formalin-fixed, paraffin–embedded lymphoma tissues (bone marrow or peripheral blood for patients with leukemia) by a targeted NGS panel MSK Integrated Mutational Profiling of Actionable Cancer Targets (MSK-IMPACT).18 Nail DNA was collected as a germline control. However, germline analysis was not permitted in this study. To evaluate the pathogenicity, somatic variants were classified as oncogenic, likely oncogenic, or variant of unknown significance as assessed according to the Clinical Genome Resource, Cancer Genomics Consortium, and Variant Interpretation for Cancer Consortium guidelines. The impact of missense variants was further evaluated by Polyphen-2 and sorting intolerant from tolerant (SIFT).19,20
Immunohistochemistry studies
Staining was performed on the Leica Bond-3 auto staining system (Leica, Deer Park, IL), using enzymatic digestion as pretreatment (AR9551; 10 minutes; Enzyme 1, Bond Enzyme Pre-treatment Kit, Leica), 30-minute primary incubation time, and a polymer detection system (DS9800; Bond Polymer Refine Detection, Leica). FAS antibody used is clone LT95 (NB500-503, Novus) with the dilution of 1:200 and the final concentration of 5 mg/mL.
Statistical analysis
Patient characteristics were summarized by frequency (percentage) or medians with interquartile range. Associations between mutation frequencies and disease characteristics were tested by Fisher exact test, Pearson χ2 test, and Wilcoxon rank sum test. Cumulative incidence curves for time-to-HLH diagnosis from lymphoma diagnosis were estimated with a death as competing event and left truncation at the date of genomic testing. Associations with genetic and clinical characteristics and risk of HLH were assessed using cause-specific Cox proportional hazards model. Overall survival (OS) from the time of HLH testing, with left truncation at date of genomic testing, was evaluated by Kaplan-Meier method, and the difference between groups were determined by Cox proportional hazards models. OS from the time of lymphoma diagnosis, with left truncation at date of genomic testing, was also evaluated by Kaplan-Meier method, and the differences between groups were determined by Cox proportional hazards models. All statistical analyses were performed using R 4.3.2.
Results
HLH in patients with T- and NK-cell lymphoma
In total, 433 patients were included in this study meeting the following criteria: carrying a diagnosis of T/NK-cell lymphoma or LPD, and having matched MSK-IMPACT analysis on neoplastic cells (supplemental Table 1). HLH was diagnosed in 29 patients (6.7%; 17 men and 12 women; median age, 60 years) based on 2004 criteria, none of whom were after hematopoietic stem cell transplant. These patients included angioimmunoblastic T-cell lymphoma (AITL; 2/89 [2.2%]), peripheral T-cell lymphoma, not otherwise specified (PTCL, NOS; 13/78 [16.7%]), anaplastic large cell lymphoma (ALCL; 2/47 [4.3%]), large granular lymphocytic leukemia (LGLL; 3/46 [6.5%]), adult T-cell leukemia/lymphoma (ATLL; 2/25 [8.0%]), extranodal T/NK-cell lymphoma (ENKTL; 1/12 [8.3%]), hepatosplenic T-cell lymphoma (2/7 [28.6%]), aggressive NK-cell leukemia (ANKL; 2/3 [66.7%]), mycosis fungoides/Sézary syndrome (1/62 [1.6%]), and other types of cutaneous T-cell lymphoma (CTCL; 1/19 [5.3%]). Notably, HLH was not found in patients with T-prolymphocytic leukemia (T-PLL; 0/23 [0%]) and intestinal T-cell lymphoma (0/11 [0%]). HLH was diagnosed at a median of 9.4 months (interquartile range, 3.5-15.8) after the diagnosis of lymphoma. Of the 29 patients, 27 had markedly increased soluble CD25 (>10 000 pg/mL), and 28 had ferritin levels >1000 ng/mL.17 EBV reactivation was detected in 17 cases at or before the onset of HLH (Table 1). Of the 29 patients with positive HLH, 28 patients succumbed to disease with a median survival of 22 days (95% confidence interval [CI], 13-60) after HLH diagnosis (supplemental Figure 1). Because the OHI index may be more sensitive for identifying malignancy-associated HLH,17 we also evaluated OHI index in our cohort. Forty-nine patients were positive for OHI index (OHI-positive), and 28 of them also met the 2004 criteria (supplemental Table 2). Patients meeting either the 2004 criteria or OHI index were both associated with inferior OS (supplemental Figure 1).
Clinicopathologic characteristics of patients with HLH and/or FAS mutations
| PID . | HLH . | FAS mutation . | Mutation significance∗ . | VAF . | IHC . | LOH . | Age . | Sex . | Lymphoma subtypes . | ALC, K/mL . | HLH, mo . | Death, mo . | Hemophagocytosis . | EBV titer, IU/mL . | sIL2R, pg/mL . | Ferritin, ng/mL . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Yes | No | NA | NA | ND | NA | 19 | F | ENKTL | 0.8 | 3 | 3 | No | >800 000 | 10 997 | 135 680 |
