Abstract
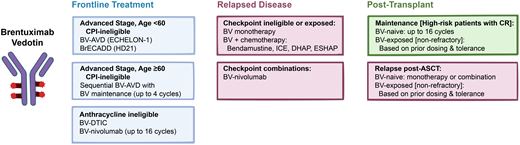
The CD30-directed antibody-drug conjugate brentuximab vedotin (BV) was FDA approved in 2011 for the treatment of relapsed classic Hodgkin lymphoma (cHL), in 2015 for maintenance after autologous transplantation in high-risk patients, and in 2018 for frontline therapy with doxorubicin, vinblastine, and dacarbazine for advanced stage cHL. Although the role of BV in cHL had been reasonably well-established, it is currently being challenged by the changing landscape of other highly effective novel agents, such as checkpoint inhibitor immunotherapies. In this review, we discuss the evolving role of BV in the management of cHL and ongoing studies attempting to define the optimal usage of this effective agent.
Learning Objectives
Describe updated results of currently approved indications for BV and how to optimize its use in the front-line treatment of cHL
Discuss the evolving role of BV in relapsed disease and challenges regarding treatment sequencing
CLINICAL CASE
A 34-year-old woman presents with night sweats. Biopsy of a supraclavicular node is consistent with nodular sclerosis classic Hodgkin lymphoma (cHL). Staging positron emission tomography with computed tomography (PET-CT) revealed supraclavicular, mediastinal, and retroperitoneal adenopathy, as well as splenic and liver lesions consistent with stage IVB disease. Her International Prognostic Score (IPS) is 4/7 (stage IV, hemoglobin <10.5 g/dL, albumin <4 g/dL, and white blood cell [WBC] ≥15 000). Past medical history is significant for systemic lupus erythematosus currently controlled by hydroxychloroquine.
Frontline therapy—advanced stage
Chemotherapy with a doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) backbone has been the mainstay of therapy for advanced cHL in the US. A widely adopted approach based on the RATHL trial utilizes an interim PET-CT (iPET) after 2 cycles of ABVD to omit bleomycin in subsequent cycles for patients with complete response (CR) defined as Deauville score (DS) 1-3.1 This approach achieved equivalent efficacy with reduced pulmonary toxicity.2
Another front-line approach utilizes brentuximab vedotin (BV) plus AVD based on the results of the phase 3 ECHELON-1 trial in patients with advanced stage cHL. At 6-year follow-up, BV-AVD had a 7.8% progression free survival (PFS) and a 4.5% overall survival (OS) benefit over ABVD. While BV-AVD had higher rates of febrile neutropenia, a protocol amendment mandating prophylactic growth factor led to reduced grade (G) ≥3 infections (18% to 11%) and febrile neutropenia (21% to 11%). Pulmonary toxicity was decreased compared to ABVD (2% versus 7% all events, <1% versus 3% G ≥ 3).3 In long-term follow-up, fertility was preserved, with similar birth rates compared to ABVD, and peripheral neuropathy resolved or improved in 85.6% of affected patients.3
In contrast to the A(B)VD approach, the German Hodgkin Study Group (GHSG) utilized escalated BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisolone) (escB) for advanced cHL. Despite high efficacy, this regimen was not widely adopted in North America due to toxicity, albeit lower with 4 versus 6 cycles.4 With the goal of further reducing acute and long-term toxicities while maintaining the efficacy of the regimen, the GHSG evaluated BV-based variants of escB.5,6 BrECADD (BV, etoposide, doxorubicin, cyclophosphamide, dacarbazine, dexamethasone) was recently compared with escB in the PET-adapted phase 3 HD21 trial.5,6 Sixty-four percent of patients were iPET-negative and received total 4 cycles of therapy. Results were excellent when BrECADD was compared to escB, with a superior 4-year PFS (94.3% versus 90.9%), lower acute hematologic toxicity (G4 31% versus 52%), and lower peripheral sensory neuropathy (all grades 38% versus 49%). There was no significant residual organ toxicity at 1 year after treatment, and >95% of female patients had hormonal recovery.7 These excellent results have established BrECADD as the new standard of care within the GHSG for adult patients age ≤60 years. Additionally, anthracycline exposure >200 mg/m2 has recently been described as a breast cancer risk factor for cHL patients independent of age or radiation exposure; with BrECADD x 4 cycles, cumulative anthracycline dosage is limited to 160 mg/m2, lower than the 300 mg/m2 with ABVD/BV-AVD.8
