Abstract
X-linked severe combined immunodeficiency (XSCID) is caused by mutations of the common gamma chain of cytokine receptors, γc. Because bone marrow transplantation (BMT) for XSCID does not provide complete immune reconstitution for many patients and because of the natural selective advantage conferred on lymphoid progenitors by the expression of normal γc, XSCID is a good candidate disease for therapeutic retroviral gene transfer to hematopoietic stem cells. We studied XSCID patients who have persistent defects in B-cell and/or combined B- and T-cell function despite having received T cell–depleted haploidentical BMT. We compared transduction of autologous B-cell lines and granulocyte colony-stimulating factor–mobilized peripheral CD34+ cells from these patients using an MFGS retrovirus vector containing the γc gene IL2RG pseudotyped with amphotropic, gibbon ape leukemia virus, or RD114 envelopes. Transduced B-cell lines and peripheral CD34+ cells demonstrated provirus integration and new cell-surface γc expression. The chimeric sheep model was exploited to test development of XSCID CD34+ cells into mature myeloid and lymphoid lineages. Transduced and untransduced XSCID CD34+ cells injected into developing sheep fetuses gave rise to myeloid cells. However, only transduced γ progenitors from XSCID patients developed into T and B cells. These results suggest that gene transfer to autologous peripheral CD34+ cells using MFGS-gc retrovirus may benefit XSCID patients with persistent T- and B-cell deficits despite prior BMT.
Introduction
X-linked severe combined immunodeficiency (XSCID) is caused by mutations in the IL2RG gene leading to absent or defective common gamma chain protein (γc), a component of receptors for interleukin-2 (IL-2) and other cytokines, IL-4, IL-7, IL-9, IL-15, and IL-21.1-3 Because γc is crucial to several steps in lymphocyte development, proliferation, and activation, XSCID patients lack T cells and natural killer (NK) cells. Although B lymphocytes are present, they are nonfunctional.4-8 The profound impairment of cellular and humoral immunity in XSCID patients makes them susceptible to chronic diarrhea, failure to thrive, and severe infections, often with opportunistic organisms. In the absence of immune reconstitution by allogeneic bone marrow transplantation (BMT), XSCID patients generally die within the first 2 years of life. While HLA-identical or T cell–depleted haploidentical BMT has effectively reconstituted T-cell immunity, many XSCID patients who have received transplants have predominantly host-derived B cells, fail to make specific antibodies, and depend on chronic immunoglobulin-replacement therapy.8-10 It is not clear why BMT for XSCID and JAK3-deficient SCID, which share the T−B+phenotype, has readily given rise to donor T cells, but often failed to give rise to donor B cells, whether or not cytoreductive conditioning was given prior to BMT. A long-term study of chimerism and B-cell function in post-BMT T−B+ SCID patients found that donor-derived B cells developed in 1 of 8 XSCID patients who did not receive conditioning and in none of 6 XSCID patients conditioned with busulfan and cyclophosphamide.10
Gene transfer into autologous hematopoietic stem cells may become an alternative to current standard treatment with BMT or an adjunctive post-BMT therapy. The biology of γc makes XSCID a favorable disease for treatment by gene therapy. Lymphocytes expressing functional γc have a strong in vivo selective advantage, as demonstrated by female carriers of IL2RG mutations, whose lymphocytes have nonrandom X-chromosome inactivation with the mutation-bearing X inactive,11 as well as by a patient who developed functional T cells following spontaneous reversion of an inherited IL2RG mutation in a lymphoid progenitor.12 In addition, γc is widely and constitutively expressed on all hematopoietic lineages and is not tightly regulated.13 14 Finally, because the XSCID phenotype is an immunodeficiency, immune-mediated elimination of corrected cells is not expected. Thus transfer of a correct copy ofIL2RG into even a small number of long-lived, self-renewing hematopoietic stem cells could give rise to an expanded pool of lymphoid precursors and a continuous supply of functional γ lymphocytes.
Several in vitro studies have demonstrated retroviral transduction of normal IL2RG complementary DNA (cDNA) into B-cell lines from XSCID patients with restoration of cell-surface γc and ability to respond to IL-2 and IL-4.15-17 Immunodeficiency in mice deficient in γc has also been corrected byex vivo gene transfer,18-20 and high-level, long-term expression of human γc on lymphocytes of normal dogs has been achieved.21 Moreover, preliminary correction of disease phenotype has occurred in 4 of 5 XSCID infants who, instead of the standard BMT treatment, received gene transfer into autologous bone marrow CD34+ cells.22 23 The patients who demonstrated T-cell recovery following gene transfer also developed a small percentage of provirus-positive B cells and specific antibody responses during the first 2 years of follow-up. The disparity between T-cell and B-cell development from transduced γhematopoietic stem cells may be similar to that seen in post-BMT XSCID patients.
In recent work by our group, IL2RG was transduced into γ murine bone marrow, which was then transplanted into either γ or stem-cell deficientW/Wv recipient mice.20Constructs that placed IL2RG into 5 retrovirus vector backbones showed that all gave rise to γ T and B cells in γ recipients. However, only MFGS-gc (a Moloney murine leukemia virus vector modified to contain a splice site and into which IL2RG cDNA was inserted), which expressed the highest levels of γc, permitted γB-cell development in W/Wv recipients. The finding that MFGS-gc–transduced B-cell progenitors successfully outcompeted endogenous W/Wv B progenitors suggested that high-level γc expression following gene transfer into autologous hematopoietic stem cells might correct the B-cell as well as T-cell lineage in humans with XSCID.