| 2 | Yes | No | NA | NA | ND | NA | 53 | M | ATLL | 2.8 | 1 | 1 | No | 7966 | >20 000 | 123 756 |
| 3 | Yes | No | NA | NA | ND | NA | 69 | M | AITL | 0.2 | 8 | 9 | Yes | 0 | >20 000 | 19 962 |
| 4 | Yes | No | NA | NA | ND | NA | 23 | M | HSTCL | 1.9 | 5 | 5 | No | <400 | >80 000 | 30 529 |
| 5 | Yes | No | NA | NA | ND | NA | 48 | F | HSTCL | 3.3 | 15 | 16 | No | 0 | >20 000 | 54 647 |
| 6 | Yes | No | NA | NA | ND | NA | 62 | M | PTCL, NOS | 0.1 | 1 | 12 | Yes | 0 | 14 250 | 5463 |
| 7 | Yes | No | NA | NA | ND | NA | 69 | F | PTCL, NOS | 0.5 | 6 | 7 | No | 0 | 19 525 | 47 693 |
| 8 | Yes | No | NA | NA | ND | NA | 61 | F | PTCL, NOS | 0.1 | 18 | 18 | No | 7313 | 6699 | 140 740 |
| 9 | Yes | No | NA | NA | ND | NA | 16 | M | PTCL, NOS | 0.3 | 1 | alive | Yes | 0 | >20 000 | 11 782 |
| 10 | Yes | No | NA | NA | ND | NA | 55 | F | PTCL, NOS | 0.4 | 12 | 13 | Yes | 3105 | 18 355 | 13 393 |
| 11 | Yes | No | NA | NA | ND | NA | 65 | M | PTCL, NOS | 6.7 | 7 | 8 | No | 0 | >20 000 | 19 502 |
| 12 | Yes | No | NA | NA | ND | NA | 59 | M | PTCL, NOS | 0.3 | 22 | 22 | No | 12 408 | >20 000 | 5547 |
| 13 | Yes | No | NA | NA | ND | NA | 62 | M | PTCL, NOS | 34.3 | 9 | 9 | ND | 2333 | >20 000 | 17 800 |
| 14 | Yes | No | NA | NA | ND | NA | 54 | M | PTCL, NOS | 0.6 | 1 | 1 | Yes | 0 | 38 945 | 42 659 |
| 15 | Yes | No | NA | NA | ND | NA | 77 | M | PTCL, NOS | 0.8 | 5 | 8 | No | 6621 | >20 000 | 21 966 |
| 16 | Yes | No | NA | NA | ND | NA | 72 | M | PTCL, NOS | 0.7 | 17 | 18 | Yes | 0 | >20 000 | 9246 |
| 17 | Yes | No | NA | NA | ND | NA | 61 | F | PTCL, NOS | 0.2 | 6 | 14 | No | <400 | >20 000 | 8906 |
| 18 | Yes | No | NA | NA | ND | NA | 64 | F | T-LGLL | 1.2 | 13 | 15 | No | 3214 | 8989 | 4021 |
| 19 | Yes | No | NA | NA | ND | NA | 69 | M | T-LGLL | 0.5 | 14 | 17 | Yes | <400 | >20 000 | 27 328 |
| 20 | Yes | No | NA | NA | ND | NA | 71 | M | T-LGLL | 0.5 | 12 | 13 | Yes | 1683 | 10 975 | 82 206 |
| 21 | Yes | No | NA | NA | ND | NA | 56 | F | MF | 1.0 | 16 | 16 | No | <400 | >20 000 | 2282 |
| 22 | Yes | No | NA | NA | ND | NA | 68 | F | CD8+ PCAETL | 0.5 | 42 | 42 | No | 3557 | >20 000 | 972 |
| 23 | Yes | No | NA | NA | ND | NA | 54 | F | ALCL | 3.1 | 12 | 12 | Yes | 0 | >20 000 | 22 621 |
| 24 | Yes | No | NA | NA | ND | NA | 49 | M | ALCL | 0.3 | 79 | 80 | ND | 0 | >20 000 | 15 073 |
| 25 | Yes | L224∗ | Likely oncogenic | 0.42 | Pos | No | 68 | F | AITL | 0.4 | 25 | 27 | Yes | 5773 | >20 000 | 12 277 |
| 26 | Yes | W281∗ | Likely oncogenic | 0.41 | Neg | No | 57 | F | PTCL, NOS | 0.3 | 2 | 2 | No | 1356 | >20 000 | 64 718 |
| 27 | Yes | D260N | predicted damaging | 0.26 | Neg | ND | 47 | M | ATLL | 0.7 | 55 | 58 | No | 0 | >20 000 | 2286 |
| 28 | Yes | S230Lfs∗4 | predicted damaging | 0.05 | Neg | No | 67 | M | ANKL | 0.6 | 3 | 3 | Yes | 1408 | >20 000 | 20 597 |
| 29 | Yes | N264K | predicted damaging | 0.10 | Neg | No | 71 | M | ANKL | 0.1 | 0 | 10 | Yes | 0 | 38 866 | >33 500 |
| 30 | No | C135Vfs∗52 | Likely oncogenic | 0.03 | ND | No | 52 | M | MEITL | 2.2 | NA | alive | No | ND | ND | ND |
| 31 | No | V220Wfs∗3 | Likely oncogenic | 0.18 | Neg | Yes | 61 | F | PTCL, NOS | 0.5 | NA | alive | No | 0 | ND | ND |
| 32 | No | X218_splice | Likely oncogenic | 0.12 | ND | ND | 86 | F | PTCL, NOS | 0.3 | NA | 70 | No | ND | ND | ND |
| 33 | No | I233Yfs∗14 | Likely oncogenic | 0.21 | ND | ND | 68 | F | PTCL, NOS | 1.6 | NA | alive | No | 0 | ND | ND |
| 34 | No | N302Vfs∗57 | Likely oncogenic | 0.66 | ND | Yes | 75 | M | PTCL, NOS | 1.4 | NA | 49 | No | 0 | ND | ND |
| 35 | No | S230Efs∗2 | Likely oncogenic | 0.45 | Neg | No | 56 | M | PTCL, NOS | 4.5 | NA | 19 | No | 0 | ND | ND |
| 36 | No | X66_splice | Likely oncogenic | 0.12 | Neg | No | 82 | F | PTCL, NOS | 0.7 | NA | 9 | No | ND | ND | ND |
| 37 | No | E272I | predicted damaging | 0.07 | ND | Yes | 48 | M | PTCL, NOS | ND | NA | alive | No | ND | ND | ND |
| 38 | No | D269G | predicted damaging | 0.33 | ND | ND | 77 | F | PTCL, NOS | 1.6 | NA | 44 | No | 0 | ND | 1476 |
| 39 | No | L242Pfs∗5 | Likely oncogenic | 0.44 | Pos | No | 74 | M | ATLL | 99.8 | NA | 3 | No | 0 | >20 000 | 595 |
| 40 | No | E261V | predicted damaging | 0.37 | ND | ND | 74 | F | ATLL | NA | NA | alive | No | ND | ND | ND |
| 41 | No | G286A | predicted damaging | 0.25 | ND | ND | 65 | F | ATLL | 5.1 | NA | alive | No | ND | ND | ND |
| 42 | No | L298Yfs∗8 | Likely oncogenic | 0.77 | Pos | Yes | 86 | M | T-LGLL | 3.2 | NA | 8 | No | 0 | ND | ND |