While ECHELON-1 was not response-adapted, the phase 2 EORTC-1537-COBRA study utilized early iPET after 1 cycle of BV-AVD to risk-stratify patients for BV-AVD x 5 (DS1-3, 60% of patients) or BrECADD (DS4-5, 40% of patients).9 All patients with fluorodeoxyglucose avidity at end of treatment received radiotherapy. The 2-year modified PFS was 88.3% for iPET-negative patients, versus 91.3% for iPET-positive patients. This trial supports the role of iPET-based therapy escalation even when BV-AVD has been used as initial therapy, with outcomes superior to those reported in ECHELON-1.10
Recently, S1826, a large US phase 3 intergroup study, directly compared concurrent nivolumab-AVD (N-AVD) to BV-AVD in newly diagnosed stage III/IV cHL.11 The trial enrolled both adult and pediatric patients and showed superior 1-year PFS for N-AVD (94% versus 86%) and no difference in OS.12 While the results at this early time point challenge the use of BV-AVD or BrECADD, it is important to note that patients with preexisting autoimmune disease requiring systemic therapy were excluded from the S1826 trial. In a systematic review of 123 patients with rheumatologic disease receiving checkpoint inhibitor immunotherapies (CPI) for cancer, 75% of patients had either an autoimmune flare or immune-related adverse event (IRAE), with 62% requiring high-dose corticosteroids, 16% requiring other immunosuppression, and 17% discontinuing CPI.13 Other exclusion criteria in S1826 included interstitial lung disease with risk of pneumonitis; patients requiring corticosteroids for other comorbidities (>10 mg daily prednisone equivalent); and patients with prior solid organ or stem cell transplantation at risk of allograft rejection.14,15 Chronic IRAEs including endocrinopathies are also underrecognized and persistent in up to ~40% of patients.16 Therefore, BV-AVD/BrECADD or ABVD-based therapy per RATHL remain viable options for select patients with advanced cHL and in regions where novel agents are unavailable or unaffordable.
CLINICAL CASE (continued)
Given our patient's history of systemic lupus erythematosus and the risk of immune flare with CPI, we opted to treat her with 6 cycles of BV-AVD. Interim and end of treatment PET demonstrated a CR.
Frontline therapy—early-stage
In contrast to advanced cHL, treatment options for early-stage disease include either chemotherapy alone or combined modality therapy (CMT) utilizing iPET-adapted strategies.17-19 The results of the RAPID, HD16, and H10F trials consistently suggest a modest PFS benefit for CMT over ABVD alone, albeit without an OS advantage. Recent studies have evaluated BV combinations in early-stage disease with the goal of increasing CR rates, reducing duration of therapy, or omitting radiation to minimize potential late effects (Table 1).
Selected trials utilizing brentuximab vedotin in frontline therapy
| Regimen . | N . | Median follow-up (months) . | ORR/CR . | PFS . | Reference . |
|---|---|---|---|---|---|
| Advanced Stage | |||||
| ECHELON-1 BV-AVDx6 ABVDx6 | 1334 | 73 | BV-AVD: 86% ORR ABVD: 83% ORR | 5-year: 82.2% BV-AVD 5-year: 75.3% ABVD | Ansell et al N Engl J Med 2022 |
| HD21 escBx4-6 BrECADDx4-6 | 1500 | 40 | escB: 80% CR BrECADD: 82% CR | 3-year: 92.3% escB 3-year: 94.9% BrECADD | Borchmann et al Lancet 2024 |
| Early-stage | |||||
| BREACH BV-AVDx4 + 30 Gy INRT ABVDx4 + 30 Gy INRT | 170 | 45 | BV-AVD: 87.6% CR (8% missing data) ABVD: 77.2% CR (19% missing data) | 2-year: 97.3% BV-AVD 2-year: 92.6% ABVD | Fornecker et al J Clin Oncol 2023 |
| BV-AVDx4 +/- RT | 117 | 46 | 96% CR | 2-year: 94% | Kumar et al J Clin Oncol 2021 |
| BV-AVD × 4-6 Interim PET adapted | 34 | 14 | 88% CR | 14-month: 90% | Abramson et al JCO 2015 (abstract) |
| BV-ADx4-6 Interim PET adapted | 34 | 53 | 97% CR | 5-year: 91% | Abramson et al Blood Advances 2023 |
