Visual Abstract
TO THE EDITOR:
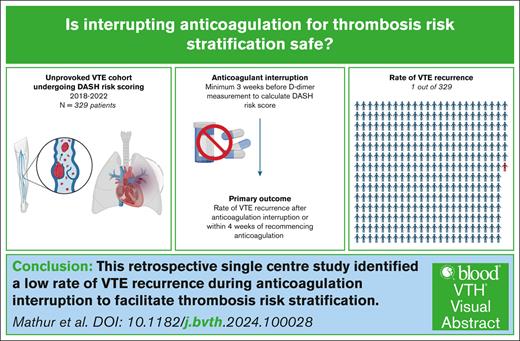
Accurately predicting the risk of venous thromboembolism (VTE) recurrence is important in deciding which patients should continue anticoagulation indefinitely.1 VTE recurrence risk after an unprovoked event is significantly higher than that provoked by a major transient risk factor.2-4 However, identifying patients who require long-term anticoagulation after a first unprovoked VTE remains challenging. Various risk scores have been developed to quantify the risk of VTE recurrence after unprovoked VTE.5-7 Current expert consensus is that if the predicted annual recurrence rate of VTE is <5%, then it is acceptable to stop anticoagulation after a finite period for patients with an unprovoked VTE.2 To perform the DASH (D-dimer, age, sex, hormone use) and Vienna risk prediction model scores in line with the initial descriptions, patients are required to interrupt anticoagulation for a minimum of 3 weeks.5,6 The rate of VTE recurrence during this period of inherent risk off anticoagulation is not known but may be significant. Understandably, this can lead to anxiety among both clinicians and patients with regard to the possibility of a new episode of VTE occurring while off anticoagulants. Patients occasionally ask for that risk to be quantified. Our review suggests that there is little in the published literature documenting the rates of VTE occurring while anticoagulation is withheld to facilitate DASH scoring.
Here, we report our retrospective analysis quantifying the recurrence rate of VTE during the anticoagulation interruption window in patients with unprovoked VTE. Our institutional policy was to use the DASH score to assess VTE recurrence risk in these patients.6 Our practice also includes screening for high-risk thrombophilias (antithrombin deficiency and antiphospholipid syndrome). After the publication of the DASH validation cohort study,7 our local policy changed and DASH scoring was no longer used in patients aged ≥65 years.
Consecutive patients with VTE reviewed at our hemostasis and thrombosis clinic between 4 January 2018 and 31 August 2022 were screened using D-dimer requests. Patients were included in the analysis if they had objectively proven unprovoked VTE and underwent DASH risk stratification, necessitating a 3-week period of anticoagulation interruption. Although there may be differences in circulating anticoagulant effect with different anticoagulants (eg, direct-acting oral anticoagulant vs warfarin), it was important to use the model as it was validated that D-dimer was measured 3 or more weeks off anticoagulation regardless of what treatment was initially used. Patients with provoked VTE (eg, cancer-associated VTE) were excluded. The primary outcome was the rate of VTE recurrence after anticoagulation interruption or within 4 weeks of recommencing anticoagulation. Patients were instructed to immediately resume anticoagulation after completion of their risk stratification blood tests. They were subsequently reviewed in the clinic for a follow-up appointment when a recommendation for anticoagulation duration was made. A diagnosis of recurrence requires objective radiological evidence. In cases where it was not possible to distinguish radiologically between new and old thrombi, the emergence of new symptoms and the assessing physician’s clinical judgment were used to define a recurrent event. Distal deep vein thrombosis (DVT) and superficial thrombophlebitis were not counted as a recurrence event.
In total, 329 consecutive and eligible patients were identified. The patient characteristics are shown in Table 1. The median age at initial VTE diagnosis was 57 years (range, 16-85 years), and 67.8% of the patients were male. The index events were DVT in 46.8%, pulmonary embolism (PE) in 50.8%, and both DVT and PE in 2.4%. Direct-acting oral anticoagulants (79.6%) were the most commonly used anticoagulants for the treatment of VTE compared with vitamin K antagonists (20.4%). Rivaroxaban was the preferred anticoagulant for 70.2% of the patients.
