Abstract
Passive immune therapy consists of several different therapies, convalescent plasma, hyperimmune globulin, and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) neutralizing monoclonal antibodies. Although these treatments were not part of any pandemic planning prior to coronavirus disease 2019 (COVID-19), due to the absence of high-quality evidence demonstrating benefit in other severe respiratory infections, a large amount of research has now been performed to demonstrate their benefit or lack of benefit in different patient groups. This review summarizes the evidence up to July 2021 on their use and also when they should not be used or when additional data are required. Vaccination against SARS-CoV-2 is the most important method of preventing severe and fatal COVID-19 in people who have an intact immune system. Passive immune therapy should only be considered for patients at high risk of severe or fatal COVID-19. The only therapy that has received full regulatory approval is the casirivimab/imdevimab monoclonal cocktail; all other treatments are being used under emergency use authorizations. In Japan, it has been licensed to treat patients with mild to moderate COVID-19, and in the United Kingdom, it has also been licensed to prevent infection.
Learning Objectives
Summarize current evidence on the use of passive immune therapy to prevent infection—whether it reduces risk of death or hospitalization
Summarize current evidence on the use of passive immune therapy for high-risk patients who have mild COVID-19 symptoms—risk of death
Can state whether passive immune therapy reduces all-cause mortality for hospitalized patients and whether any subgroups will benefit
CLINICAL CASE 1
A 74-year-old man (case) had a test for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) after a family gathering for the christening of his granddaughter. He had had the test because he was a close contact for the index case at the christening. His 49-year-old nephew (index case) had been admitted to hospital the day after the christening and was found to be SARS-CoV-2 positive. The nephew had had some symptoms at the time of the christening but had not thought that these were due to coronavirus disease 2019 (COVID-19). The 74-year-old man self-isolated with his wife while awaiting the results of the test.
Introduction
Passive antibody therapy is one of the oldest treatments for infectious diseases that is still in use. Emil von Behring (1854-1917) was awarded the first Nobel Prize in Medicine “for his work on serum therapy, especially its application against diphtheria.”1 Today, passive antibody therapy involves treatment with polyclonal antibodies derived from humans (convalescent plasma [CP] or hyperimmune globulin), animals (antisera), or antigen-specific monoclonal antibodies (mAbs).2 In this review, I focus on CP and neutralizing mAbs and the current evidence for their use. There are no published trials on the use of hyperimmune globulin in COVID-19.3
CP after infection, particularly after severe illness, may contain high levels of polyclonal pathogen-specific antibodies. These antibodies may confer passive immunity to recipients and in viral diseases are thought to have their main action via neutralization of viral particles.4 Collection and transfusion of CP can occur rapidly after the onset of a pandemic, with collection of plasma occurring from 14 days after a patient has recovered from the infection. The antibody response in CP donors adapts with the virus, either due to donors becoming infected with new variants of the virus or due to vaccination after an initial natural infection. However, the levels of neutralizing antibody can vary significantly from 1 unit to the next, and a minimum threshold of antibody is required within each unit to ensure that the transfusion contains a sufficient level of neutralizing antibody (Table 1).
Hyperimmune globulin is currently used to protect vulnerable individuals from other viral infections, including varicella zoster.5 It is produced by pooling thousands of donations from people who have recovered from an infection or have been vaccinated against an infection and have high levels of antibodies. It produces a consistent product that always has a defined level of antibody within it. However, it takes time to produce, so it cannot be used as early in a pandemic. It will also evolve with changes with the viral variant but not as rapidly as CP.