| ABVDx2-6, BV × 6 Interim PET adapted | 41 | 47 | 95% CR | 3-year: 92% | Park et al Blood Advances 2020 |
| Elderly or anthracycline-ineligible | |||||
| Sequential BV-AVD | 48 | 23 | 95% ORR 93% CR | 2-year: 84% | Evens et al J Clin Oncol 2018 |
| BV-nivolumab | 21 | 51.6 | 86% ORR 67% CR | Not reached | Friedberg et al Blood 2024 |
| Regimen . | N . | Median follow-up (months) . | ORR/CR . | PFS . | Reference . |
|---|---|---|---|---|---|
| Advanced Stage | |||||
| ECHELON-1 BV-AVDx6 ABVDx6 | 1334 | 73 | BV-AVD: 86% ORR ABVD: 83% ORR | 5-year: 82.2% BV-AVD 5-year: 75.3% ABVD | Ansell et al N Engl J Med 2022 |
| HD21 escBx4-6 BrECADDx4-6 | 1500 | 40 | escB: 80% CR BrECADD: 82% CR | 3-year: 92.3% escB 3-year: 94.9% BrECADD | Borchmann et al Lancet 2024 |
| Early-stage | |||||
| BREACH BV-AVDx4 + 30 Gy INRT ABVDx4 + 30 Gy INRT | 170 | 45 | BV-AVD: 87.6% CR (8% missing data) ABVD: 77.2% CR (19% missing data) | 2-year: 97.3% BV-AVD 2-year: 92.6% ABVD | Fornecker et al J Clin Oncol 2023 |
| BV-AVDx4 +/- RT | 117 | 46 | 96% CR | 2-year: 94% | Kumar et al J Clin Oncol 2021 |
| BV-AVD × 4-6 Interim PET adapted | 34 | 14 | 88% CR | 14-month: 90% | Abramson et al JCO 2015 (abstract) |
| BV-ADx4-6 Interim PET adapted | 34 | 53 | 97% CR | 5-year: 91% | Abramson et al Blood Advances 2023 |
| ABVDx2-6, BV × 6 Interim PET adapted | 41 | 47 | 95% CR | 3-year: 92% | Park et al Blood Advances 2020 |
| Elderly or anthracycline-ineligible | |||||
| Sequential BV-AVD | 48 | 23 | 95% ORR 93% CR | 2-year: 84% | Evens et al J Clin Oncol 2018 |
| BV-nivolumab | 21 | 51.6 | 86% ORR 67% CR | Not reached | Friedberg et al Blood 2024 |
CMT utilizing a BV regimen was compared to ABVD in the phase 2 BREACH trial. Patients with unfavorable risk early-stage disease, as defined by European Organization for Research and Treatment of Cancer criteria, received either BV-AVD x 4 or ABVD x 4 cycles, with both arms followed by 30 Gy involved-node radiotherapy.20 The primary endpoint was iPET CR rate (DS1-3), which was significantly higher with BV-AVD (82.3% versus 75.4%).20 However, 2-year PFS was similar (97.3% versus 92.6%), and patients receiving BV-AVD had higher rates of febrile neutropenia and peripheral neuropathy.20
The omission of radiotherapy with BV was evaluated in a multicohort phase 2 US trial of patients with unfavorable risk factors by GHSG criteria (disease bulk defined as ≥10 m for cohort 1, >7 cm for cohorts 2-4).21 Patients with a negative PET (DS1-3) after BV-AVD x 4 cycles were treated with 1 of 4 radiotherapy strategies. At a median follow-up of 3.8 years, the 2-year PFS was 93% for patients receiving 30 Gy involved site radiotherapy (ISRT), 97% with 20 Gy ISRT, 90% with 30 Gy to residual PET-negative sites >1.5 cm, and 97% for patients receiving no radiotherapy.21 In a recent update, the 4-year PFS was inferior in patients with higher baseline metabolic tumor volume (91% versus 100%, P = 0.047).22
Studies have evaluated the omission of individual chemotherapy agents or reduction of number of cycles with BV-based regimens. A single-arm phase 2 US study evaluated the omission of vinblastine and bleomycin in patients with nonbulky early-stage disease. Patients were treated with BV-AD x 4-6 cycles (based on iPET response) without growth factor support.23 Ninety-four percent of patients achieved iPET CR (DS1-3) after 2 cycles and received BV-AD x 4, with a 97% end-of-treatment CR, an estimated 5-year PFS of 91%, and an OS of 96%.23 Another phase 2 US study evaluated ABVD x 2-6 cycles based on unfavorable risk status and iPET response, followed by consolidation with BV x 6.24 The CR rate was 95% with an estimated 3-year PFS of 92%, A subset of patients (11/40, 27.5%) completed treatment with only ABVD x 2 without radiotherapy, 65% received 4 cycles, and only 7.5% received 6 cycles.24
Cumulatively, these trials suggest that high CR rates and excellent PFS can be achieved with incorporation of BV and may allow for chemotherapy-only treatment of early-stage cHL. However, longer follow-up, larger randomized studies, and assessment of patterns of treatment failure are required to establish superiority.
