TO THE EDITOR:
T-cell lymphoblastic lymphoma (T-LBL) and T-cell acute lymphoblastic leukemia (T-ALL) represent malignancies of immature T cells. Clinical presentation of T-LBL and T-ALL differs, with patients with T-LBL mainly presenting with severe cardiorespiratory symptoms, whereas patients with T-ALL usually suffer from complaints related to leukocytosis and massive bone marrow (BM) infiltration. Relapsed T-LBL as well as T-ALL are associated with extreme poor prognosis.1,2 In the last decades, survival of children with T-ALL has improved through the implementation of treatment strategies based on minimal residual disease as well as high-risk genetics.3,4 Extensive research of risk factors in T-LBL has not been performed and minimal residual disease measurement has not been proven to be a usable stratification strategy yet. Pediatric patients with T-LBL are currently treated according to ALL-based strategies, which results in event-free survival in ∼80% of the patients.2 The high toxicity of treatment accompanied by considerable morbidity and mortality shows the urgent need for improved stratification and prognostic parameters. A good-prognostic risk group based on the presence of NOTCH1/FBXW7 mutations has been described, but the remaining group of T-LBL patients has a worse outcome.5,6 We recently discovered that NOTCH1 gene fusions represent a high-risk subgroup,8 but a comprehensive genomic comparison between pediatric T-LBL and T-ALL is still missing. Our study explores molecular genetic differences as well as similarities between T-ALL and T-LBL to increase further insight in the etiology of T-cell malignancies. By doing so, we aim to identify possible high-risk and low-risk profiles.
Pediatric patients with T-LBL diagnosed between 2010 and 2023 treated in the Netherlands were included in this study (n = 59). Informed written consent was obtained from all patients and/or their legal guardians (supplemental Material and Methods). The clinical characteristics of these unselected pediatric patients with T-LBL in this cohort are summarized in supplemental Table 1. The median age at diagnosis was 10 years (range, 0-17), and there were more males (63%) than females (37%). In almost all patients (93%) the mediastinum was enlarged and, based on radiology results, 71% of the patients presented with an enlarged lymph node in the head-neck region. Half of the patients (53%) presented with pleural effusion at diagnosis. Based on cytomorphological studies, 22% of the patients presented with BM involvement at time of diagnosis (5%-25% blasts). Six patients (10%) had a relapse and none of them survived. The overall survival rate of the patients in our cohort with a follow-up of at least 1 year after diagnosis was 84%. In order to study the mutational landscape, whole-exome sequencing was performed on either formalin-fixed paraffin embedded (FFPE) tumor biopsies, or fresh (frozen) tumor material (n = 44) combined with matching nonmalignant BM aspirations or peripheral blood (n = 38/44; supplemental Figure 1). In the latter group, we found a median tumor mutational burden of 0.42 mutations per megabase (Mb; range, 0.05-1.23; Figure 1A). The 5 most frequently mutated genes in our T-LBL cohort were NOTCH1, FBXW7, RPL10, PHF6, and BCL11B, which is in agreement with other studies.6 Chromosomal aberrations (>20 Mb) were found in 39% of patients in our T-LBL cohort, and recurrent gains were found on chromosome 10 (chr10), chr17q, and chr20. LOH6q was found in 16% of our cohort, compared to 19% in patients with T-ALL.7 The frequencies of detected mutations and copy number alterations strongly resembled those previously found in a reference cohort of patients with T-ALL, both at the level of individual genes and of pathways7 (Figure 1B; supplemental Table 2). However, we did notice that the percentage of patients with loss of CDKN2A/B was lower in T-LBL (61%) compared with T-ALL (78%; P = .0143). Furthermore, mutations in NOTCH1 were also found significantly less frequently in T-LBL (50%) compared to T-ALL (74%; P = .00117; supplemental Table 2). We recently showed that, in addition to NOTCH1 mutations, NOTCH1 gene fusions are recurrent in T-LBL but absent in T-ALL.8,9,10,NOTCH1 fusions appear mutually exclusive with NOTCH1 mutations and associated with high occurrence of relapse and death.8 Because the presence of NOTCH1 gene fusions could only be determined in a subset of this cohort, we cannot determine whether the sum of all NOTCH1 aberrations is similar between T-LBL and T-ALL. However, considering the differences between NOTCH1 fusions and NOTCH1 mutations in downstream effects and outcome,8 these alterations should probably not be combined in these analyses.
