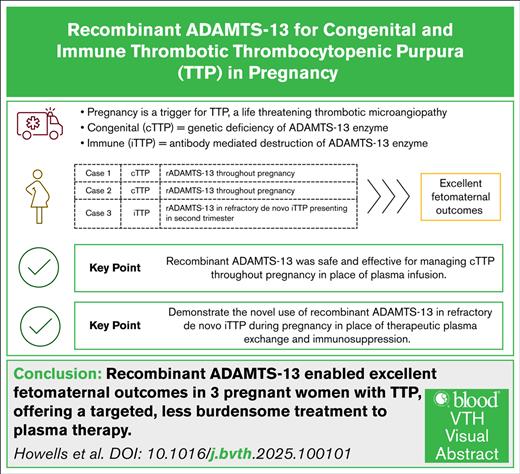
Key Points
rADAMTS-13 was safe and effective for managing cTTP throughout pregnancy in place of plasma infusion.
Novel use of rADAMTS-13 in refractory de novo iTTP during pregnancy in place of therapeutic plasma exchange and immunosuppression.
Visual Abstract
Thrombotic thrombocytopenic purpura (TTP) is a life-threatening emergency. Congenital TTP (cTTP) and immune-mediated TTP (iTTP) are caused by an inherited severe deficiency of, or immune-mediated destruction of the ADAMTS-13 enzyme, respectively. Pregnancy is recognized as a trigger for both subtypes of this condition. Until recently, the treatment for TTP in pregnancy has involved therapeutic plasma exchange and immunosuppression or plasma infusion. Here, we report 3 cases of TTP in pregnancy: 2 women with cTTP, treated throughout pregnancy with recombinant ADAMTS-13 (rADAMTS-13), and 1 with refractory iTTP, where rADAMTS-13 was used in place of ongoing plasma exchange. All pregnancies resulted in excellent fetomaternal outcomes.
Introduction
Thrombotic thrombocytopenic purpura (TTP) is a thrombotic microangiopathy caused by an inherited deficiency or immune-mediated destruction of ADAMTS-13 (a disintegrin and metalloproteinase with thrombospondin type 1 motif, member 13). Congenital TTP (cTTP) and immune-mediated TTP (iTTP) can complicate pregnancy or the postpartum period.1,2 ADAMTS-13 is a protease responsible for cleavage of ultralarge von Willebrand factor multimers, preventing platelet aggregation and microthrombus formation.3
Management of iTTP in pregnancy involves therapeutic plasma exchange (TPE) and immunosuppression. cTTP requires regular plasma infusion (PI) throughout pregnancy and beyond. Recently, recombinant ADAMTS-13 (rADAMTS-13) has emerged as an effective alternative to plasma. We present 2 patients with cTTP treated with rADAMTS-13 throughout pregnancy and 1 patient with refractory iTTP for whom rADAMTS-13 replaced further TPE and immunosuppression.
Methods
The diagnosis of TTP is based on microangiopathic hemolytic anemia, thrombocytopenia and organ ischemia, particularly affecting the heart, brain, kidneys, and placenta in pregnancy. Schistocytes and thrombocytopenia are present on peripheral blood smear. ADAMTS-13 activity levels <10% (normal range, 60-146 IU/dL) were confirmed in all cases.4 Raised anti-ADAMTS-13 antibodies indicate iTTP (normal range, 0%-6.1%),5 while cTTP is confirmed by identifying homozygous or compound heterozygous variants of the ADAMTS-13 gene.
ADAMTS-13 gene variants were identified in cases 1 and 2 (cTTP), and anti-ADAMTS-13 immunoglobulin G (IgG) antibody was detected in case 3 (iTTP). rADAMTS-13 is available in the United Kingdom on a Named Patient Programme, via Takeda Pharmaceuticals International AG, and was administered by expanded access in case 3. Consent was given by all patients (Medical Research Ethics Committee Numbers 08/H0810/54 and 08/H0716/72).
Results
Case 1
A 35-year-old patient was diagnosed with acute TTP immediately following her third pregnancy. Her obstetric history was significant for an intrauterine death of “unknown cause” at 28 weeks' gestation in her first pregnancy. Although she delivered a live infant 3 years later, placental histology showed chorionic villous hypoplasia, infarction, and decidual thrombosis, consistent with vascular malperfusion. In hindsight, maternal laboratory parameters at delivery were in keeping with acute TTP.
Her third pregnancy resulted in an emergency cesarean delivery at 37 weeks' gestation for reduced fetal movements. Two days prior, she had received prednisolone and IV immunoglobulin for suspected immune thrombocytopenia (ITP). Thrombocytopenia worsened postpartum, with hemolysis and schistocytes on a blood film. ADAMTS-13 gene mutational analysis confirmed homozygous R1060W variants c.3178C>T, p(Arg1060Trp) at exon 24.