| 43 | No | D260G | predicted damaging | 0.35 | ND | No | 68 | M | T-LGLL | 1 | NA | alive | No | ND | ND | ND |
| 44 | No | Q273∗ | Likely oncogenic | 0.09 | ND | No | 71 | M | T-LGLL | 0.6 | NA | alive | No | ND | ND | 484 |
| 45 | No | D265G | predicted damaging | 0.39 | ND | ND | 58 | M | ENKTL | 2.1 | NA | alive | No | 0 | ND | ND |
| 46 | No | N252D | predicted damaging | 0.12 | ND | ND | 80 | M | AITL | 1.1 | NA | alive | No | 0 | ND | 4138 |
| 47 | No | E150∗ | Likely oncogenic | 0.49 | Neg | Yes | 76 | M | PCGDTCL | 2.9 | NA | alive | No | ND | ND | 34 |
| 48 | No | C119Afs∗68 | Likely oncogenic | 0.03 | Neg | No | 41 | F | SS | 4.1 | NA | alive | No | 0 | ND | 239 |
| 49 | No | H142D | Predicted damaging | 0.97 | Neg | Yes | 81 | M | SS | 1.2 | NA | alive | No | ND | ND | ND |
| 50 | No | X66_splice | Likely oncogenic | 0.12 | ND | Yes | 62 | M | MF | 0.2 | NA | 19 | No | 0 | ND | 1674 |
| 51 | No | X226_splice | Likely oncogenic | 0.45 | ND | No | 65 | M | MF | 1.1 | NA | alive | No | 0 | ND | ND |
| 52 | No | F134_C135ins∗ | Likely oncogenic | 0.46 | Neg | Yes | 59 | F | T-PLL | 1.2 | NA | alive | No | ND | ND | ND |
| PID . | HLH . | FAS mutation . | Mutation significance∗ . | VAF . | IHC . | LOH . | Age . | Sex . | Lymphoma subtypes . | ALC, K/mL . | HLH, mo . | Death, mo . | Hemophagocytosis . | EBV titer, IU/mL . | sIL2R, pg/mL . | Ferritin, ng/mL . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Yes | No | NA | NA | ND | NA | 19 | F | ENKTL | 0.8 | 3 | 3 | No | >800 000 | 10 997 | 135 680 |
| 2 | Yes | No | NA | NA | ND | NA | 53 | M | ATLL | 2.8 | 1 | 1 | No | 7966 | >20 000 | 123 756 |
| 3 | Yes | No | NA | NA | ND | NA | 69 | M | AITL | 0.2 | 8 | 9 | Yes | 0 | >20 000 | 19 962 |
| 4 | Yes | No | NA | NA | ND | NA | 23 | M | HSTCL | 1.9 | 5 | 5 | No | <400 | >80 000 | 30 529 |
| 5 | Yes | No | NA | NA | ND | NA | 48 | F | HSTCL | 3.3 | 15 | 16 | No | 0 | >20 000 | 54 647 |
| 6 | Yes | No | NA | NA | ND | NA | 62 | M | PTCL, NOS | 0.1 | 1 | 12 | Yes | 0 | 14 250 | 5463 |
| 7 | Yes | No | NA | NA | ND | NA | 69 | F | PTCL, NOS | 0.5 | 6 | 7 | No | 0 | 19 525 | 47 693 |
| 8 | Yes | No | NA | NA | ND | NA | 61 | F | PTCL, NOS | 0.1 | 18 | 18 | No | 7313 | 6699 | 140 740 |
| 9 | Yes | No | NA | NA | ND | NA | 16 | M | PTCL, NOS | 0.3 | 1 | alive | Yes | 0 | >20 000 | 11 782 |
| 10 | Yes | No | NA | NA | ND | NA | 55 | F | PTCL, NOS | 0.4 | 12 | 13 | Yes | 3105 | 18 355 | 13 393 |
| 11 | Yes | No | NA | NA | ND | NA | 65 | M | PTCL, NOS | 6.7 | 7 | 8 | No | 0 | >20 000 | 19 502 |
| 12 | Yes | No | NA | NA | ND | NA | 59 | M | PTCL, NOS | 0.3 | 22 | 22 | No | 12 408 | >20 000 | 5547 |
| 13 | Yes | No | NA | NA | ND | NA | 62 | M | PTCL, NOS | 34.3 | 9 | 9 | ND | 2333 | >20 000 | 17 800 |
| 14 | Yes | No | NA | NA | ND | NA | 54 | M | PTCL, NOS | 0.6 | 1 | 1 | Yes | 0 | 38 945 | 42 659 |
| 15 | Yes | No | NA | NA | ND | NA | 77 | M | PTCL, NOS | 0.8 | 5 | 8 | No | 6621 | >20 000 | 21 966 |
| 16 | Yes | No | NA | NA | ND | NA | 72 | M | PTCL, NOS | 0.7 | 17 | 18 | Yes | 0 | >20 000 | 9246 |
| 17 | Yes | No | NA | NA | ND | NA | 61 | F | PTCL, NOS | 0.2 | 6 | 14 | No | <400 | >20 000 | 8906 |
| 18 | Yes | No | NA | NA | ND | NA | 64 | F | T-LGLL | 1.2 | 13 | 15 | No | 3214 | 8989 | 4021 |
| 19 | Yes | No | NA | NA | ND | NA | 69 | M | T-LGLL | 0.5 | 14 | 17 | Yes | <400 | >20 000 | 27 328 |
| 20 | Yes | No | NA | NA | ND | NA | 71 | M | T-LGLL | 0.5 | 12 | 13 | Yes | 1683 | 10 975 | 82 206 |
| 21 | Yes | No | NA | NA | ND | NA | 56 | F | MF | 1.0 | 16 | 16 | No | <400 | >20 000 | 2282 |
| 22 | Yes | No | NA | NA | ND | NA | 68 | F | CD8+ PCAETL | 0.5 | 42 | 42 | No | 3557 | >20 000 | 972 |
| 23 | Yes | No | NA | NA | ND | NA | 54 | F | ALCL | 3.1 | 12 | 12 | Yes | 0 | >20 000 | 22 621 |
| 24 | Yes | No | NA | NA | ND | NA | 49 | M | ALCL | 0.3 | 79 | 80 | ND | 0 | >20 000 | 15 073 |
| 25 | Yes | L224∗ | Likely oncogenic | 0.42 | Pos | No | 68 | F | AITL | 0.4 | 25 | 27 | Yes | 5773 | >20 000 | 12 277 |
| 26 | Yes | W281∗ | Likely oncogenic | 0.41 | Neg | No | 57 | F | PTCL, NOS | 0.3 | 2 | 2 | No | 1356 | >20 000 | 64 718 |
| 27 | Yes | D260N | predicted damaging | 0.26 | Neg | ND | 47 | M | ATLL | 0.7 | 55 | 58 | No | 0 | >20 000 | 2286 |
| 28 | Yes | S230Lfs∗4 | predicted damaging | 0.05 | Neg | No | 67 | M | ANKL | 0.6 | 3 | 3 | Yes | 1408 | >20 000 | 20 597 |
| 29 | Yes | N264K | predicted damaging | 0.10 | Neg | No | 71 | M | ANKL | 0.1 | 0 | 10 | Yes | 0 | 38 866 | >33 500 |
| 30 | No | C135Vfs∗52 | Likely oncogenic | 0.03 | ND | No | 52 | M | MEITL | 2.2 | NA | alive | No | ND | ND | ND |