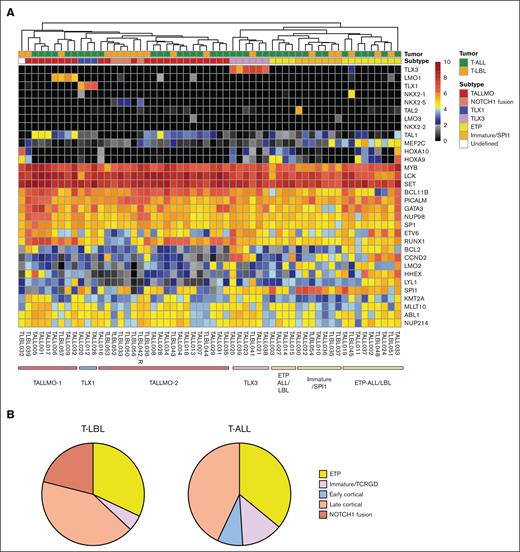
In T-ALL, next to the mutational landscape, transcriptomic characterization in T-ALL has provided valuable insights, including the identification of recurrent fusion genes as important drivers of the disease. The landscape of fusion genes in T-LBL is not yet extensively studied,7,11-14 but in our previous study, we identified gene fusions in 14 of 29 samples (48%), which, apart from NOTCH1 fusions, also included recurrent fusions involving the HOXA locus (supplemental Table 3). Most of these gene fusions have not, or only very rarely, been described in T-ALL. To further compare the 2 entities, we used the transcriptome data of 19 patients with T-LBL and 39 patients with T-ALL with sufficient quality for gene expression analysis (supplemental Methods). Based on the complete transcriptomes, an ample number of genes showed significant differential expression between T-LBL and T-ALL (upregulated, n = 4768; downregulated, n = 2380; supplemental Figure 2A). Upregulated genes in T-LBL were frequently associated with pathways related to extracellular matrix composition, adhesion, and cytokine-cytokine receptor interactions, likely caused by differences in the T-LBL and T-ALL microenvironments and heterogeneity in tumor biopsy source. Therefore, we studied a set of 32 genes that was previously shown to have the discriminatory power to distinguish between the different T-ALL subtypes (Early T-cell Precursor [ETP-ALL], TLX1/NKX2.1, TLX3, and TALLMO).15 These subtypes are associated with different stages of arrest of the T-cell and frequently determined by translocations and overexpression of transcription factors functioning as oncogenes. Analysis of the T-ALL cohort indeed revealed distinct clusters of the different subtypes as expected, with subclusters of ETP-ALL and TALLMO (supplemental Figure 2B). One of the ETP-ALL subclusters (ETP-ALL/SPI1) was found to be characterized by high expression of SPI1 and lower expression of MEF2C.16 We subsequently incorporated our T-LBL cohort into the analysis (Figure 2A). This combined analysis showed that the T-LBL samples clustered together with the various T-ALL subtypes associated with T-cell developmental stages, indicating a significant resemblance to T-ALL in terms of developmental arrest. All samples with a NOTCH1 gene fusion clustered together in TALLMO-2 and exhibited a similar, albeit aberrant, expression pattern compared with that of the rest of the samples, with increased expression of NKX2-5 (supplemental Table 3). Based on this clustering, we conclude that T-LBL and T-ALL samples share features associated with various thymocyte developmental stages. The contribution of cases arrested at the ETP stage was similar in T-LBL and T-ALL, accounting for 32% and 38% of the cases, respectively. Arrest of the immature/T-cell Receptor Gamma/Delta (TCRGD) (TLX3; T-LBL, 5%; T-ALL, 13%) and early cortical stages (T-LBL, 0%; T-ALL, 8%) was more frequent in T-ALL, although this might be because of the lower number of T-LBL cases. Lastly, arrest at the late cortical or mature stages of T-cell development was more frequent in T-LBL compared with T-ALL, accounting for 63% and 43% of the cases, respectively (Figure 2B). Therefore, comparable genetic lesions and subtypes suggest that the events required for oncogenic transformation of the T cell appear similar in T-LBL and T-ALL. Migration and homing mechanisms cannot be discovered by the currently used techniques and will require further in-depth studies. Nevertheless, our data further indicate that T-LBL and T-ALL represent different manifestations of the same disease, characterized by similar mutations and subtypes, but different gene fusions.