The choice of retrovirus envelope also affects transduction efficiency of retroviral vectors into human hematopoietic progenitors. Most vectors used to date for gene transfer into human cells have had the amphotropic envelope.24 However, transduction efficiency is poor, consistent with the very low levels of amphotropic envelope receptor expressed by highly enriched human hematopoietic cell populations.25,26 Therefore alternative envelopes have been considered for transduction of human hematopoietic stem cells. The gibbon ape leukemia virus (GALV) and the feline endogenous virus RD114 permit transduction of human hematopoietic cells,27-35 and their receptors are expressed at higher levels than the amphotropic receptor on CD34+CD38− human and baboon bone marrow cells.36,37 Retrovirus marking of human cells maturing in nonobese diabetic/SCID (NOD/SCID) mice has shown that GALV-pseudotyped viruses were more efficient than amphotropic viruses for gene transfer.32,33,38-40 The GALV envelope was also superior to the amphotropic envelope in baboon studies.41RD114-pseudotyped vector particles demonstrated better gene transfer into human CD34+ cord blood cells than either amphotropic or GALV-pseudotyped particles.35
In the present study, we compared amphotropic, GALV-pseudotyped, and RD114-pseudotyped MFGS-gc vectors by transducing autologous cells from post-BMT XSCID patients who had persistent defects in B-cell immunity or combined B- and T-cell immunity. Both XSCID B-cell lines and mobilized peripheral blood CD34+ hematopoietic progenitors demonstrated provirus integration and new cell-surface γcexpression. The chimeric sheep model was exploited to test development of XSCID CD34+ cells into mature myeloid and lymphoid lineages without and with retrovirus correction. Although human myeloid cells were recovered from sheep injected during gestation with either untransduced or transduced CD34+ cells, only transduced γ progenitors from XSCID patients developed into T and B cells.
Patients, materials, and methods
Human subjects, cell lines, and primary cells
Healthy volunteers and 4 XSCID patients (Table 1) were enrolled in National Institutes of Health–approved protocols with informed consent. Each of the XSCID patients, despite 1 to 4 attempted BMTs without prior cytoablative conditioning, had no specific antibody responses and continued to require immunoglobulin replacement. Epstein-Barr virus (EBV)–transformed B-cell lines had been established by standard techniques from control subjects and XSCID patients prior to BMT.7 B-cell lines were cultured in complete medium consisting of RPMI 1640 (Life Technologies, Gaithersburg, MD) supplemented with 20% fetal bovine serum (FBS) (Hyclone, Logan, UT), 2 mM l-glutamine, and penicillin/streptomycin at 37°C, 5% CO2.
Volunteers and XSCID patients were given subcutaneous injections of granuloctyle colony-stimulating factor (G-CSF) (Filgrastim) (Amgen, Thousand Oaks, CA) 10 μg/kg/d for 5 days.42 On day 5, leukapheresis was performed by means of a Fenwal CS3000 continuous-flow blood cell separator (Baxter Healthcare, Deerfield, IL). CD34+ cells were purified by means of the Isolex 300I paramagnetic bead immunoaffinity-positive selection system (Newell, Irvine, CA). CD34+ cells were either used fresh or cryopreserved and thawed for transduction experiments. Human cord blood cells were purchased from National Disease Research Interchange (Philadelphia, PA).
DNA fingerprinting of posttransplantation XSCID patients.
Donor and recipient cells were detected by quantitative analysis of informative microsatellite DNA sequences. DNA was extracted from CD3+ T cells, CD19+ B cells, CD15+neutrophils, and NK cells isolated from peripheral blood with immunomagnetic beads. Similarly, CD34+ hematopoetic progenitor cells were isolated from peripheral blood of the XSCID patients after treatment with G-CSF. Microsatellite sequences were amplified by polymerase chain reaction (PCR) with a multiplex kit (Ampfister Cofiler or Profiler; Perkin-Elmer Applied Biosystems, Foster City, CA).43 PCR products were analyzed on an automated DNA sequencer (Model 310, Perkin-Elmer Applied Biosystems) with GeneScan software (ABI Prism, version 3.1, Perkin-Elmer Applied Biosystems). The proportions of amplified products representing bone marrow donor–specific and recipient–specific microsatellite alleles were calculated from the peak areas under the curves representing each allele.
MFGS-gc–pseudotyped retrovirus producer lines.
PG13 and FLYRD18 packaging cell lines were cultured in Dulbecco modified Eagle minimum essential medium supplemented with 10% newborn calf serum, 2 mM l-glutamine, and penicillin/streptomycin (Life Technologies). The 293SPA packaging cell line was cultured in improved modified Eagle medium zinc option medium with 10% FBS and 2 mMl-glutamine.