Patient characteristics in the study
| No. of patients . | N = 329 . |
|---|---|
| Sex | |
| Male | 223 (67.8) |
| Female | 106 (32.2) |
| Median age at VTE, y (range) | 57 (16-85) |
| Index VTE | |
| PE | 167 (50.8) |
| DVT | 154 (46.8) |
| PE + DVT | 8 (2.4) |
| Anticoagulant choice for initial treatment period | |
| Apixaban | 26 (7.9) |
| Rivaroxaban | 231 (70.2) |
| Edoxaban | 3 (0.9) |
| Dabigatran | 2 (0.6) |
| Warfarin | 66 (20.1) |
| Phenindione | 1 (0.3) |
| DASH score | |
| −2 | 3 (0.9) |
| −1 | 7 (2.1) |
| 0 | 22 (6.7) |
| 1 | 142 (43.2) |
| 2 | 57 (17.4) |
| 3 | 88 (26.7) |
| 4 | 10 (3.0) |
| Positive D-dimer | 131 (39.8) |
| No. of patients . | N = 329 . |
|---|---|
| Sex | |
| Male | 223 (67.8) |
| Female | 106 (32.2) |
| Median age at VTE, y (range) | 57 (16-85) |
| Index VTE | |
| PE | 167 (50.8) |
| DVT | 154 (46.8) |
| PE + DVT | 8 (2.4) |
| Anticoagulant choice for initial treatment period | |
| Apixaban | 26 (7.9) |
| Rivaroxaban | 231 (70.2) |
| Edoxaban | 3 (0.9) |
| Dabigatran | 2 (0.6) |
| Warfarin | 66 (20.1) |
| Phenindione | 1 (0.3) |
| DASH score | |
| −2 | 3 (0.9) |
| −1 | 7 (2.1) |
| 0 | 22 (6.7) |
| 1 | 142 (43.2) |
| 2 | 57 (17.4) |
| 3 | 88 (26.7) |
| 4 | 10 (3.0) |
| Positive D-dimer | 131 (39.8) |
All values are reported as n (%) unless otherwise indicated.
PE, pulmonary embolism.
During the period of anticoagulation interruption for DASH scoring, only 1 patient (0.3%) in our cohort experienced a new VTE event. This patient experienced new leg swelling on the same side as their index DVT. It was not possible to radiologically comment on chronicity or extension but the patient was treated as a likely new event based on the clinical and radiological evidence available. Three other patients had repeat imaging during their period off anticoagulation. These demonstrated residual thrombus but were not labeled as new events. Two patients had index PEs and presented with breathlessness; repeat imaging was consistent with chronic or resolving thrombosis. The other patient with index DVT had leg swelling on the same side as the initial presentation; repeat imaging was consistent with chronic thrombosis, and a diagnosis of postthrombotic syndrome was made.
The absolute risk of new VTE events off anticoagulation in our cohort was 1 in 329 (or 3/1000). This is lower than the rate of 1 in 67 new events previously reported.8 This risk quantification may be a useful aid in deciding whether to proceed with interrupting anticoagulation in high-risk patients. In our opinion, it is safe to discontinue anticoagulation for the purpose of VTE risk stratification, because the small risk of recurrent event is balanced against making a potentially life-changing decision regarding lifelong anticoagulation.
Although our study was limited by its retrospective data collection, the outcomes could be reliably identified from the detailed electronic records of the patients. Further analysis has been included in the supplemental Data.
The study was approved by our local National Health Service Caldicot Guardian. We also obtained a review by our institutional Integrated Research Application System (IRAS) board, and no ethical approval was needed for the work submitted in this article.
Contribution: A.M. and M.M.K. contributed to the study’s conception and design; A.M. and A.C. performed data collection and analysis; A.M. performed statistical analyses and wrote the first draft of the manuscript; and all authors reviewed and contributed to the writing of the manuscript and approved the final manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Abhinav Mathur, Department of Haematology, Aberdeen Royal Infirmary, Foresterhill Health Campus, Aberdeen, United Kingdom; email: abhinav.mathur@nhs.scot.
References
Author notes
The data that support the findings of this study are available on request from the corresponding author, Abhinav Mathur (abhinav.mathur@nhs.scot). The data are not publicly available because of privacy or ethical restrictions.
The full-text version of this article contains a data supplement.