| 31 | No | V220Wfs∗3 | Likely oncogenic | 0.18 | Neg | Yes | 61 | F | PTCL, NOS | 0.5 | NA | alive | No | 0 | ND | ND |
| 32 | No | X218_splice | Likely oncogenic | 0.12 | ND | ND | 86 | F | PTCL, NOS | 0.3 | NA | 70 | No | ND | ND | ND |
| 33 | No | I233Yfs∗14 | Likely oncogenic | 0.21 | ND | ND | 68 | F | PTCL, NOS | 1.6 | NA | alive | No | 0 | ND | ND |
| 34 | No | N302Vfs∗57 | Likely oncogenic | 0.66 | ND | Yes | 75 | M | PTCL, NOS | 1.4 | NA | 49 | No | 0 | ND | ND |
| 35 | No | S230Efs∗2 | Likely oncogenic | 0.45 | Neg | No | 56 | M | PTCL, NOS | 4.5 | NA | 19 | No | 0 | ND | ND |
| 36 | No | X66_splice | Likely oncogenic | 0.12 | Neg | No | 82 | F | PTCL, NOS | 0.7 | NA | 9 | No | ND | ND | ND |
| 37 | No | E272I | predicted damaging | 0.07 | ND | Yes | 48 | M | PTCL, NOS | ND | NA | alive | No | ND | ND | ND |
| 38 | No | D269G | predicted damaging | 0.33 | ND | ND | 77 | F | PTCL, NOS | 1.6 | NA | 44 | No | 0 | ND | 1476 |
| 39 | No | L242Pfs∗5 | Likely oncogenic | 0.44 | Pos | No | 74 | M | ATLL | 99.8 | NA | 3 | No | 0 | >20 000 | 595 |
| 40 | No | E261V | predicted damaging | 0.37 | ND | ND | 74 | F | ATLL | NA | NA | alive | No | ND | ND | ND |
| 41 | No | G286A | predicted damaging | 0.25 | ND | ND | 65 | F | ATLL | 5.1 | NA | alive | No | ND | ND | ND |
| 42 | No | L298Yfs∗8 | Likely oncogenic | 0.77 | Pos | Yes | 86 | M | T-LGLL | 3.2 | NA | 8 | No | 0 | ND | ND |
| 43 | No | D260G | predicted damaging | 0.35 | ND | No | 68 | M | T-LGLL | 1 | NA | alive | No | ND | ND | ND |
| 44 | No | Q273∗ | Likely oncogenic | 0.09 | ND | No | 71 | M | T-LGLL | 0.6 | NA | alive | No | ND | ND | 484 |
| 45 | No | D265G | predicted damaging | 0.39 | ND | ND | 58 | M | ENKTL | 2.1 | NA | alive | No | 0 | ND | ND |
| 46 | No | N252D | predicted damaging | 0.12 | ND | ND | 80 | M | AITL | 1.1 | NA | alive | No | 0 | ND | 4138 |
| 47 | No | E150∗ | Likely oncogenic | 0.49 | Neg | Yes | 76 | M | PCGDTCL | 2.9 | NA | alive | No | ND | ND | 34 |
| 48 | No | C119Afs∗68 | Likely oncogenic | 0.03 | Neg | No | 41 | F | SS | 4.1 | NA | alive | No | 0 | ND | 239 |
| 49 | No | H142D | Predicted damaging | 0.97 | Neg | Yes | 81 | M | SS | 1.2 | NA | alive | No | ND | ND | ND |
| 50 | No | X66_splice | Likely oncogenic | 0.12 | ND | Yes | 62 | M | MF | 0.2 | NA | 19 | No | 0 | ND | 1674 |
| 51 | No | X226_splice | Likely oncogenic | 0.45 | ND | No | 65 | M | MF | 1.1 | NA | alive | No | 0 | ND | ND |
| 52 | No | F134_C135ins∗ | Likely oncogenic | 0.46 | Neg | Yes | 59 | F | T-PLL | 1.2 | NA | alive | No | ND | ND | ND |
HLH represents months from TCL diagnosis to HLH diagnosis; and death represents months from TCL diagnosis to decease.
ALC, absolute lymphocyte counts; CD8+ PCAETL, Primary cutaneous CD8+ epidermotropic cytotoxic T-cell lymphoma; ENKTL, extranodal T/NK-cell lymphoma, nasal type; IHC, immunohistochemistry; LOH, loss of heterozygosity; MEITL, monomorphic epitheliotropic intestinal T-cell lymphoma; NA, not applicable; ND, not done/determined; Neg, negative; PCGDTCL, primary cutaneous gamma delta T-cell lymphoma; Pos, positive; T-LGLL, T-large granular lymphocytic leukemia; VAF, variant allelic frequency.
Mutations were classified as oncogenic, likely oncogenic, or variant of unknown significance (VUS) as assessed according to the Clinical Genome Resource, Cancer Genomics Consortium, and Variant Interpretation for Cancer Consortium guidelines. VUS were further evaluated by Polyphen 2 and SIFT. A score of Polyphen2 >0.9 and/or of SIFT <0.05 was deemed as damaging.
Somatic mutations in FAS pathway associated with HLH in patients with T- and NK-cell lymphoma
We evaluated the mutational landscape of T/NK-cell lymphoma in our cohort (Figure 1). The most frequently mutated genes were TET2, TP53, STAT3, ROHA, and DNMT3A. As expected, mutations in TET2, DNMT3A, and RHOA were highly prevalent in AITL, whereas STAT3 mutations were enriched in indolent TCL, mostly LGLL. Interestingly, TP53 mutations were present in nearly a third of PTCL, NOS.
Mutational profiles between patients with and without HLH. (A) Oncoprints (only top 30 mutated genes were shown). (B) Bar plots showing the comparison of mutations in various genes. (C) Illustration of mutations in FAS pathway; figure created with BioRender.com.
Mutational profiles between patients with and without HLH. (A) Oncoprints (only top 30 mutated genes were shown). (B) Bar plots showing the comparison of mutations in various genes. (C) Illustration of mutations in FAS pathway; figure created with BioRender.com.