ADAMTS-13 replacement for cTTP was initiated via weekly PI. Two months before her latest pregnancy, she had converted to weekly rADAMTS-13 infusions due to fatigue and headaches. Weekly rADAMTS-13 infusions of 40 IU/kg continued throughout pregnancy. The dose increased at 25 weeks' gestation to account for weight gain. Estimated fetal weight tracked between the 20th and 30th percentiles with normal uterine artery Doppler measurements.
The patient remained clinically well and underwent an elective cesarean delivery at 37 weeks' gestation, delivering a male baby weighing 2430 g. Placental histology was normal. The patient remained well postpartum, and continues weekly rADAMTS-13 infusions.
Case 2
A 36-year-old patient presented with acute TTP 5 years previously, following the preterm delivery of her first child at 29 weeks' gestation, weighing 964 g. Genetic analysis subsequently confirmed heterozygosity for both: c.1703G>T, p(Arg568IIe) missense variant in exon 14 and c.3178C>T, p(Arg1060Trp) missense variant in exon 24 of the ADAMTS-13 gene. Regular PI was initiated alternate weekly.
She became pregnant again 4 months later. The pregnancy was uneventful. From 20 weeks' gestation, PI was increased to weekly, and fetal growth tracked the 50th percentile. She underwent induction of labor at 37 weeks and delivered a healthy male baby weighing 2891 g.
PI continued alternate weekly for 3 years, but the patient reported debilitating fatigue, anxiety, and depression. She was taught to self-administer 40 IU/kg rADAMTS-13 infusions alternate weekly, with a rapid improvement in well-being.
In her third pregnancy, alternate-weekly rADAMTS-13 infusions continued without interruption, but were increased to weekly dosing from 29 weeks' gestation. She underwent induction of labor, and delivered a healthy male baby weighing 2650 g at 37 weeks' gestation. She remains well and continues alternate-weekly rADAMTS-13 infusions.
Case 3
A 28-year-old woman presented at 25 weeks' gestation in her first pregnancy, with 3 days of bruising, headaches, and visual blurring alongside thrombocytopenia (platelets, 21 × 109/L) and mild anemia (hemoglobin, 104 g/L). Initial lactate dehydrogenase levels were normal, and schistocytes were absent. Pregnancy was so far uncomplicated. She received prednisolone and IV immunoglobulin for presumed ITP. ADAMTS-13 activity subsequently confirmed TTP (<10%), and anti-ADAMTS-13 IgG antibody was elevated (69%).
Acute iTTP treatment was initiated. Magnetic resonance imaging of the head showed multiple areas of restricted diffusion in keeping with ischemic foci. Serum troponin was elevated (64 ng/L; normal range, 0-14 ng/L). Following 5 days of TPE and corticosteroids, the platelet count normalized. Daily corticosteroids caused hyperglycemia requiring metformin and insulin therapy. ADAMTS-13 activity remained <5 IU/dL, and rituximab (375 mg/m2) was added.
On day 13, she reported recurrence of visual blurring, and the platelet count fell to 145 × 109/L. ADAMTS-13 activity levels remained <5 IU/dL. TPE was restarted, and additional treatment options were discussed. Caplacizumab was not initiated given the early gestation. She commenced rADAMTS-13 (40 IU/kg), with a rapid rise in ADAMTS-13 activity (49.5 IU/dL before rADAMTS-13 infusion immediately after TPE, to 114.5 IU/dL after rADAMTS-13). A second dose was administered 12 hours later (ADAMTS-13 activity before infusion was 83.9 IU/dL vs 148.7 IU/dL after infusion), and a second dose of rituximab was administered. Further dosing was based on ADAMTS-13 activity, aiming to maintain levels >50% (Figure 1).
The patient was discharged at 29 weeks' gestation. Fetal growth progressed between the 10th and 20th percentiles. Three further doses of rADAMTS-13 were administered. Thereafter, ADAMTS-13 activity levels remained normal (>60 IU/dL), and ADAMTS-13 antibody level was <1%. Immunosuppression and antihyperglycemic therapy were stopped.
At 37 weeks' gestation, she delivered a healthy female baby weighing 2755 g via elective cesarean delivery as per maternal choice. Placental histology was unremarkable, without perivillous or intervillous fibrin deposition. No further treatment for TTP was required, and her ADAMTS-13 level remains normal 1 year later.
Discussion
Here we report 2 previously undescribed scenarios, to our knowledge, of treatment for TTP in pregnancy with rADAMTS-13: 2 cTTP cases exclusively managed with rADAMTS-13 throughout pregnancy and the first case of rADAMTS-13 usage in a case of acute iTTP, where the patient demonstrated refractory TTP early in her pregnancy course.