CLINICAL CASE (continued)
At a clinic visit 12.5 months after end of therapy, a physical exam confirmed a new palpable supraclavicular lymph node. Biopsy was consistent with relapsed cHL, and PET demonstrated cervical recurrence.
Relapsed & Refractory Disease
The standard of care in relapsed cHL is salvage therapy followed by high-dose chemotherapy and autologous stem cell transplantation (ASCT), with improved outcomes seen in patients achieving PET negativity before transplant.25
Based on the high response rates observed with BV in relapsed cHL after ASCT, BV monotherapy has been evaluated as a bridge to transplantation. A multicenter phase 2 study reported an overall response rate (ORR) of 68% after BV x 4, and with this approach, 49% of patients (18/37) avoided additional chemotherapy, proceeding directly to ASCT after CR (35%) or partial response (14%).26,27
BV has also been combined with several chemotherapy regimens (Table 2). BV-bendamustine, with ASCT any time after the second cycle and single-agent BV maintenance for up to 16 total cycles, achieved a CR rate of 73.6% after a median of 2 cycles, with 75% of patients proceeding to ASCT.28 The regimen was well-tolerated with 54.4% peripheral neuropathy (3.6% G ≥ 3) and an estimated 92% 3-year OS.28 Platinum-based salvage combinations have also been evaluated and include BV, ifosfamide, carboplatin, and etoposide (BV-ICE); BV, dexamethasone, cisplatin, and cytarabine (BV-DHAP); and BV, etoposide, methylprednisolone, cytarabine (BRESHAP).29-31 Although these regimens achieve high CR rates of 70%-79%, most patients experience G3-4 hematologic toxicity with serious adverse event incidence from 29%-33%.29-31
Selected trials utilizing brentuximab vedotin in relapsed/refractory disease
| Regimen . | N . | Median follow-up (months) . | ORR/CR . | ASCT (%) . | PFS . | Reference . |
|---|---|---|---|---|---|---|
| BV combinations | ||||||
| BV-bendamustinex2-6 | 55 | 44.5 | 92.5% ORR 73.6% CR | 74% | 3-year: 60.3% | LaCasce et al Br J Haematol 2020 |
| BV-ICEx2 | 45 | 37 | 91% ORR 74% CR | 75% | 2-year: 80.4% | Lynch et al Lancet Haematol 2021 |
| Sequential BV-ICE | 46 | 20 | 76% CR | 98% | 2-year: 80% | Moskowitz et al Lancet Onc 2015 |
| BV-DHAPx3 | 55 | 27 | 90% ORR | 100% | 2-year: 74% | Kersten et al Haematologica 2021 |
| BRESHAPx3 | 66 | 27 | 91% ORR 70% CR | 70% | 30-month: 71% | Garcia-Sanz et al Ann Oncol 2019 |
| BV-nivolumab | 126 | 24 | 88% ORR 60.7% CR | 36% Included post-ASCT | Not reached | Diefenbach et al. ASH 2023 (abstract) |
| BV-nivolumab | 91 | 34.3 | 85% ORR | 92% | 3-year: 77% (all) 91% (per protocol) | Advani et al Blood 2021 |
| Regimen . | N . | Median follow-up (months) . | ORR/CR . | ASCT (%) . | PFS . | Reference . |
|---|---|---|---|---|---|---|
| BV combinations | ||||||
| BV-bendamustinex2-6 | 55 | 44.5 | 92.5% ORR 73.6% CR | 74% | 3-year: 60.3% | LaCasce et al Br J Haematol 2020 |
| BV-ICEx2 | 45 | 37 | 91% ORR 74% CR | 75% | 2-year: 80.4% | Lynch et al Lancet Haematol 2021 |