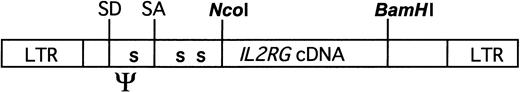
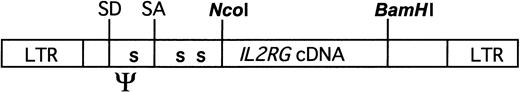
The MFGS-gc vector was generated by cloning the human IL2RGcDNA into the NcoI and BamHI sites of MFGS (Figure 1).20 An amphotropic MFGS-gc producer line was made by transfection of 293SPA cells with the MFGS-gc plasmid by calcium-phosphate coprecipitation followed by colony selection. GALV-pseudotyped MFGS-gc was produced by transducing PG13 packaging cells44 with supernatant from the ecotropic GP+E86 MFGS-gc.20RD114-pseudotyped MFGS-gc was prepared by transducing the FLYRD18 packaging cell line with supernatant from PG13 MFGS-gc. Transduced cells were sorted after immunofluorescent staining of γcby means of the monoclonal antibody TUGh4 (Pharmingen, San Diego, CA) with a FACS Vantage flow cytometer (Becton Dickinson, San Jose, CA). The brightest cells were plated at limiting dilution. RNA was extracted from conditioned medium of individual clones and, for comparison, a producer line bearing IL2RG and a selectable marker for which titers had been directly measured as 1.7 × 107 on 3T3 cells.21 The RNA was analyzed semiquantitatively by slot blot (Schleicher & Schuell, Knee, NH), and MFGS-gc clones giving signals equal to the control were selected for subsequent experiments. All MFGS-gc producer cell lines generated sufficient titers of retrovirus particles to transduce full-length provirus into K562 cells at single-copy levels, as determined by Southern blot analysis (not shown).
MFGS-gc vector.
IL2RG cDNA was inserted into NcoI andBamHI sites of MFGS, derived from Moloney murine leukemia virus. In addition to packaging and splice sites, 3 nucleotide substitutions have been engineered at positions 1256, 1273, and 1478 of the plasmid to produce termination codons (S) in all reading frames.
MFGS-gc vector.
IL2RG cDNA was inserted into NcoI andBamHI sites of MFGS, derived from Moloney murine leukemia virus. In addition to packaging and splice sites, 3 nucleotide substitutions have been engineered at positions 1256, 1273, and 1478 of the plasmid to produce termination codons (S) in all reading frames.
Retroviral transduction
EBV-transformed B cells were cultured overnight without serum and then placed in RPMI 1640 medium supplemented with 20% FBS, 2 mMl-glutamine, and penicillin/streptomycin for 4-hour recovery at 37°C, 5% CO2. The cells were then cultured at 5 × 105/mL in 24-well polystyrene plates coated with fibronectin (Retronectin CH-296; Takara Shuzo, Otsu, Japan), in 50% filtered supernatant from amphotropic, GALV- or RD114-enveloped retrovirus producer cells supplemented with 6 μg/mL polybrene (Sigma, St Louis, MO). The B cells were placed at 32°C, 5% CO2 for 2 hours15 21 followed by 7 hours at 37°C. Transductions of B-cell lines were performed on 2 consecutive days. Following the second transduction, cells were cultured in complete medium supplemented with IL-2 (Hoffman-LaRoche, Nutley, NJ). After 2 to 3 days of growth, a third and fourth transduction were performed as above.
CD34+ cells were transduced following previously described protocols.35,45 Briefly, purified mobilized peripheral CD34+ cells were prestimulated by culturing overnight in X-Vivo 10 medium (BioWhittaker, Walkersville, MD) containing 1% human serum albumin and cytokines at 37°C in 5% CO2. Cytokines used for transductions with amphotropic and GALV-pseudotyped viruses were Pixykine (IL-3/granulocyte-macrophage–CSF fusion protein; 50 ng/mL) (Immunex, Seattle, WA); Flt-3 ligand (100 ng/mL); and stem cell factor (SCF) (50 ng/mL). In some experiments, IL-6 (50 ng/mL), IL-3 (1 ng/mL), and G-CSF (10 ng/mL) were substituted for Pixykine. For transduction with the RD114-pseudotyped vector, the cytokine cocktail consisted of Flt-3 ligand (300 ng/mL), SCF (300 ng/mL), and IL-6 (50 ng/mL). Transductions were performed in fibronectin-coated wells with 1 to 1.5 × 106 cells per well and 1 to 2 × 105 cells per milliliter. Cytokines other than Pixykine were from R&D Systems (Minneapolis, MN). Following prestimulation, transductions with amphotropic and GALV-pseudotyped retroviruses were performed as daily 6- to 7-hour incubations on 4 consecutive days with 90% fresh, filtered virus supernatant supplemented with 6 μg/mL polybrene. RD114 transductions were performed by adding the stimulated cells to fibronectin-coated wells that had been preloaded with retroviral particles on day 2 of cytokine activation as described by Kelly et al.35
In utero transplantation to generate human-sheep chimeras
Following transduction, CD34+ cells were resuspended in medium containing 10% FBS and sent by overnight mail for injection into preimmune fetal sheep at 55 to 60 days of gestation by means of the amniotic bubble procedure described previously.46 An average of 5 × 105 untransduced, mobilized peripheral blood CD34+ cells from a healthy adult donor were injected into 3 sheep fetuses. Another sheep fetus received 1 × 105 untransduced human cord blood CD34+cells. Two fetuses received an average of 4 × 105untransduced XSCID CD34+ cells from patient 1; 5 fetuses each received 1.8 × 105 RD114-transduced XSCID CD34+ cells, also from patient 1. Single sheep fetuses each received either 2 × 106 untransduced or 5 × 106 RD114-transduced XSCID CD34+ cells from patient 3.