Subtypes associated to developmental stages in T-LBL and T-ALL. (A) Unsupervised clustering of T-LBL and T-ALL based on genes associated with the T-cell developmental genes, showing clustering in the major T-ALL subtypes for most of the T-LBL samples. Range of 0 to 10 showing the log2 transcript per millions of normalized expression values. (B) Distribution of subtypes associated with T-cell developmental stages in T-LBL and T-ALL shows great similarities, suggesting similar stages of arrest in T-LBL and T-ALL.
Subtypes associated to developmental stages in T-LBL and T-ALL. (A) Unsupervised clustering of T-LBL and T-ALL based on genes associated with the T-cell developmental genes, showing clustering in the major T-ALL subtypes for most of the T-LBL samples. Range of 0 to 10 showing the log2 transcript per millions of normalized expression values. (B) Distribution of subtypes associated with T-cell developmental stages in T-LBL and T-ALL shows great similarities, suggesting similar stages of arrest in T-LBL and T-ALL.
Acknowledgment: This research was funded by Kinderen Kankervrij (grant number 393).
Contribution: E.K. performed the study and wrote the manuscript; M.M.K., R.H., and F.v.D. performed the bioinformatic analyses; R.S.B. performed the wet laboratory work; L.A.K. coordinated the sequencing and data interpretation; M.A.S.-V. performed the histological analyses; J.L.C.L., J.P.P.M., and R.P.K. supervised the study; and all authors have read and agreed to the published version of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
The current affiliation for J.P.P.M. is Acerta Pharma (AstraZeneca), Oss, The Netherlands.
Correspondence: Roland P. Kuiper, Princess Máxima Center for Pediatric Oncology, Heidelberglaan 25, 3584 CS Utrecht, The Netherlands; email: r.kuiper@prinsesmaximacentrum.nl.
References
Author notes
J.L.C.L. and R.P.K. are joint last authors.
The transcriptome and whole-exome sequencing data in this article have been deposited in the European Genome-Phenome Archive, hosted by the European Bioinformatics Institute and the Centre for Genomic Regulation (accession numbers EGAS00001007703 and EGAS00001007767, respectively).
The full-text version of this article contains a data supplement.


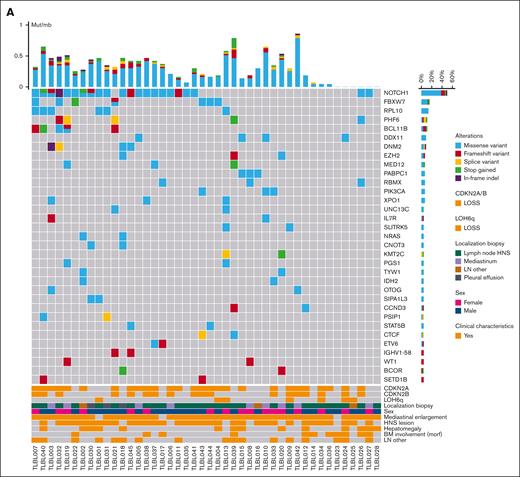
![Overview of recurrently mutated genes and pathways in T-LBL. (A) Oncoplot showing an overview of recurrently mutated genes in T-LBL per patient and per mutation, combined with the total mutation burden (mutations per megabase [mut/Mb]) and clinical characteristics. (B) Comparison of mutations sorted per pathway in T-LBL compared with T-ALL based on cohort from St. Jude Children’s Research Hospital (Liu et al7). Most frequently involved pathways are shown.](https://ash.silverchair-cdn.com/ash/content_public/journal/bloodneoplasia/1/3/10.1016_j.bneo.2024.100029/3/m_bneo_neo-2024-000230-gr1b.jpeg?Expires=1763926195&Signature=YAk70yhljn8Jlvr75Fu5kKlVVZzetzn9GtM7nSAlfvqwgxD~R-gwx3tgz6TnJYWV4tqeoHNlTaK2lNJeu4xJGTnR34qJ8zUnSGAZnLdA2LAt6DynsUqJzkjZLArQT5yZ~IGp8CQzyOOMhVQexy2uwnRekfLqKAToUaBM3divH4WagBd4F9~qoVUwiTEwtxlbQKo-6cPPz2tadm8V0EQE1Yi8b-kgnEGSpihdQ43XHw5DPe2mOIAqdpcriZ-~a0HhFWg85T86riV11n~ZQN-5egRMyQ4U5OqoValtYybJF8S3wc~OgzuFAxIicbD-JWuUnLObc9ZmEc8hPU9~CyN3qw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