Neutralizing monoclonal antibody therapy can be derived from humans who have had an infection, or been vaccinated, or from humanized mice that have been exposed to SARS-CoV-2 antigens.2 Monoclonal antibody production can identify antibodies with a high level of neutralizing activity and can be produced without the need for blood donors. mAbs will, however, not adapt to viral variants, and so over time, the virus can become resistant to the monoclonal antibody. This has already happened with the SARS-CoV-2 virus (Table 2). Monotherapy with bamlanivimab has had its emergency use authorization (EUA) withdrawn due to development of viral resistance.6 This may mean that monoclonal cocktails are effective and less likely to lead to resistance than use of a single monoclonal. However, even a monoclonal cocktail could become ineffective in the future, as shown by the prospective mapping of viral variants that detected a potential mutation (E406W) that could escape neutralization by both components of the casirivimab/imdevimab monoclonal cocktail, as well as both components of the bamlanivimab/etesevimab cocktail (Table 2).7 Monoclonal therapy is expensive and requires very specialized manufacturing units. It is therefore a treatment that most low- and middle-income countries cannot afford and will find more difficult to manufacture locally. CP can be produced in many countries and is much more affordable.8 Therefore, when thinking about whether to use passive immunization therapy, consideration needs to be made not just on its effectiveness but also on its accessibility.
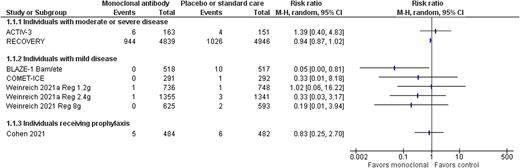
Prophylactic therapy
The mainstay of preventing infection in people with an intact immune system is vaccination. Active immunization against SARS-CoV-2 has been shown to be effective at preventing severe and fatal COVID-19, as well as reducing the risk of symptomatic COVID-19.9 In the United States, by the end of June 2021, vaccination had averted an estimated 279 000 deaths and up to 1.25 million hospitalizations.10 However, vaccination is not as effective in patients with an impaired immune system, either due to immunosuppressive therapy or an underlying disease that affects the immune system. Patients with hematologic malignancies mount blunted antibody responses to SARS-CoV-2 vaccination, and those most at risk appear to be patients who are actively treated with Bruton tyrosine kinase inhibitors, ruxolitinib, venetoclax, or anti-CD20 antibody therapies.11 Consideration therefore needs to be given to preventing infection in people who are unvaccinated or partially vaccinated and are at high risk of developing severe and fatal COVID-19 due to comorbidities or those who have been fully vaccinated but are unable to mount an effective immune response to vaccination. There have been 2 completed trials assessing monoclonal therapy12,13 (Table 3), with 1 trial assessing the effect of 1.2 g of the casirivimab/imdevimab cocktail (subcutaneously via 4 injections) given to household contacts of a positive case.13 However, most of these individuals were not at high risk of severe disease, with fewer than 10% older than 65 years and only 1% with immune suppression. The other trial used bamlanivimab, which showed a benefit in nursing home residents who received the intervention in progression to moderate or severe disease but no evidence of a difference in mortality (Figure 1). However, bamlanivimab is not effective against many of the viral variants currently in circulation. Ongoing studies of CP, hyperimmune globulin, and mAbs assessing high-risk prophylaxis will be assessed within living systematic reviews, so additional information may be available over the next few months.23,24 It is especially important to know their additional impact over and above vaccination for those individuals who have a poor response to vaccination, for example, the immunosuppressed population.11
SARS-CoV-2 mAb vs placebo or standard care—all-cause mortality at 28 days or hospital discharge.
SARS-CoV-2 mAb vs placebo or standard care—all-cause mortality at 28 days or hospital discharge.
CLINICAL CASE (Continued)
The patient and his wife received the results of the polymerase chain reaction test the next day, and both had tested positive for SARS-CoV-2. In total, 15 of the 45 people who attended the christening tested positive for SARS-CoV-2 within the days following the christening. He started to develop symptoms of fever and a dry cough the day after his positive test, but his symptoms were mild, and he treated the fever with paracetamol and rested at home.