Detection of provirus DNA
Semiquantitative PCR and Southern blot analysis were performed on DNA isolated from untransduced and transduced B-cell lines and CD34+ cells of patients and healthy controls. Human lymphoid and myeloid cells were recovered from peripheral blood of human-sheep chimeras by means of serial immunomagnetic bead selection of CD3+, CD19+, CD14+, and CD45+ cells (Dynabeads M-450; Dynal, Lake Success, NY).
For PCR, the 5′ primer (5′-CAGTGTTTTGTGTTCAATGTCG) and 3′ primer (5′-TGCAGTTTTAGCA TCTGTGTGG) were located in exons 2 and 3, respectively, of human IL2RG, allowing coamplification of both a genomic DNA segment spanning intron 2 (473 base pairs [bp]) and a provirus cDNA segment (265 bp). Each PCR reaction contained32P–deoxycytidine 5′-triphosphate (dCTP) and was carried out with 35 cycles of 94°C for 20 seconds, 60°C for 20 seconds, and 72°C for 1 minute. The genomic and cDNAIL2RG signals were quantitated with a Molecular Dynamics PhosphorImager and ImageQuant software (both from Molecular Dynamics, Sunnyvale, CA), with the genomic IL2RGband used as an internal control (modified from Aviles Mendoza et al20).
Southern blotting of SstI-digested DNA was performed by means of 32P-dCTP–labeled IL2RGcDNA as a probe.
Analysis of transduced cells
Expression of γc.
Untransduced and transduced control and XSCID cells were stained with phycoerythrin (PE)-conjugated anti–human γc after blocking with isotype control, purified rat immunoglobulin G2b (IgG2b) isotype. Cells were stained for 30 minutes on ice, washed, and analyzed by either a FACScan or a FACSCalibur (Becton Dickinson) and FlowJo software (Tree Star, version 3.3.4, San Carlos, CA). Analysis was based on a live cell gate on side-scatter versus forward-scatter dot plots. The percentage of positive cells was estimated by a gate including fewer than 1.0% of cells exposed to isotype alone.
Restoration of γc function.
Restoration of γc function following retrovirus transduction was assayed in patient B-cell lines by Western and flow cytometric analyses by means of a mouse monoclonal antibody to phosphorylated signal transducer and activator of transcription 5 (p-STAT5) antibody (Zymed Laboratories, San Francisco, CA) to detect downstream signaling following IL-2 stimulation. Cells were acid washed to remove bound cytokines, exposed to IL-2 for 10 minutes, and then probed or stained for p-STAT5. For Western blots, goat anti–mouse IgG heavy and light chain (H&L)–conjugated with horseradish peroxidase (Zymed) was used as the secondary antibody. Fluorescein isothiocyanate (FITC)–conjugated goat anti–mouse IgG H&L (CalTag, Burlingame, CA) was used as a secondary antibody for flow cytometric analysis of p-STAT5. Isotype control for flow cytometry was FITC-conjugated mouse IgG1κ. Cells stimulated with IL-2 were compared with unstimulated cells. For flow cytometric analysis, the percentage of p-STAT5+ cells was estimated by an isotype gate of fewer than 1.0%.
Analysis of γc expression in human-sheep chimeras.
Peripheral blood was harvested from sheep at 1 to 3 months and from selected sheep again at 10 months of age. Blood was analyzed for the presence of human cells by staining with human-specific monoclonal antibodies directly conjugated with FITC, PE, CyChrome, and allophycocyanin (APC), including CD45, CD3, CD19 CD20, CD132 (TUGh4), CD11b, and CD15 (Pharmingen). Only cells within live mononuclear cell or lymphocyte gates on side-scatter versus forward-scatter dot plots were analyzed. The overall percentage of human CD45+ mononuclear cells and the percentage of CD45+ mononuclear cells that were myeloid cells (CD45+CD11b+CD15+, CD45+CD11b+CD15−, and CD45+CD11b−CD15+ or CD45+CD3−CD20−), T cells (CD45+CD3+ CD19/CD20−), and B cells (CD45+CD19/CD20+CD3−) were determined. The percentages of T and B cells were calculated as the ratio of T cells to lymphoid-plus-myeloid cells and B cells to lymphoid-plus-myeloid cells. Double-gated populations (CD45+ plus appropriate lymphoid or myeloid markers) were then analyzed for human γc, or CD132, expression.
