TO THE EDITOR:
Chimeric antigen receptor (CAR) T-cell therapy directed toward CD19 for B-cell malignancies often results in cytokine release syndrome (CRS). CRS typically occurs in the first week and is characterized by increased proinflammatory cytokines and symptoms such as fever, headache, and nausea, in some cases progressing to hypotension, hypoxia, and multiorgan failure.1-3 Prediction of CRS, as well as a better understanding of the mechanisms leading to CRS onset, remain important unmet needs to improve outcomes of CAR T-cell therapy. However, aside from the known set of cytokines associated with CRS, current understanding of CRS mechanisms and biomarkers for early prediction remains limited.3,4
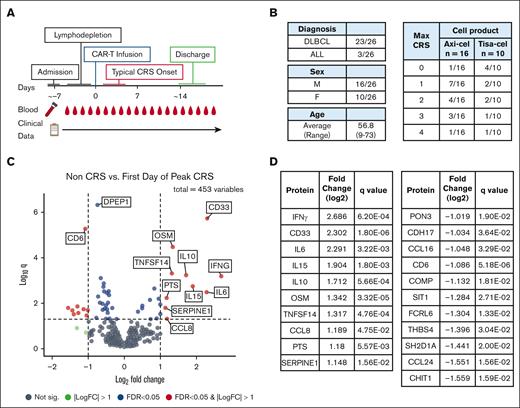
To discover novel plasma proteins associated with CRS, we used a proximity ligation–based high-throughput proteomics screening approach (Olink Proteomics) to analyze 453 protein biomarkers in longitudinal plasma samples from 26 patients receiving CD19 CAR T-cell therapies, 21 of whom developed CRS. Blood samples were collected at baseline (ie, before CAR T-cell infusion), on the day of CAR T-cell infusion, and on multiple days throughout the inpatient hospitalization (∼2 weeks; Figure 1A). Matched demographic and clinical data (eg, daily CRS grading scores) were collected from the electronic health record (Figures 1A and B; supplemental Table 1). We then used differential expression analyses and linear mixed models to identify novel proteins that were elevated during CRS, proteins that may predict CRS at baseline, and proteins in plasma that showed changes over time specific to patients who developed CRS.
Study design and differential protein expression at peak CRS. Overview of the study design and results of the differential expression analysis. (A) Schematic depicting the course of treatment and data types collected. (B) Patient demographics and the maximum grades of CRS experienced. The median time to onset of CRS was 2 days (with interquartile range, 1-7 days). The median time to onset of the peak CRS grade was 5 days (with inter-quartile range of 2-10 days). (C) Volcano plot of proteins significantly up and down regulated at peak CRS compared to samples taken after CAR T-cell infusion from patients who never developed CRS, with dotted lines to distinguish between points with an absolute fold change >2 or <2 and a q-value < 0.05. (D) Table of proteins identified as significant in the volcano plot, with an absolute fold-change >2 or <2 and a q-value < 0.05. Axi-cel, axicabtagene ciloleucel; tisa-cel, tisagenlecleucel.
Study design and differential protein expression at peak CRS. Overview of the study design and results of the differential expression analysis. (A) Schematic depicting the course of treatment and data types collected. (B) Patient demographics and the maximum grades of CRS experienced. The median time to onset of CRS was 2 days (with interquartile range, 1-7 days). The median time to onset of the peak CRS grade was 5 days (with inter-quartile range of 2-10 days). (C) Volcano plot of proteins significantly up and down regulated at peak CRS compared to samples taken after CAR T-cell infusion from patients who never developed CRS, with dotted lines to distinguish between points with an absolute fold change >2 or <2 and a q-value < 0.05. (D) Table of proteins identified as significant in the volcano plot, with an absolute fold-change >2 or <2 and a q-value < 0.05. Axi-cel, axicabtagene ciloleucel; tisa-cel, tisagenlecleucel.
To identify proteins elevated as part of CRS, we analyzed proteomics data to find those differentially abundant proteins in plasma of 21 patients at onset of peak CRS (ie, the first day of the highest CRS grade experienced by a given patient) as compared with that in postinfusion samples from 5 patients who did not develop CRS. This analysis identified multiple cytokines that are known to be elevated in CRS, including IFNγ, IL6, IL15, and IL10 (Figure 1C-D).2,4 However, 6 additional proteins were newly identified to be significantly increased at the onset of peak CRS, and 11 proteins were newly identified to be significantly decreased (Figure 1C and D; full results of differential abundance analysis are provided in supplemental Table 2).