Treatment with asymptomatic infection or mild symptoms
Vaccination is known to decrease the risk of progression to moderate or severe COVID-19 disease, although it has less of an impact on the development of asymptomatic or mild symptoms. All of the current evidence for passive immune therapy is prior to vaccination, or patients who were vaccinated or about to be vaccinated were excluded from the trials. Data from Public Health England have shown that vaccination decreases the risk of hospitalization by over 90%, even with the delta variant. It is therefore more difficult to know the real additional effect of passive immune therapy over and above vaccination (Tables 3 and 4).
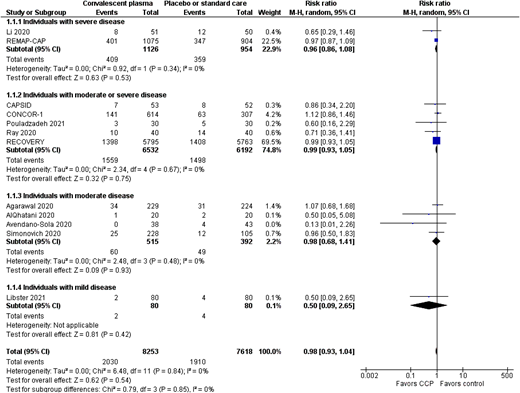
In the studies that assessed bamlanivimab alone or regdanvimab, there were no deaths in any of the study arms; therefore, any effect on all-cause mortality cannot be assessed.42 The only study that showed a reduction in mortality was the BLAZE-1 trial17 arm that used the bamlanivimab/etesevimab monoclonal cocktail (Figure 1); the casirivimab/imdevimab cocktail trial showed a trend in the direction of effect, but it was not clinically significant,15,20 nor was the effect of high-dose CP (Figure 2).3,8 Therefore, although it is suggestive that passive immune therapy if given early could save lives and the reduce risk of severe disease, additional data are required before it can be used in routine practice. None of the studies have performed a cost-effectiveness analysis, but it is likely that those patients who do not respond to vaccination and are at high risk of severe or fatal COVID-19 are the group that will demonstrate a benefit.
CP vs placebo or standard care—all-cause mortality at 28 days or hospital discharge.
CP vs placebo or standard care—all-cause mortality at 28 days or hospital discharge.
CLINICAL CASE (Continued)
Seven days after the christening, he developed increasing shortness of breath and called an ambulance. On examination by the paramedics, he was pyrexial (temperature 38.9°C), had a respiratory rate of 25 breaths per minute, and was hypoxic with an oxygen saturation of 91% on room air. He was given oxygen by the paramedics and taken to the local emergency room. In the emergency room, he was given steroids and admitted to the hospital for oxygen therapy.
Treatment with moderate or severe symptoms
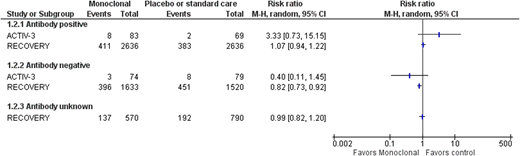
Two trials have assessed monoclonal antibody use in moderately or severely unwell patients; neither showed a benefit for patients overall (Figure 1), but there was a benefit for patients who had not yet developed a detectable antibody response (Figure 3). Those patients who did not develop an antibody response had a much higher mortality rate than those who did not.19,21 This is partly because patients who have a delayed antibody response are older and have more comorbidities. This does mean that reducing mortality in this group will mean a larger absolute reduction in mortality; for example, based on the RECOVERY data, 54 lives per 1000 patients treated would be saved (95% CI, 24-80 lives saved per 1000 patients treated). Some SARS-CoV-2 variants are resistant to bamlanivimab monotherapy, whereas the current major variants in circulation are still sensitive to neutralization by the casirivimab/imdevimab cocktail. However, this may change with the development of new variants.7 As variant screening cannot be done in real time, passive antibody treatments need to be used that are effective against all current variants in a particular region of the world. CP use does not show a benefit overall for patients with moderate or severe COVID-19.29,30,39 CP has also been assessed in antibody-negative patients in 2 major trials, RECOVERY and REMAP-CAP.29,39 This shows a similar trend in the direction of a possible effect in CP, but it does not reach statistical significance (risk ratio [RR], 0.93; 95% CI, 0.86-1.01). This may partly be because CP is a much more variable product, with some units having much lower antibody levels than others, so even if a minimum titer is used within the trials, this may not have been sufficient. Several trials have shown an effect in a subgroup of participants who received a higher titer product.8,32
SARS-CoV-2 mAb vs placebo or standard care—all-cause mortality at 28 days or hospital discharge by antibody status at baseline.