To identify genetic alterations associated with increased HLH risk, mutational profiles were compared between patients with and without HLH (Figure 1A). The frequent mutated genes were TP53 (24.1%), TET2 (20.7%), FAS (17.2%), and HLA-A (13.8%) in patients with HLH and TET2 (27.7%), STAT3 (14.6%), TP53 (14.4%), and RHOA (13.9%) in patients without HLH. Importantly, FAS, HLA-A, CDKN1B, and CASP8 mutations were more frequent in patients with HLH than those without (P = .03; P = .01; P = .01; and P = .03, respectively; Figure 1B). The frequencies of STAT5B, RARA, and TNFAIP3 mutations were also borderline increased in patients with HLH (P = .09; P = .07; and P = 0.06, respectively). Notably, FAS, CASP8, and TNFAIP3 encode proteins critical for the FAS pathway (Figure 1C). Among patients with HLH, 27.6% had at least 1 mutation in the FAS pathway compared with 8.9% of patients without HLH (P = .004).
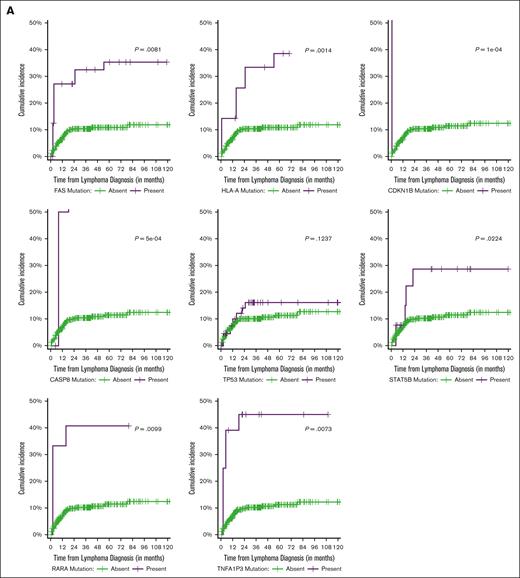
We next examined the association of gene mutations with HLH risk using univariable cause-specific Cox regression. Among all the patients undergoing HLH evaluation, we found an increased risk of HLH in patients harboring somatic mutations in FAS (hazard ratio [HR], 4.24; 95% CI, 1.46-12.4; P = .008), CASP8 (HR, 13.4; 95% CI, 3.14-57.5; P < .001), HLA-A (HR, 5.71; 95% CI, 1.96-16.6; P = .001), CDNK1B (HR, 19.2; 95% CI, 4.40-83.5; P < .001), STAT5B (HR, 3.45; 95% CI, 1.19-10.0; P = .022), TNFAIP3 (HR, 5.20; 95% CI, 1.56-17.4; P = .007), and RARA (HR, 6.72; 95% CI, 1.58-28.6; P = .010; Figure 2A; supplemental Table 3). Interestingly, TP53 mutations were not a risk factor for HLH. The presence of at least 1 mutation in FAS pathway genes (FAS, CASP8, and TNFAIP3) was significantly associated with increased HLH risk (HR, 4.98; 95% CI, 2.11-11.8; P < .001). HLH risk may be different between T- and NK-cell lymphoma subtypes.7 Indeed, after grouping the T/NK-cell lymphomas into 4 major categories (indolent TCL [LGLL, SS/MF/other CTCL, ALCL, and LPD], AITL, PTCL, NOS, and aggressive TCL [ANKL, ATLL, T-PLL, HSTCL, ENKTL, and intestinal TCL]), we demonstrated that PTCL, NOS appeared to be significantly associated with an increased risk of HLH (HR, 2.79; 95% CI, 1.06-7.35; P = .038; Figure 2B; supplemental Table 3). To disentangle these confounding factors, multivariable cause-specific time-to-HLH analysis was performed for each mutation, stratified by specific T-cell malignancy and adjusting for age and sex. To this end, we identified mutations in HLA-A, CDKN1B, CASP8, and TNFAIP3 as independent HLH risks (supplemental Table 4). The presence of at least 1 mutation involving the FAS pathway (FAS, CASP8, and TNFAIP3) was independently associated with increased HLH risk (HR, 3.56; 95% CI, 1.44-8.77; P = .006; supplemental Table 4). This association remained significant even when OHI criteria were applied (HR, 3.21; 95% CI, 1.48-6.93; P = .003).
Association of HLH risk by time-to-HLH (cumulative incidence) for patients undergoing complete HLH workup and mutations or specific T-cell malignancy. (A) Association between HLH risk and mutations of FAS, CASP8. HLA-A, CDKN1B, TP53, TNFA1P3, RARA, and STAT5B. (B) Association between HLH risk and specific T-cell malignancy.
Association of HLH risk by time-to-HLH (cumulative incidence) for patients undergoing complete HLH workup and mutations or specific T-cell malignancy. (A) Association between HLH risk and mutations of FAS, CASP8. HLA-A, CDKN1B, TP53, TNFA1P3, RARA, and STAT5B. (B) Association between HLH risk and specific T-cell malignancy.
Association between FAS pathway mutations and survival
We first evaluated clinical risk factors associated with OS. Univariable analysis identified both HLH and lymphoma subtypes as poor risk factors, whereas age, sex, or EBV status were not (supplemental Table 5). Because an increased risk of HLH was associated with multiple mutations, the impacts of individual mutations on OS were also evaluated. Univariable OS analysis showed an association between inferior OS and mutations in TP53 (HR, 1.99; 95% CI, 1.36-2.93; P < .001), CASP8 (HR, 6.95; 95% CI, 2.54-19.05; P < .001), HLA-A (HR, 2.19; 95% CI, 1.18-4.07; P = .01), RARA (HR, 3.24; 95% CI, 1.43-7.36; P = .005), STAT5B (HR, 1.84; 95% CI, 1.04-3.25; P = .04; supplemental Figure 3), and CDKN1B (HR, 2.19; 95% Cl, 1.18-4.07; P = .013) (data not shown). Multivariable analysis, however, after stratification by lymphoma subtypes and adjusting for age and sex, showed that the association with inferior OS remained significant only for TP53 (HR, 1.7; 95% CI, 1.03-2.80; P = .037), CASP8 (HR, 5.44; 95% CI, 1.62-18.3; P = .006), and CDKN1B (HR, 16.2; 95% Cl, 3.11-84.4; P < .001; Table 2). Importantly, the presence of at least 1 mutation in FAS pathway genes (FAS, CASP8, and TNFAIP3) was still significantly associated with inferior OS in this multivariable model (HR, 1.91; 95% CI, 1.10-3.34; P = .022). The association between FAS pathway mutations and outcome was lost when stratified by HLH (data not shown), further validating the close interaction between FAS pathway mutations and HLH. However, the significance of TP53 mutations remained even after stratification by HLH. The findings, together with the significant association seen between other mutations and T-cell subtypes (supplemental Table 6), suggests the survival impact was largely determined by specific lymphoma subtypes, but mutations in FAS pathways and TP53 also carry independent risks for poor outcome.