Of note, the CD33 protein was a novel CRS protein that demonstrated an increase in abundance of magnitude comparable with that observed for IFNγ and IL6. Interestingly, CD33 is expressed on myeloid cells, notably neutrophils and monocytes, which crosstalk with other leukocytes via cytokine secretion and can be important regulators of inflammation.5,6 Monocytes express the cytokines IL-1 and IL-6 and have been shown to be crucial for development of CRS in animal models.7
To identify candidate biomarkers for predicting the occurrence of CRS incidence, the abundance levels of individual proteins at baseline were compared between patients who developed CRS and those who did not. Eleven proteins were found to have differential expression at baseline using a threshold of unadjusted P-value < .05 and absolute fold-change of ≥2.0 (supplemental Figure 1; supplemental Table 3).
Notably, 3 of these proteins, SERPINE1 (PAI-1), TNFSF11 (RANKL), and PON3 showed differential abundance at baseline with a q-value < 0.1 and represent candidate biomarkers for predicting CRS (supplemental Table 3; supplemental Figures 2-4). Elevated serum SERPINE1 (PAI-1) levels have been observed in patients with sepsis, ARDS, and COVID-19, but to our knowledge, this is the first identification of SERPINE1 (PAI-1) as a baseline predictor of CRS.8 SERPINE1 (PAI-1) is also a marker of endothelial activation, a process that appears to be important in the development of CRS.9 Interestingly, CD33 and 5 other proteins found to be elevated at the onset of peak CRS (discussed above), were among the list of 11 proteins differentially expressed at baseline in patients who went on to develop CRS (unadjusted P < .05 and absolute fold difference of ≥2; supplemental Table 3).
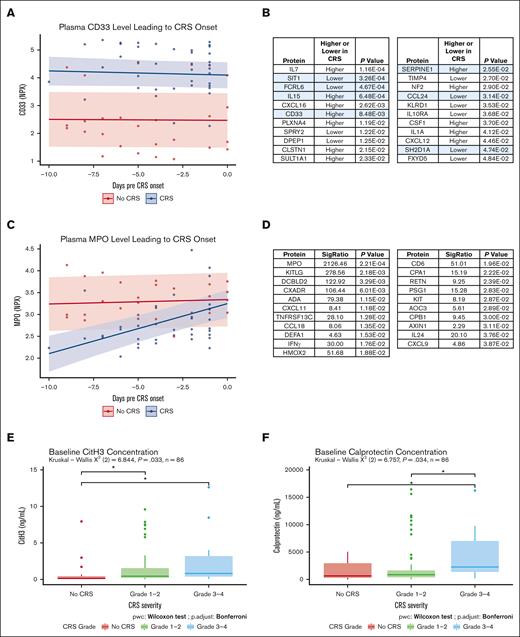
We next sought to evaluate whether the longitudinal dynamics of protein abundance might be associated with subsequent development of CRS using a linear mixed model analytic approach (supplemental Methods). In this analysis, we identified 43 proteins exhibiting differences in their abundance profile over time between patients who developed any grade of CRS and those who never developed CRS (Figure 2A-D; supplemental Table 4). This included identification of 22 of 43 proteins that showed stable over-time but different absolute levels of abundance between groups (Figure 2B). Of these, 7 corresponded to proteins that were also elevated at the time of peak CRS (shaded rows in Figure 2B), and included CD33, which was stably elevated in plasma over the entire period leading up to CRS onset (Figure 2A).
Longitudinal differences in protein expression and NETosis-related assays. Results from the longitudinal linear mixed model analysis (with prediction intervals calculated based on standard error), followed by protein expression assays. (A) CD33 expression after CAR T-cell infusion in participants (n = 22) leading up to CRS onset or leading up to day 7 to 9 in those without CRS. NPX represents normalized protein eXpression on a log2 scale (Olink Proteomics). (B) Table of proteins with a significant CRS term within the linear mixed model, indicating constitutively higher or lower expression levels over time leading to CRS onset. Light blue shading indicates proteins that were also found to be differentially abundant at peak CRS in Figure 1D. (C) MPO expression after CAR T-cell infusion in participants (n = 22) leading up to CRS onset or leading up to day 7 to 9 in those without CRS. NPX represents normalized protein eXpression on a log2 scale (Olink Proteomics). (D) Table of proteins with significant changes over time only in participants who developed CRS, as indicated by the interaction term CRS:time P-value and significance ratio (ratio of interaction term P-value/CRS term P-value). (E) Pre-CAR T–cell infusion CitH3 and (F) Calprotectin levels, measured using enzyme-linked immunosorbent assay, in participants (n = 86) who later developed various grades of CRS. For CitH3 levels from 8 patients, a linear regression–based rescaling was done to correct for a batch effect (see supplemental Methods for more detail).