Statistical analysis
We performed χ2 tests using the population comparison platform in the FlowJo software package. The platform allows direct comparison between different populations through the Probability Binning (Chi(T) or PB) comparison algorithm, related to the Cox χ2 approach. The χ2 is converted into a metric, T(χ), that can be used to estimate the probability that a test population is different from a control population. When T(χ) = 0, the 2 populations are indistinguishable (P = .5). When T(χ) = 1, the populations differ by 1 SD, giving the probability that the 2 populations differ as P < .17. A T(χ) that exceeds 4 implies that the 2 distributions are different, withP < .01 (99% confidence). All reported nonzero percentages for cell populations are statistically different from control populations.
Results
Donor cell engraftment in posttransplantation XSCID patients
Table 1 summarizes the mutations inIL2RG, BMT treatment and outcome, and latest lymphocyte functional status of the 4 XSCID patients. Patient 1 carried a nonsenseIL2RG mutation in exon 5, causing undetectable levels of messenger RNA (mRNA) and no cell-surface γc in EBV-transformed B-cell lines. Patient 2 had a defect in the poly(adenylic acid) addition signal of IL2RG, with absent to trace amounts of γc. Patients 3 and 4 had mutations truncating the intracellular domain, but resulting in normal γc expression at the cell surface. All XSCID patients included in this study had received haploidentical, parental T cell–depleted transplants without cytoreductive conditioning within the first year of life, but had not achieved full reconstitution of their immune systems (Table 1). They continued to require immunoglobulin replacement and additional treatments as noted. Patients 2 and 3 were lymphopenic, with poor to absent T-cell responses to mitogens and antigens as compared with healthy controls.
Chimerism analysis by PCR was performed to delineate the post-BMT donor and host contributions to hematopoietic lineages in our patients (Table1). No patient had any detectable donor-derived alleles in DNA from myeloid cells. Patient 2 had no detectable donor cell alleles in either T- or B-cell compartments. Patients 1, 3, and 4 had 5% or fewer donor B cells. The same assay was used to analyze CD34+progenitor cells purified after G-CSF mobilization and apheresis. In no patient were donor-derived hematopoietic progenitor cells detectable.
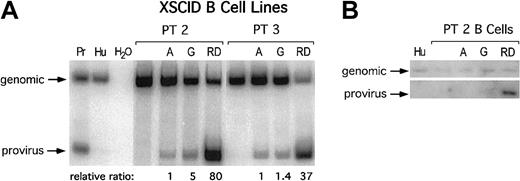
Retroviral transduction of patient cells
Titers of the producer lines were estimated by Southern blotting and RNA slot-blot analysis to be equivalent and high (see “Patients, materials, and methods”). XSCID B-cell lines were transduced as described with amphotropic, GALV-, and RD114-pseudotyped virus supernatants. With the use of coding sequence primers flankingIL2RG intron 2, genomic and provirus DNA were amplified in the same PCR reaction (Figure 2A). Provirus equivalents per genome (relative to genomic signal) were calculated, and within each set of transductions, a relative ratio of provirus integration was obtained by normalizing to the amphotropic virus transduction rate. For all XSCID patients and controls, transduction with GALV- and RD114-pseudotyped viruses produced higher rates of provirus integration than did the amphotropic virus, with RD114 more than 10-fold higher than either of the other 2. The relative amounts of provirus integration were further analyzed by Southern blot, confirming that the RD114 envelope afforded the most provirus integration, followed by GALV and then amphotropic (Figure2B).
Detection of provirus versus genomic DNA in transduced patient cell lines.
(A) PCR using primers flanking IL2RG intron 3 coamplified genomic and provirus DNA in a single PCR reaction to estimate provirus equivalents per genome. Pr indicates producer line 293SPA MFGS-gc; Hu, human genomic DNA. Representative transductions of cell lines from patients 2 and 3 with amphotropic (A)– GALV (G)–, and RD114 (RD)–enveloped retrovirus. (B) Southern blot analysis ofSstI–digested DNA probed with IL2RG cDNA to detect both genomic and provirus DNA.
Detection of provirus versus genomic DNA in transduced patient cell lines.
(A) PCR using primers flanking IL2RG intron 3 coamplified genomic and provirus DNA in a single PCR reaction to estimate provirus equivalents per genome. Pr indicates producer line 293SPA MFGS-gc; Hu, human genomic DNA. Representative transductions of cell lines from patients 2 and 3 with amphotropic (A)– GALV (G)–, and RD114 (RD)–enveloped retrovirus. (B) Southern blot analysis ofSstI–digested DNA probed with IL2RG cDNA to detect both genomic and provirus DNA.