Multivariable OS after HLH assessment for each mutation stratified by specific T-cell malignancy, adjusting for age and sex
| Characteristics . | Mutations . | n . | Event, n . | HR . | 95% CI . | P value . |
|---|---|---|---|---|---|---|
| FAS mutation | Absent | 187 | 98 | Ref. | Ref. | |
| Present | 19 | 11 | 1.66 | 0.87-3.16 | .12 | |
| HLA-A mutation | Absent | 195 | 100 | Ref. | Ref. | |
| Present | 11 | 9 | 1.82 | 0.88-3.78 | .11 | |
| CDKN1B mutation | Absent | 204 | 107 | Ref. | Ref. | |
| Present | 2 | 2 | 16.2 | 3.11-84.4 | <.001 | |
| CASP8 mutation | Absent | 203 | 106 | Ref. | Ref. | |
| Present | 3 | 3 | 5.44 | 1.62-18.3 | .006 | |
| TP53 mutation | Absent | 173 | 87 | Ref. | Ref. | |
| Present | 33 | 22 | 1.7 | 1.03-2.80 | .037 | |
| TET2 mutation | Absent | 139 | 75 | Ref. | Ref. | |
| Present | 67 | 34 | 1.10 | 0.63-1.91 | .7 | |
| STAT3 mutation | Absent | 181 | 99 | Ref. | Ref. | |
| Present | 25 | 10 | 0.61 | 0.32-1.19 | .15 | |
| STAT5B mutation | Absent | 191 | 98 | Ref. | Ref. | |
| Present | 15 | 11 | 1.29 | 0.66-2.51 | .5 | |
| ROHA mutation | Absent | 172 | 92 | Ref. | Ref. | |
| Present | 34 | 17 | 1.27 | 0.64-2.54 | .5 | |
| RARA mutation | Absent | 200 | 104 | Ref. | Ref. | |
| Present | 6 | 5 | 1.69 | 0.64-4.43 | .3 | |
| TNFA1P3 mutation | Absent | 198 | 105 | Ref. | Ref. | |
| Present | 8 | 4 | 1.78 | 1.63-5.04 | .3 | |
| KMT2D mutation | Absent | 191 | 99 | Ref. | Ref. | |
| Present | 15 | 10 | 1.37 | 0.70-2.09 | .4 | |
| DNMT3A mutation | Absent | 177 | 93 | Ref. | Ref. | |
| Present | 29 | 16 | 1.41 | 0.79-2.52 | .2 | |
| Any mutations involving FAS, CASP8, and TNFA1P3 | Absent | 179 | 93 | Ref. | Ref. | |
| Present | 27 | 16 | 1.91 | 1.10-3.34 | .022 | |
| No. of mutations involving FAS, CASP8, and TNFA1P3 | 0 | 179 | 93 | Ref. | Ref. | |
| 1 | 24 | 14 | 1.80 | 1.00-3.24 | .048 | |
| 2 | 3 | 2 | 3.45 | 0.79-15.0 | .10 |
| Characteristics . | Mutations . | n . | Event, n . | HR . | 95% CI . | P value . |
|---|---|---|---|---|---|---|
| FAS mutation | Absent | 187 | 98 | Ref. | Ref. | |
| Present | 19 | 11 | 1.66 | 0.87-3.16 | .12 | |
| HLA-A mutation | Absent | 195 | 100 | Ref. | Ref. | |
| Present | 11 | 9 | 1.82 | 0.88-3.78 | .11 | |
| CDKN1B mutation | Absent | 204 | 107 | Ref. | Ref. | |
| Present | 2 | 2 | 16.2 | 3.11-84.4 | <.001 | |
| CASP8 mutation | Absent | 203 | 106 | Ref. | Ref. | |
| Present | 3 | 3 | 5.44 | 1.62-18.3 | .006 | |
| TP53 mutation | Absent | 173 | 87 | Ref. | Ref. | |
| Present | 33 | 22 | 1.7 | 1.03-2.80 | .037 | |
| TET2 mutation | Absent | 139 | 75 | Ref. | Ref. | |
| Present | 67 | 34 | 1.10 | 0.63-1.91 | .7 | |
| STAT3 mutation | Absent | 181 | 99 | Ref. | Ref. | |
| Present | 25 | 10 | 0.61 | 0.32-1.19 | .15 | |
| STAT5B mutation | Absent | 191 | 98 | Ref. | Ref. | |
| Present | 15 | 11 | 1.29 | 0.66-2.51 | .5 | |
| ROHA mutation | Absent | 172 | 92 | Ref. | Ref. | |
| Present | 34 | 17 | 1.27 | 0.64-2.54 | .5 | |
| RARA mutation | Absent | 200 | 104 | Ref. | Ref. | |
| Present | 6 | 5 | 1.69 | 0.64-4.43 | .3 | |
| TNFA1P3 mutation | Absent | 198 | 105 | Ref. | Ref. | |
| Present | 8 | 4 | 1.78 | 1.63-5.04 | .3 | |
| KMT2D mutation | Absent | 191 | 99 | Ref. | Ref. | |
| Present | 15 | 10 | 1.37 | 0.70-2.09 | .4 | |
| DNMT3A mutation | Absent | 177 | 93 | Ref. | Ref. | |
| Present | 29 | 16 | 1.41 | 0.79-2.52 | .2 | |
| Any mutations involving FAS, CASP8, and TNFA1P3 | Absent | 179 | 93 | Ref. | Ref. | |
| Present | 27 | 16 | 1.91 | 1.10-3.34 | .022 | |
| No. of mutations involving FAS, CASP8, and TNFA1P3 | 0 | 179 | 93 | Ref. | Ref. | |
| 1 | 24 | 14 | 1.80 | 1.00-3.24 | .048 | |
| 2 | 3 | 2 | 3.45 | 0.79-15.0 | .10 |
FAS mutations in patients with T- and NK-cell lymphoma
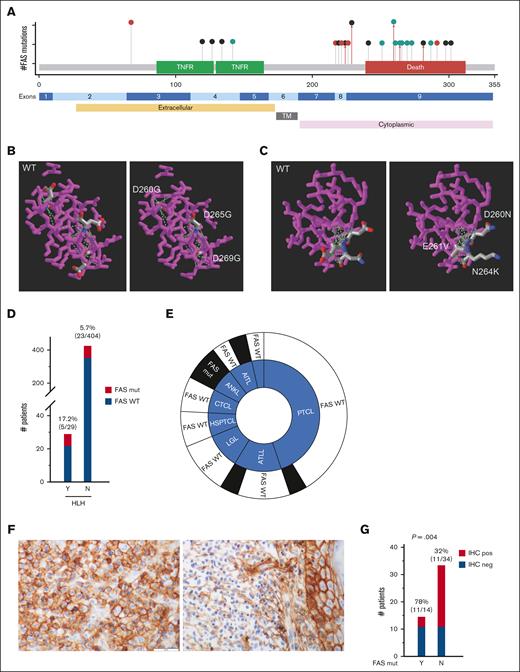
Because FAS appears frequently mutated in T- and NK-cell lymphoma, we decided to further evaluate the clinicopathologic features of patients with FAS mutations. FAS mutations were identified in 28 patients (19 men and 9 women; median age, 66 years), with an overall frequency of 6.5% (Figure 1A; Table 1). These 28 patients included AITL (2/89 [2.2%]), PTCL, NOS (9/78 [11.5%]), ATLL (4/25 [16.0%]), ENKTL (1/12 [8.3%]), LGLL (3/46 [6.5%]), ANKL (2/3 [66.7%]), T-PLL (1/23 [4.3%]), intestinal T-cell lymphoma (1/11 [9.1%]), and mycosis fungoides/Sézary syndrome/CTCL (5/81 [6.2%]). Interestingly, the prevalence of FAS mutations in PTCL, NOS was significantly higher than that in AITL (P = .02). FAS mutations were not identified in ALCL and hepatosplenic T-cell lymphoma. Seventeen