SARS-CoV-2 mAb vs placebo or standard care—all-cause mortality at 28 days or hospital discharge by antibody status at baseline.
CLINICAL CASE (Continued)
Over the next 2 days, the 74-year-old man continued to deteriorate and was admitted to intensive care for noninvasive ventilatory support. An emergency use access request for CP was made, and he received CP on day 10 after the christening.
Treatment of critically unwell participants
Fewer trials have specifically assessed interventions for the critically unwell patients (requiring respiratory or cardiovascular organ support) with an intensive care level of care (Tables 1 and 2). Several trials exclude patients requiring mechanical ventilation or organ support of any type. One of the trials that has focused on this patient group is the REMAP-CAP trial.39 It showed no benefit of CP overall (Figure 2), but a prespecified subgroup showed potential benefit of CP. This trial, based on Bayesian statistics, showed an 89.9% posterior probability of benefit in this subgroup. This was a broad group of immunosuppressed patients based on the Acute Physiology and Chronic Health Evaluation (APACHE) score definition of immunosuppression.39 However, as it was a small subgroup, additional research is required to confirm whether or not this is a true finding. The RECOVERY trial did include patients receiving noninvasive and invasive ventilation, and no evidence of a difference was seen for those patients receiving invasive (RR, 0.71; 95% CI, 0.35-1.47; 70 participants) or noninvasive ventilation (RR, 0.86; 95% CI, 0.68-1.08; 673 participants), but the CIs are wide.
CLINICAL CASE (Continued)
Unfortunately, the 74-year-old man continued to deteriorate and subsequently required invasive ventilation. Fourteen days after the christening, he died due to COVID-19. In total, 5 of the guests at the christening were admitted to hospital, including all 4 of the grandparents of the baby and the uncle (the index case), who had diabetes and hypertension. Both grandfathers died of COVID-19.
Key points (see Visual abstract)
Up to now (July 2021), most of the evidence is based on trials performed prior to the introduction of vaccination. Vaccination is likely to be the most cost-effective strategy for preventing infection in the general population, including healthy individuals with high-risk exposure (eg, health care workers). There are insufficient data on the outcomes of prophylactic passive antibody therapy in immunosuppressed individuals.
Passive immune therapy (monoclonal therapy and CP) may be beneficial for high-risk patients who have mild COVID-19 symptoms, but more data are required. Some countries, including the United States, are using passive monoclonal therapy for this indication under EUA.
High-dose passive immune therapy (casirivimab/imdevimab) reduces all-cause mortality for hospitalized patients who have not yet developed a detectable antibody response (SARS-CoV-2 IgG antibody). This monoclonal cocktail has just been approved by the Medicines and Healthcare products Regulatory Agency based on this evidence, but indications for its use are currently not available.
CP may be beneficial for immunosuppressed individuals who are severely or critically unwell, but more data are required.
The virus continues to change, and so although treatments may be effective against current SARS-CoV-2 viral variants of concern, this may not be true in the future. Passive immune therapies will either have to be very broad spectrum or adapt with the virus.
Conflict-of-interest disclosure
Lise J. Estcourt: author on Cochrane living systematic reviews of monoclonal therapies and CP. Investigator on the RECOVERY and REMAP-CAP trials.
Off-label drug use
Lise J. Estcourt: nothing to declare.