Pregnancy-related TTP is rare, and severe ADAMTS-13 deficiency affects an estimated 1 in 200 000 pregnancies.6,7 Diagnostic uncertainty is common and may delay diagnosis. Two cases here were initially labeled as ITP, and in 1 case the patient had significant prior obstetric morbidity where cTTP was most likely implicated. Prompt recognition of TTP, as well as distinction between cTTP and iTTP, is essential for optimizing pregnancy outcomes.1
Figures from the United Kingdom TTP Registry report that two-thirds of de novo TTP cases presenting during pregnancy were attributable to cTTP rather than iTTP.2 Fetal loss was highest during the second trimester but was reduced when cTTP was diagnosed and actively managed. In other cohorts, cTTP accounts for approximately one-third of obstetric TTP cases, reporting an overall fetal survival rate of 75%.8,9
In patients who were not pregnant, the standard of care for acute iTTP involves TPE, caplacizumab, and immunosuppression.10 Caplacizumab is a bivalent nanobody inhibiting platelet binding to von Willebrand factor, and has become a mainstay in acute TTP treatment.11 Publications reporting its safe use in pregnancy are limited.12-14 Its mechanism of action poses a hemorrhagic risk, and small molecular size carries the potential for placental transfer and fetal harm. This iTTP case presented early in pregnancy, requiring remission of anti-ADAMTS-13 immune response, reduction in anti-ADAMTS-13 IgG antibody levels, and normalization of ADAMTS-13 activity level, which cannot be achieved by the use of caplacizumab. Prolongation of severe ADAMTS-13 deficiency would impact placental function and fetal outcome.
rADAMTS-13 is a pivotal treatment in cTTP. It has a favorable and nonimmunogenic safety profile, with superior pharmacokinetics to PI.15,16 In the phase 3 trial comparing prophylaxis with rADAMTS-13 vs standard of care with PI in cTTP, adverse events were lower in the rADAMTS-13 group, and peak ADAMTS-13 activity levels were fivefold higher.17 Use of rADAMTS-13 in the treatment of acute iTTP in place of established standard of care with TPE is novel. The results of a phase 2 multicenter clinical trial appear promising, and cases of its use in the nonobstetric setting have been reported.18,19
To date, there are 2 published cases of rADAMTS-13 use in pregnant patients with cTTP. In both cases, patients became refractory or intolerant of plasma-based therapy, and rADAMTS-13 represented rescue therapy.20,21 Our 2 patients with cTTP were safely managed with regular rADAMTS-13 prior to, and throughout pregnancy, averting plasma infusion altogether. Neither experienced a clinical exacerbation, and both delivered babies of healthy birth weight with no TTP-associated complications. Trough ADAMTS-13 activity levels were maintained between 10% and 15% throughout pregnancy, which is not achievable with plasma alone.
Case 3 reports on the novel use of rADAMTS-13 in place of TPE in a patient with refractory de novo iTTP in the second trimester of pregnancy. rADAMTS-13 infusion resulted in significantly higher ADAMTS-13 activity levels than had been achieved with TPE and immunosuppression. ADAMTS-13 activity levels were used to guide interval timing of rADAMTS-13 infusions, and rapidly resulted in TTP remission, cessation of immunosuppression, and swift discharge from the hospital. Complete serological and clinical remission were sustained throughout pregnancy, and at 1 year.
In conclusion, significant advances in the diagnosis and management of cTTP and iTTP have improved obstetric outcomes. While the use of rADAMTS-13 has already been described in cTTP in pregnancy, we report its safe and effective use throughout the entirety of pregnancy, bypassing the need for plasma therapy. We also describe the first case of rADAMTS-13 being used in place of TPE and immunosuppression in the setting of acute refractory de novo iTTP in pregnancy, with an excellent fetomaternal outcome. This series will add to the available literature supporting the use of rADAMTS-13 in pregnancy in both cTTP and iTTP.
Acknowledgments
The authors thank Takeda Pharmaceuticals, Cambridge and Boston, MA, for compassionate use of recombinant ADAMTS-13 for case 3.
Authorship
Contribution: All authors contributed to the writing of the manuscript and its final review.
Conflict-of-interest disclosure: M.R.T. reports advisory board fees from Ablynx, Sanofi, and Bayer; speaker fees from Bayer, Sanofi, and Anthos; consultancy for Bayer and Anthos; and research support from Anthos, Thrombosis UK, and NHS Blood and Transplant. M.S. reports advisory board and speaker fees from Takeda, Sanofi, and Alexion; and a research grant from Takeda. The remaining authors declare no competing financial interests.
Correspondence: Lara Howells, Department of Haematology, University College London Hospitals, 5th Floor Central, 250 Euston Rd, London NW12PG, United Kingdom; email: lara.howells1@nhs.net.
References
Author notes
Publication-related data are available on request from the corresponding author, Lara Howells (lara.howells1@nhs.net).