Longitudinal differences in protein expression and NETosis-related assays. Results from the longitudinal linear mixed model analysis (with prediction intervals calculated based on standard error), followed by protein expression assays. (A) CD33 expression after CAR T-cell infusion in participants (n = 22) leading up to CRS onset or leading up to day 7 to 9 in those without CRS. NPX represents normalized protein eXpression on a log2 scale (Olink Proteomics). (B) Table of proteins with a significant CRS term within the linear mixed model, indicating constitutively higher or lower expression levels over time leading to CRS onset. Light blue shading indicates proteins that were also found to be differentially abundant at peak CRS in Figure 1D. (C) MPO expression after CAR T-cell infusion in participants (n = 22) leading up to CRS onset or leading up to day 7 to 9 in those without CRS. NPX represents normalized protein eXpression on a log2 scale (Olink Proteomics). (D) Table of proteins with significant changes over time only in participants who developed CRS, as indicated by the interaction term CRS:time P-value and significance ratio (ratio of interaction term P-value/CRS term P-value). (E) Pre-CAR T–cell infusion CitH3 and (F) Calprotectin levels, measured using enzyme-linked immunosorbent assay, in participants (n = 86) who later developed various grades of CRS. For CitH3 levels from 8 patients, a linear regression–based rescaling was done to correct for a batch effect (see supplemental Methods for more detail).
The remaining 21 proteins that were identified showed increasing or decreasing temporal dynamics leading up to CRS, in comparison with patients who did not experience CRS (Figure 2D). Among these, the myeloperoxidase protein (MPO) had the highest significance ratio and the lowest P-value (Figure 2C). MPO was lower at day 0 in the group experiencing CRS and demonstrated a rise to the time of CRS onset. MPO is specifically expressed in neutrophils and constitutes a major component of neutrophilic azurophilic granules.5,10 MPO is released upon activation of neutrophils, promoting increased inflammation as well as damage to the endothelium and tissues that may be relevant to promoting CRS.11,12 Furthermore, MPO is important for the release of neutrophil extracellular traps (NETs) and is a marker of NETosis.10,11 Interestingly, the values of MPO were not significantly different among the groups at baseline (supplemental Figure 5A). Because the majority of our baseline samples were collected before lymphodepleting chemotherapy, this may suggest that chemotherapy leads to a decline in MPO concentration preferentially in patients who later develop CRS (supplemental Figure 5B), with MPO increasing toward baseline levels in the days leading up to CRS onset.
Review of the other significantly altered proteins in the longitudinal analysis identified another neutrophil granule protein, DEFA1 (α defensin 1, also known as human neutrophil peptide 1 [HNP-1] or neutrophil defensin 1; supplemental Figure 6), as well as RETN, a marker of neutrophil activation (supplemental Figure 7), and DPEP1, a neutrophil adhesion receptor (supplemental Figure 8).11,13,14
Collectively, these findings led us to ask whether neutrophil activation, and the process of NETosis in particular, might be associated with development of CRS. We then used enzyme-linked immunosorbent assay to measure 2 additional markers of neutrophil activation and NETosis, citrullinated histone H3 (CitH3) and circulating calprotectin, which were not included in the Olink proteomic panels. CitH3 contributes to neutrophil chromatin decondensation during NETosis,12,15 and calprotectin is a heterodimer of S100A8 and S100A9 abundant in the neutrophil cytoplasm and released via NETosis.16 We measured these proteins in a larger cohort of baseline plasma samples (n = 86) collected from patients at the University of Michigan and Johns Hopkins Medicine receiving CAR T-cell therapies, predominantly targeting CD19 (supplemental Table 5). The results showed a significant elevation of CitH3 and calprotectin in patients who later developed CRS (Figure 2E and F). CitH3 was elevated in patients who went on to develop grade 1 to 2 or grade 3 to 4 CRS, with increased levels seen with grade 3 to 4, whereas calprotectin was elevated only in patients who went on to have grade 3 to 4 CRS. Longitudinal analysis of these markers, in a subset of patients for whom such samples were available, did not show a definitive change in their levels over time leading up to CRS (supplemental Figure 9).