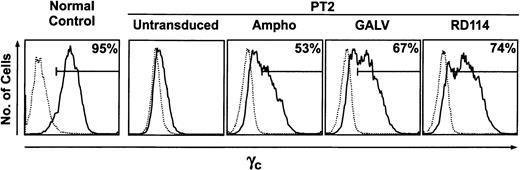
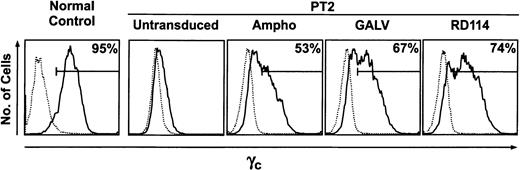
Transduced B-cell lines from patient 1, patient 2 (both γ), and patient 3 (expressing intracellularly truncated γc) were analyzed by immunofluorescence for cell-surface γc protein; a representative transduction of patient 2 cells is shown in Figure 3. Patient cell lines without γc became positive, and cells with defective γc had increased fluorescence following transduction, consistent with the addition of provirally expressed γc protein. RD114-pseudotyped virus consistently gave the highest proportions of γ cells. On average, 14% of γ cells transduced with the amphotropic retrovirus became γ; 17% newly expressed γcafter transduction with the GALV virus, and 39% after transduction with the RD114 virus (Table 2). GALV- and RD114-pseudotyped viruses, but not amphotropic virus, achieved levels of γc expression, estimated by geometric mean channel (GMC) values, comparable to those of γ EBV B cells from healthy donors (not shown). In the patient 3 B-cell line expressing defective γc, successful transduction was demonstrated by an increased GMC of γ cells; untransduced γ cells had a GMC of 394, and amphotropic, GALV, and RD114 virus transductions increased the GMC by 41, 50, and 114 channels, respectively (Table 2).
Expression of γc protein on B-cell lines.
Cells from a healthy control, left. Untransduced and transduced cells from patient 2, right. Black line, cells stained with TUGh4 (anti-CD132 γc antibody); dotted line, isotype controls. Percentage of γ cells determined by inflection points of histograms.
Expression of γc protein on B-cell lines.
Cells from a healthy control, left. Untransduced and transduced cells from patient 2, right. Black line, cells stained with TUGh4 (anti-CD132 γc antibody); dotted line, isotype controls. Percentage of γ cells determined by inflection points of histograms.
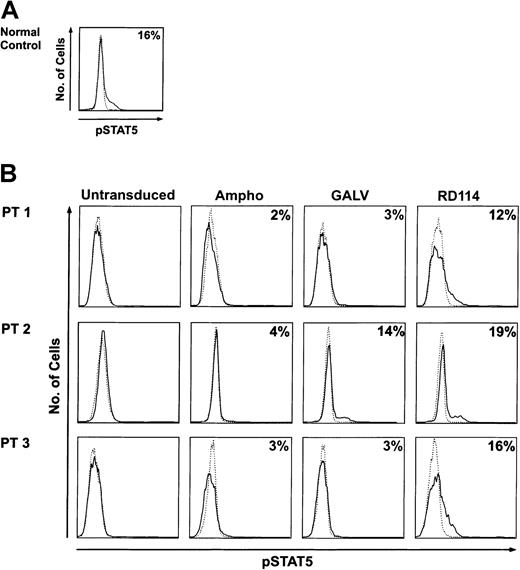
Restoration of γc function in XSCID cells following retrovirus transduction
To test integrity of the γc signaling pathway, we took advantage of the specificity of the interaction of γc with JAK3 and the subsequent activation of STAT5, using IL-2–induced pSTAT5 as an indicator of γc signal transduction. We found no pSTAT5 by Western analysis in untransduced B-cell lines from XSCID patients, but detectable pSTAT5 in all transduced cell lines following IL-2 stimulation (not shown). In contrast to normal control cells assayed by flow cytometry (Figure4A), untransduced XSCID cells had no pSTAT5 following IL-2 exposure. The proportion of pSTAT5 in transduced cells matched that of cells to which γc expression was newly restored (Figure 4B). Comparison of IL-2–stimulated cells with their unstimulated controls showed that untransduced XSCID B-cell lines did not phosphorylate STAT5. Trace amounts of pSTAT5 induced by IL-2 exposure were detected in cells transduced with amphotropic-enveloped MFGS-gc. Higher amounts of pSTAT5 production on average were achieved with GALV MFGS-gc, but the highest proportion of pSTAT5+cells was seen following transduction with RD114 MFGS-gc. In the latter cells, the levels of pSTAT5 were comparable to those seen in cells from normal controls (Figure 4A). For the XSCID B-cell line of patient 3 with truncated γc, detection of pSTAT5 was more informative than cell-surface staining for γc.
Phosphorylated STAT5 (pSTAT5) as an indicator of γc signaling.
B-cell lines from a healthy control (panel A) and XSCID patients (panel B), before and after transduction. Cells were exposed (black line) or not exposed (dotted line) to IL-2, then permeabilized and stained with mouse anti-pSTAT5 and a FITC-conjugated anti–mouse secondary antibody.
Phosphorylated STAT5 (pSTAT5) as an indicator of γc signaling.
B-cell lines from a healthy control (panel A) and XSCID patients (panel B), before and after transduction. Cells were exposed (black line) or not exposed (dotted line) to IL-2, then permeabilized and stained with mouse anti-pSTAT5 and a FITC-conjugated anti–mouse secondary antibody.
Engraftment and lineage development of human cells in sheep
To evaluate whether transduced γc-deficient CD34+ cells could differentiate into T and B lymphocytes, thus demonstrating correction of the XSCID defect, we transplanted the human cells into fetal sheep to create stable chimeras. In a preliminary experiment (Table 3), we compared CD34+ cells from normal cord blood, known to have high numbers of hematopoietic stem cells, to peripheral blood CD34+ cells obtained from a healthy donor using our G-CSF mobilization protocol. Immunomagnetic bead–selected CD34+cells from freshly harvested cord blood were cultured for 4 days in cytokine-supplemented medium and then injected into a preimmune sheep fetus. Another sheep fetus received cytokine-cultured mobilized peripheral blood CD34+ cells from a healthy adult. At 1 month after birth of the sheep, their peripheral blood was analyzed for human cell engraftment. Comparable levels of chimerism were found in the recipient of cord blood and of peripheral blood, 3.0% and 2.7%, respectively (Table 3). Similar percentages of human-derived cells were also found in the T-cell, B-cell, and myeloid lineages. The γc-expression profiles of human lymphoid and myeloid cells were similar in the sheep engrafted with cord blood and peripheral blood CD34+ cells (not shown).