of these 28 patients had a nodal biopsy, and none showed features suggestive of ALPS. Nineteen patients had documented flow cytometric analysis on peripheral blood, and none showed CD4/CD8 double negative TCR alpha/beta positive T cells >1.5% of lymphocytes or 2% of total T cells. Fifteen mutations were nonsense or frameshift, predicted to cause decreased/absent protein expression, thus deemed as likely oncogenic (Figure 3A). Ten patients had missense mutations, mostly involving death domain, and initially deemed as variant of unknown significance. Further evaluation predicted these 10 missense mutations to be damaging by Polyphen 2 (score > 0.9), SIFT (score < 0.05), and 3-dimensional structural modeling (Figure 3B-C; supplemental Table 7). Several amino acids affected by these mutations are highly conserved in evolution (supplemental Figure 4). The variant allelic frequency ranged from 0.03 to 0.97 (median, 0.30 ± 0.09). Because all patients had nail DNA as germ line control, these mutations were deemed as somatic. By reviewing NGS data, loss of heterozygosity of FAS mutations was identified in 8 patients, with variant allelic frequency ranging from 0.07 to 0.97 (Table 1).
FAS mutations in patients with T- and NK-cell lymphoma. (A) Lollipop illustration of FAS mutations in protein coding sequence (modified from cBioPortal). Red circle represents nonsense mutations; black circle represents frameshift mutations; and green circle represents missense mutations. Red arrowed line represents mutations identified in patients with HLH (only 1 patient with D260N or N264K mutations had HLH). (B-C) 3-dimensional modeling showing the amino acid changes of several representative missense mutations (https://www.ncbi.nlm.nih.gov/Structure/pdb/3OQ9). (D) Graphic illustration of the frequency of FAS mutations in patients with HLH. (E) The distribution of patients with HLH related to FAS mutations and the types of T/NK-cell lymphoma. (F) Representative pictures of FAS immunohistochemical staining in patients with T-cell lymphoma with wild-type FAS (left) and mutant FAS (right). Original magnification, 400×; scale bar, 50 mm. (G) Summary of FAS immunohistochemical staining in 48 patients with and without FAS mutations. IHC, immunohistochemistry; Mut, mutated; N, no; neg, negative; pos, positive; Y, yes.
FAS mutations in patients with T- and NK-cell lymphoma. (A) Lollipop illustration of FAS mutations in protein coding sequence (modified from cBioPortal). Red circle represents nonsense mutations; black circle represents frameshift mutations; and green circle represents missense mutations. Red arrowed line represents mutations identified in patients with HLH (only 1 patient with D260N or N264K mutations had HLH). (B-C) 3-dimensional modeling showing the amino acid changes of several representative missense mutations (https://www.ncbi.nlm.nih.gov/Structure/pdb/3OQ9). (D) Graphic illustration of the frequency of FAS mutations in patients with HLH. (E) The distribution of patients with HLH related to FAS mutations and the types of T/NK-cell lymphoma. (F) Representative pictures of FAS immunohistochemical staining in patients with T-cell lymphoma with wild-type FAS (left) and mutant FAS (right). Original magnification, 400×; scale bar, 50 mm. (G) Summary of FAS immunohistochemical staining in 48 patients with and without FAS mutations. IHC, immunohistochemistry; Mut, mutated; N, no; neg, negative; pos, positive; Y, yes.
In total, 5 of 28 (17.9%) patients carrying FAS mutations (all locating at cytoplasmic portion) developed HLH compared with only 24 of 405 patients (5.9%) without FAS mutations (P = .03; Figure 3D-E; Table 1). FAS mutations were not detected in any of the 21 patients who were OHI-positive but did not meet 2004 criteria. Relatedly, there was no significant association between FAS mutations and OHI index status (HR, 2.39; 95% CI, 0.85-6.74; P = .1).
Because most somatic FAS mutations in our cohort were nonsense or frameshift, it would predict decreased or absent FAS protein expression levels. To test this, immunohistochemical stain using anti-FAS antibody was performed on formalin-fixed, paraffin-embedded tissues of 48 patients, obtained from our archives (Figure 3F). FAS protein expression was absent in 11 of 14 patients (78%) with FAS mutations. In contrast, only 9 of 34 patients (32%) with no FAS mutation had loss of FAS protein expression (P = .004; Figure 3G). There appeared no correlation between FAS protein expression and types of mutations.