In summary, our longitudinal plasma proteomic screen identified novel candidate biomarkers related to CRS prediction at baseline, during the time leading up to CRS, and during CRS itself. These candidate markers have potential to be developed as biomarkers for assessing CRS risk before CAR T-cell infusion or for earlier CRS detection and escalation of care. Prospective studies of these candidate biomarkers will be needed to validate our findings toward clinical use.
The elevation of plasma levels of neutrophil-associated proteins, including the NETosis markers CitH3 and calprotectin and their correlation to CRS incidence and grade, suggests that neutrophil dysregulation and overactivation may be an important new mechanism underlying the genesis and risk of CRS. To our knowledge, neutrophil activation and NETosis have not yet been reported in CAR T-cell therapy–associated CRS. If not contained or degraded, NETs can function as damage-associated molecular patterns to amplify inflammation.10,17,18 Excessive NETosis promotes inflammation and tissue damage in various infectious and autoimmune diseases.18-21 Indeed, recent research into COVID-19 pathogenesis suggests that NETs contribute to the cytokine storm that leads to respiratory failure in some patients with COVID-19 by promoting the release of cytokines, such as IL-1β and IL-6,22,23 and elevated calprotectin levels and increasing numbers of neutrophils have been associated with severe COVID-19 cases.24 In the case of CAR T-cell therapy–associated CRS, our data indicate that elevated NETosis-related signals occur before CAR T-cell infusion, suggesting that they may have predictive value as candidate biomarkers and may function to amplify the subsequent systemic inflammatory cascade leading to CRS. In future studies, examining the association between NETosis and traditional risk factors of CRS, such as tumor burden may help better characterize the role of NETosis in the development of CRS.
In conclusion, these findings have implications for the understanding and prediction of severe CRS, as well as potential new therapeutic targets. Our findings support the hypothesis that NETosis and neutrophil activity contribute to the mechanism of CRS development. This is particularly exciting because Food and Drug Administration–approved drugs that can inhibit neutrophil activation or NETosis are available,10 representing promising candidates for CRS prevention, which could be tested in clinical trials if this hypothesis is validated.
Acknowledgments: The authors thank Jenny Wolfgang for assistance with specimen processing, and Amanda Mazzoli and Kristen Gilley for assistance with clinical research coordination.
This work was supported by a Taubman Medical Institute Grand Challenge grant and a Taubman Medical Institute Innovation Project grant. S.W.C. is currently supported by NHLBI grants R01HL146354 and K24HL156896 (for mentoring) and NCI grant R01CA249211. C.F. was supported by an NHLBI T32 training grant (T32HL007622). C.B. is supported by St. Baldrick's Foundation and Hyundai Hope on Wheels Scholar Awards.
Contribution: M.O., E.S., and A.S. prepared blood samples; C.F., Y.Z., and K.S. performed experiments; C.F., M.O., R.M., and G.L. provided statistical guidance or analyzed data; M.R., A.L., and A.A.C. curated clinical data; Y.Z., G.A.Y., D.G.F., C.L.B., T.J., J.S.K., S.W.C., and M.T. conceived aspects of the study, obtained funding, oversaw specimen and clinical data collection, and/or interpreted results; Y.Z., D.G.F., C.L.B., T.J., J.S.K., S.W.C., and M.T. provided study guidance and oversight; M.J.G., G.A.Y., M.G., D.G.F., C.L.B., and T.J. provided clinical input and guidance; M.O., E.S., and M.T. wrote the manuscript; and all authors provided manuscript edits and approved the final manuscript.
Conflict-of-interest disclosure: M.T., S.W.C., C.F., Y.Z., J.S.K., and D.G.F. are inventors of a CRS biomarkers–related invention, for which the University of Michigan is pursuing patent protection. T.J. has participated in an advisory board with Kite Pharma. The remaining authors declare no competing financial interests.
Correspondence: Muneesh Tewari, 109 Zina Pitcher Pl, 1502 BSRB, SPC 2200, Ann Arbor, MI 48109; email: mtewari@med.umich.edu; and Sung Won Choi, 1500 E. Medical Center Dr, D4118 MPB, Ann Arbor, MI 48109; email: sungchoi@med.umich.edu.
References
Author notes
C.F. and M.O. contributed equally to this work.
Detailed results from the proteomics analyses are provided in the supplemental Materials. Additional data that support the findings of this study are available to investigators upon request to Muneesh Tewari (mtewari@med.umich.edu), contingent upon review and compliance with government regulatory requirements and University of Michigan policies.
The full-text version of this article contains a data supplement.