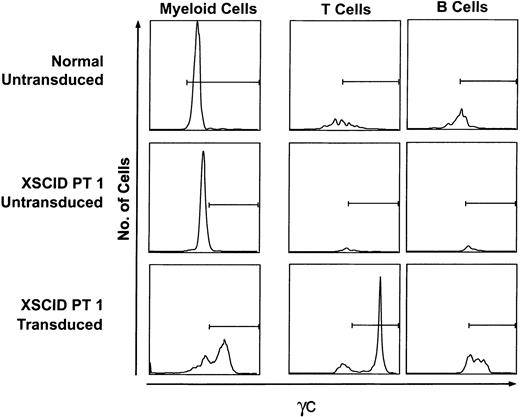
Untransduced XSCID peripheral CD34+ cells from patient 1 and patient 3 and the same cells transduced with RD114 MFGS-gc were transplanted into preimmune fetal sheep to generate human-sheep hematopoietic chimeras. Flow cytometric analyses of peripheral blood obtained postnatally from the sheep are summarized in Table4. The mononuclear cells bearing human-specific CD45 ranged from 1.4% to 5.1%. The 5 sheep that received identical aliquots of 1.8 × 105 transduced cells from patient 1 had engraftment of CD45+ human leukocytes varying from 2.0% to 5.1%, and all developed roughly similar proportions of mature human lineages. As expected, untransduced and transduced XSCID CD34+ cells were equally capable of development into human myeloid cells, demonstrated with CD11b and/or CD15, accounting for 47% to 95% of the human leukocytes. As illustrated in Figure 5, the myeloid cells were γ when derived from CD34+cells from a healthy control donor (top left panel), γ when derived from untransduced XSCID CD34+ cells (center left panel), and a mixture of γ and γ when derived from XSCID cells transduced with RD114 MFGS-gc (lower left panel). In contrast, neither T cells nor B cells developed to a significant degree from untransduced XSCID CD34+ cells (Table 4; Figure 5, center right panels). Transduced XSCID CD34+ cells were found to have regained γc function as evidenced by both lymphoid-lineage development and expression of γc on lymphoid and myeloid compartments (Table 4; Figure 5, lower right panels). Human γ T cells accounted for 4% to 43% (mean, 20%; SD, 14) of the cells bearing human CD45 in the 5 sheep that received transduced cells from patient 1 and for 7% to 10% at 2 time points in the single sheep that received transduced cells from patient 3. All 6 sheep that were transplanted with transduced XSCID CD34+ cells also developed human γ B cells.
Flow cytometric analysis of human cells from chimeric sheep.
Top panels, cells from a sheep receiving control peripheral human CD34+ cells; center panels, a sheep receiving untransduced XSCID CD34+ cells; bottom panels, a sheep receiving XSCID CD34+ cells transduced with RD114 MFGS-gc. Horizontal bars, positive γc gates based on less than 5% background γc expression of sheep cells (CD45−CD3−CD19− or CD45−CD11b−CD15−). For myeloid staining, untransplanted sheep were used as the negative control for setting gates.
Flow cytometric analysis of human cells from chimeric sheep.
Top panels, cells from a sheep receiving control peripheral human CD34+ cells; center panels, a sheep receiving untransduced XSCID CD34+ cells; bottom panels, a sheep receiving XSCID CD34+ cells transduced with RD114 MFGS-gc. Horizontal bars, positive γc gates based on less than 5% background γc expression of sheep cells (CD45−CD3−CD19− or CD45−CD11b−CD15−). For myeloid staining, untransplanted sheep were used as the negative control for setting gates.
Discussion
Post-BMT XSCID patients with varying degrees of persistent immune compromise were studied. One patient had no donor cell engraftment despite multiple attempted BMTs. The other 3 patients had T cells derived from their bone marrow donor, but B cells and myeloid cells of host origin. No patient had detectable CD34+ cells from the bone marrow transplant donor, suggesting that the stem cells or progenitors giving rise to T cells in these individuals were rare, and underlining the positive selection for T cells with intact γc. Using an MFGS-gc vector construct pseudotyped with different viral envelopes, we transferred the correctIL2RG cDNA into B-cell lines and cytokine-mobilized peripheral blood CD34+ hematopoietic stem cells from these XSCID patients. In vitro and in vivo studies demonstrated restoration of γc function in transduced patient cells. Improvement in transduction efficiency over that seen with amphotropic virus was achieved by pseudotyping with the GALV envelope, and even greater improvement was achieved by pseudotyping with the RD114 envelope.