| Sequential BV-ICE | 46 | 20 | 76% CR | 98% | 2-year: 80% | Moskowitz et al Lancet Onc 2015 |
| BV-DHAPx3 | 55 | 27 | 90% ORR | 100% | 2-year: 74% | Kersten et al Haematologica 2021 |
| BRESHAPx3 | 66 | 27 | 91% ORR 70% CR | 70% | 30-month: 71% | Garcia-Sanz et al Ann Oncol 2019 |
| BV-nivolumab | 126 | 24 | 88% ORR 60.7% CR | 36% Included post-ASCT | Not reached | Diefenbach et al. ASH 2023 (abstract) |
| BV-nivolumab | 91 | 34.3 | 85% ORR | 92% | 3-year: 77% (all) 91% (per protocol) | Advani et al Blood 2021 |
A sequential BV-chemotherapy strategy offers a potentially less toxic approach for patients achieving an adequate response to BV. A phase 2 study evaluated PET-adapted sequential BV-ICE.32 BV 1.2 mg/kg was administered on days 1, 8, and 15 for two 28-day cycles followed by iPET. Those achieving CR (DS1-2) proceeded to ASCT, while patients with residual disease received ICE x 2.32 This strategy allowed 27% of patients to proceed to ASCT after BV alone, with favorable 2-year event-free survival of 80% for the full cohort. A similar PET-directed strategy utilizing BV x 2 followed by dose-escalated BV x 2 (2.4 mg/kg) for patients with stable disease or partial response, then additional pre-ASCT therapy per investigator's discretion, demonstrated 43% CR with BV alone.33
Lastly, the combination of BV-nivolumab has been assessed as a bridge to ASCT. A phase 1/2 study demonstrated an ORR of 85% and a CR rate of 67%, with 3-year PFS of 77% for the full cohort, of whom 92% ultimately underwent ASCT.34 For patients proceeding directly to ASCT per protocol after study treatment, the estimated 3-year PFS was 91%.34 A recent phase 2 ECOG study compared BV-nivolumab to the triplet combination of BV-nivolumab-ipilimumab, with similar CR rates (60.7% versus 66.7%, P = 0.31) but higher toxicity in the triplet arm.35
Cumulatively, these studies suggest that BV can be combined with other agents relatively safely with high CR rates and a potential to improve outcomes with ASCT. The role of BV as a salvage agent is likely to increase as more patients receive CPI-based frontline therapy.
CLINICAL CASE (continued)
Since our patient relapsed around 1 year after primary treatment with BV-AVD, we opted to treat her cautiously with a CPI and BV combination.28 PET after 2 cycles demonstrated a CR, and she proceeded to ASCT without exacerbation of autoimmune disease.
Maintenance therapy after transplant
While many patients are cured by ASCT, a subset do relapse and experience poor outcomes.36 The phase 3 randomized AETHERA trial evaluated BV monotherapy as a maintenance strategy after transplant for high-risk patients defined as having primary refractory disease, relapse <1 year after initial treatment, or extranodal disease at relapse.37 Patients randomized to receive BV for up to 16 cycles experienced significantly improved 5-year PFS versus placebo (59% versus 41%).37 Based on these results, BV monotherapy was FDA-approved for posttransplant maintenance.