Discussion
Our study demonstrated a previously unrecognized association between FAS pathway mutations and HLH-L in patients with T/NK-cell lymphoma. The etiology of HLH-L may be multifactorial including EBV infection, chemotherapy-related injury, and genetic susceptibility. Our study identified somatic, pathogenic mutations in FAS pathway overrepresented in patients with HLH-L, suggesting acquired genetic susceptibility as an underlying etiology. Notably, 28 of 29 patients developed HLH after treatment, and many of them had EBV and/or other viral infections, suggesting a possible intricate interplay between genetic alterations, viral infection, and chemotherapy, and more studies are warranted for better understanding the underlying mechanisms. A recent study has shown somatic mutations in TET2 in blood cells are more prevalent in patients with sHLH and may contribute to sHLH by inducing hyperactivation of macrophages.11 Our study showed comparably frequent TET2 mutations in T/NK-cell lymphoma in both patients with HLH and those with non-HLH. Notably, mutations in several genes (FAS, CASP8, and TNFAIP3) identified in our cohort are implicated in FAS pathways. It will be interesting to study whether these somatic mutations in lymphoma cells also lead to dysregulation of immune response, including macrophage hyperactivation.21
Both germline and somatic FAS mutations are characteristic of ALPS.13,14,22,23 Patients with ALPS have increased risks of lymphoma.24 Because ALPS and HLH share some clinical and laboratory features, the presence of somatic FAS mutations in T/NK-cell lymphoma in our cohort raises the possibility of an underlying, undiagnosed ALPS in these patients. However, several lines of evidence argue against this. First, patients with ALPS with germline FAS mutations are mostly aged <5 years, and those with somatic FAS mutations are aged <20 years, with only rare exceptions.22,23 Our cohort with FAS mutations were mostly aged >50 years. Second, CD4/CD8 double negative TCR alpha/beta positive T cells, characteristic of ALPS, were not increased in our patients. Third, reviewing of histology did not show features suggestive of ALPS. Fourth, the patients with FAS mutations and HLH had extremely high levels of sCD25 (>20 000 pg/mL) and serum ferritin (>10 000 ng/mL), which is very rare in ALPS.15,25
FAS/FASL pathway is essential for the downregulation of immune reactions as well as in T-cell–mediated cytotoxicity via inducing apoptosis.26 Mutations in FAS or FASL lead to defective apoptosis and lymphoproliferation in ALPS.13,14 It is conceivable to speculate that loss-of-function mutations along this pathway in our cohort provides survival advantage in lymphoma cells. However, the mechanistic link between these mutations in lymphoma and HLH is yet to be established. FAS/FASL signaling pathway may regulate the activation of macrophages.27 The interplay between mutated lymphoma cells and macrophages warrants further studies.
We identified mutations in TP53 and FAS pathway as independent risk factors for poor outcomes. TP53 mutations has been previously shown to correlate with inferior progression-free survival in patients with PTCL treated with chemotherapy.28 Intriguingly, TP53 mutations were not associated with HLH, and the prognostic significance was not affected by HLH stratification in patients with T- and NK-cell lymphoma. In comparison, the prognostic value of mutations in FAS pathways was lost after HLH stratification. Therefore, we posit that TP53 mutations lead to inferior outcome by conferring therapeutic resistance to chemotherapy, whereas FAS pathway mutations do this by increasing HLH risk. These pieces of evidence collectively support that genetic information may be incorporated into current risk-stratification models in clinical practice for these patients.29,30
One major caveat of our study is the lack of germline analysis to exclude the rare possibility of coexisting germ line FAS and other primary HLH-related mutations in these patients. Although these germline mutations may not be sufficient to induce sHLH as suggested by a recent study,10 they may collaborate with somatic mutations. In addition, other germline mutations such as Hepatitis A virus cellular receptor 2/T-cell immunoglobulin and mucin-domain containing-3 (TIM-3), commonly seen in subcutaneous panniculitis-like TCL, resulting in loss of TIM-3 protein function, may lead to macrophage activation and HLH.31 Second, due to the retrospective in nature, our study might have underestimated the frequency of HLH, despite extensive manual chart review being performed. Third, the median survival of our patients was only 25 days after the diagnosis of HLH, indicating an extremely poor prognosis. However, the possibility of a delayed diagnosis cannot be ruled out because an early, accurate diagnosis of HLH has been very challenging. Nevertheless, this study sheds new light on the potential clinical relevance of somatic mutations in the FAS pathway in HLH-L and calls for further investigations and eventually the development of methods for early diagnosis and targeted therapeutic approaches for these patients at high risk.
Acknowledgments
This study was funded in part through the National Institutes of Health (NIH)/National Cancer Institute (NCI) Cancer Center Support grant P30 CA008748. W.X. is supported by Alex’s Lemonade Stand Foundation and the Runx1 Research Program, a Cycle for Survival’s Equinox Innovation Award in Rare Cancers, MSK Leukemia SPORE (Career Enhancement Program, NIH/NCI P50 CA254838-01), and a NCI grant (K08CA267058-01).
Authorship
Contribution: Y.L. and R.S. compiled and annotated the patient cohort; Y.L. and M.A. annotated the mutations; D.N. and A. Derkach performed statistical analyses; W.T.J., S.V., and S.M.H. provided clinical information; A. Dogan helped the pathology and provided guidance; W.X. designed and supervised the study; Y.L., R.S., and W.X. wrote the manuscript; and all authors approved the manuscript.
Conflict-of-interest disclosure: W.T.J. received consulting fees from Myeloid Therapeutics. S.V. served on the advisory board for Immunai and received consulting fees from ADC Therapeutics and Koch Disruptive Technologies. S.M.H. received research funding from ADC Therapeutics, Affimed, Aileron, Celgene, CRISPR Therapeutics, Daiichi Sankyo, Forty Seven Inc, Kyowa Hakko Kirin, Millennium/Takeda, Seattle Genetics, Trillium Therapeutics, and Verastem/SecuraBio, and consulting fees from Acrotech Biopharma, ADC Therapeutics, Astex, Auxilus Pharma, Merck, C4 Therapeutics, Celgene, Cimieo Therapeutics, Daiichi Sankyo, Janssen, Kura Oncology, Kyowa Hakko Kirin, Myeloid Therapeutics, ONO Pharmaceuticals, Seattle Genetics, SecuraBio, Shoreline Biosciences Inc, Takeda, Trillium Therapeutics, Tubulis, Verastem/SecuraBio, Vividion Therapeutics, and Yingli Pharma Ltd. A. Dogan served as a consultant for Incyte, EUSA Pharma, and Loxo, and receives research support from Roche and Takeda. W.X. received research support from Stemline Therapeutics. The remaining authors declare no competing financial interests.
The current affiliation for R.S. is Sardana Labs, Punjab, India.
Correspondence: Wenbin Xiao, Department of Pathology and Laboratory Medicine, Memorial Sloan Kettering Cancer Center, 1275 York Ave, New York, NY 10065; email: xiaow@mskcc.org.
References
Author notes
Additional data and materials are available on request from the corresponding author, Wenbin Xiao (xiaow@mskcc.org).
The full-text version of this article contains a data supplement.