Since the first successful BMT for XSCID was reported in 1968,47 BMT has become the standard treatment. Techniques such as T-cell depletion have improved BMT outcome for patients without an HLA-matched sibling donor, making possible survival of up to 70% to 90% or more of infants with XSCID.8,48,49 However, immune reconstitution, especially of specific antibody production by B cells, remains incomplete in many post-BMT XSCID patients,8-10 a finding possibly related to their ability to make γ B cells that are nonfunctional. Therapeutic gene transfer into autologous hematopoietic stem cells has now been carried out with promising early results by Cavazzana-Calvo et al,22 who substituted ex vivoretroviral correction of aspirated autologous bone marrow for BMT in newly diagnosed infants. Whether gene therapy may prove superior to BMT as primary treatment for XSCID remains to be shown; even the preliminary success of gene transfer in 4 of 5 XSCID infants resulted in low levels of corrected B lymphocytes.23 However, another role for gene transfer in the therapy of XSCID may be to improve immune function in the many post-BMT XSCID patients without full reconstitution.
Successful retroviral gene transfer depends on several factors involving the retrovirus vector and the target cell. The impact of retrovirus vector backbone on transgene expression was recently highlighted in a murine transplantation model by Aviles Mendoza et al.20 In a comparison of 5 retrovirus vectors containingIL2RG cDNA, the highest transgene expression level, achieved by MFGS-gc, was required to overcome competition with endogenous B-lymphoid progenitors to produce B cells in unirradiatedW/Wv hosts. We have now extended these findings by testing the hypothesis that MFGS-gc viruses of equivalent titer, but with different pseudotypes, would transduce human hematopoietic stem cells with varying efficiency and thus lead to varying degrees of functional restoration. DNA analysis of provirus in transduced patient cells illustrated the significant differences between amphotropic, GALV-pseudotyped, and RD114-pseudotyped retrovirus transduction efficiencies. As reflected in the relative ratios of provirus equivalents per genome, RD114 facilitated the transduction of the highest proportion of target cells.35 The differences observed in provirus integration paralleled the relative levels of retrovirus receptor mRNA expressed in successive enrichments for hematopoietic stem cells (D.M.B., unpublished data, December 2001). The most striking finding on DNA analysis of cells transduced with RD114-enveloped virus was that the provirus per copy number was greater than 1 (the signal from provirus cDNA exceeded that from genomic DNA). The improvement in transduction efficiency over amphotropic-enveloped virus that was achieved with the GALV and RD114 envelopes was further confirmed by analyses of new γccell-surface expression and functional γc response to stimulation with IL-2. These results suggest that the RD114 receptor, a neutral amino-acid transporter, is expressed at higher levels in human hematopoietic progenitor cells than the phosphate transporters that serve as receptors for amphotropic and GALV-enveloped retrovirus particles. Our findings are consistent with those of Kelly et al,35 who demonstrated in a NOD/SCID repopulating assay that RD114-pseudotyped vector particles were more efficient for gene transfer into human cord blood hematopoietic stem cells than were amphotropic, GALV-pseudotyped, or VSVG-pseudotyped particles. The improvement in transduction efficiency achieved with the RD114 envelope may be as significant for in vivo selection of γ-transduced cell lineages as the previously demonstrated mRNA expression levels from constructs with MFGS versus other retrovirus backbones.
The human-sheep hematopoietic chimera, an excellent model for studying human hematopoietic stem cell engraftment and maturation, has become an important tool for our preclinical evaluation of gene therapy strategies for XSCID. Despite reported phenotypic and functional differences among progenitors from mobilized peripheral blood, cord blood, and bone marrow,50-53 we achieved equivalent human lymphoid and myeloid cell development in sheep transplanted with cord blood or mobilized peripheral CD34+ cells from healthy human donors, and we showed durable human chimerism lasting for 10 months. These findings suggest that peripheral mobilized CD34+ cells are appropriate target cells for a human XSCID gene transfer trial. The sheep model also allowed us to demonstrate directly the successful development of γ human T and B cells in addition to myeloid cells in sheep transplanted with XSCID peripheral CD34+ cells transduced with MFGS-gc. Furthermore, the development of gene-corrected XSCID B cells in sheep from transplanted cells transduced with RD114 MFGS-gc offers the opportunity to define in future studies the parameters required, such as level of γc expression and proportion of transduced cells, for development of functional human B cells. Evaluation of target cells and vector constructs to treat other hematologic and immunodeficiency diseases may be facilitated by preclinical studies in human-sheep chimeras.
We thank Stacie Anderson, Gilda Linton, and Roxanne Fischer for technical assistance; Joie Davis for coordinating patient visits and samples; Charlie Carter for CD34+ cell isolation; and the XSCID patients and their families for their ongoing participation and encouragement.
Supported by the Howard Hughes Medical Institute (E.J.T.); the Veterans Administration (E.D.Z.); the Mathers Charitable Foundation (E.D.Z.); and National Institutes of Health grants HL40722, HL46566, and HL39875 (E.D.Z.).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Jennifer M. Puck, Genetics and Molecular Biology Branch, NHGRI/NIH, Bldg 49, Rm 4A14, 49 Convent Dr, Bethesda, MD 20892-4442; e-mail: jpuck@nhgri.nih.gov.