With the increased use of BV in the frontline setting, extrapolating the results of the AETHERA trial is difficult, as all patients were BV-naive.37 This question has been explored in several retrospective series. In a large US study, the benefit of BV maintenance appeared limited to patients who had not received a novel agent pre-ASCT.38 In contrast, in the nationwide French AMAHRELIS cohort, 70% of patients receiving BV maintenance (n = 81) had received BV prior to ASCT, with no PFS difference seen between patients with or without prior BV exposure.39 Likewise, in retrospective Spanish data, posttransplant BV was associated with superior PFS as compared to no maintenance, regardless of prior BV exposure.40
The majority of patients in AETHERA (53%) did not complete the planned 16 doses of BV, primarily due to adverse events (69%).37 In a retrospective US study evaluating dose intensity during real-world maintenance, 44% of patients had prior BV exposure and only 14% completed 16 doses.41 However, PFS did not significantly differ across dose intensities, with 2-year PFS of 89.2% for patients receiving >75% of the planned BV dose and 77.9% for patients receiving ≤50% (P = 0.70).41 While additional data are required to define an optimal maintenance approach based on prior therapies, emerging evidence seems to support a benefit for post-ASCT BV in selected preexposed patients even at lower dose intensities.
CLINICAL CASE (continued)
As our patient did not have neuropathy, we offered her BV maintenance up to a cumulative lifetime dosage equivalent to the total used in AETHERA (16 doses at 1.8 mg/kg), assuming she continued to tolerate the therapy.
Role of BV in patients ≥60 years of age or anthracycline ineligible
Patients diagnosed with cHL at ≥60 years of age represent a high-risk patient population. In addition to baseline clinical comorbidities and performance status, high-risk patients' outcomes with standard regimens including ABVD and BV-AVD are inferior to those seen in patients <60 years, with increased toxicity and high rates of treatment discontinuation.42,43
Alternative BV-containing regimens have been evaluated in older patients. A phase 2 study utilized a sequential approach with BV monotherapy x 2 followed by AVD x 6 cycles.44 Patients with a clinical response received consolidation with BV x 4 cycles. The median age was 69 years, and a predominant percentage of patients had advanced stage disease (81%). Most patients completed planned chemotherapy (77% completing AVD x 6) and received at least 1 dose of BV consolidation (73%), with an ORR of 95% and a CR rate of 90%. The 2-year PFS was 84% and 2-year OS was 93%.44 Among patients discontinuing therapy due to toxicity, 75% had an ongoing CR. Sequential BV-AVD represents a reasonable choice for anthracycline-eligible patients, especially those who may have contraindications to CPI and are unable to receive N-AVD.
For anthracycline-ineligible patients, a phase 2 study evaluated BV in combination with dacarbazine for an extended duration (up to 16 cycles), with an ORR of 95% and median PFS of 47.2 months.45 In another arm of the same study, BV-nivolumab showed an ORR of 85% with median PFS not reached at 51.6 months. These results suggest either combination could benefit selected anthracycline-ineligible patients.
Conclusions
With a targeted mechanism of action and manageable safety profile, BV has demonstrated efficacy in clinical scenarios ranging from frontline treatment to posttransplant maintenance. The frontline role of BV continues to evolve and is increasingly challenged by emerging data with CPI-based therapies. For early-stage disease, the high CR rates observed when BV is incorporated in the frontline setting could potentially allow for omission of radiotherapy. This is being investigated in several studies, including the international phase 3 RADAR trial comparing BV-AVD with ABVD and the US intergroup study AHOD2131 comparing BV-nivolumab to chemotherapy.46 In both trials, no ISRT is administered for patients with negative iPET. For patients with advanced stage disease and comorbidities such as autoimmune disease precluding the use of CPI, BV-AVD or BrECADD remain viable options, and BV-nivolumab has demonstrated efficacy in patients who cannot receive anthracycline-based chemotherapy. As novel agents are used increasingly in the frontline therapy, their optimal efficacy and sequencing in subsequent lines of therapy and maintenance will need to be evaluated.
Conflict-of-interest disclosure
Joseph G. Schroers-Martin: no competing financial interests to declare.
Ranjana Advani reports research funding from Genentech/Roche, Gilead, Merck, Millennium, Pharmacyclics, Regeneron, BeiGene, and Seagen Inc and has served as a consultant for Autolus, Genentech/Roche, Gilead, and ADCT.
Off-label drug use
Joseph G. Schroers-Martin: There is discussion of off label drug use: frontline use of BV for early stage Hodgkin lymphoma, frontline use of checkpoint inhibitors.
Ranjana Advani: There is discussion of off label drug use: frontline use of BV for early stage Hodgkin lymphoma, frontline use of checkpoint inhibitors.