Abstract
Kallistatin is a unique serine proteinase inhibitor (serpin) and a heparin-binding protein. It has been localized in vascular smooth muscle cells and endothelial cells of human blood vessels, suggesting that kallistatin may be involved in the regulation of vascular function. Our previous study showed that kallistatin plays a role in neointima hyperplasia. In this study, we investigated the potential role of kallistatin in angiogenesis in vitro and in vivo. Purified human kallistatin significantly inhibited vascular endothelial growth factor (VEGF)– or basic fibroblast growth factor (bFGF)–induced proliferation, migration, and adhesion of cultured endothelial cells. Kallistatin attenuated VEGF- or bFGF-induced capillary density and hemoglobin content in subcutaneously implanted Matrigel plugs in mice. To further investigate the role of kallistatin in angiogenesis, we prepared adenovirus carrying the human kallistatin cDNA (Ad.HKBP) and evaluated the effect of kallistatin gene delivery on spontaneous angiogenesis in a rat model of hind-limb ischemia. Local kallistatin gene delivery significantly reduced capillary formation and regional blood perfusion recovery in the ischemic hind limb after removal of the femoral artery. Furthermore, a single intratumoral injection of Ad.HKBP into pre-established human breast tumor xenografts grown in athymic mice resulted in significant inhibition of tumor growth. CD31 immunostaining of tumor sections showed a decreased number of blood vessels in the kallistatin-treated group as compared to the control. These results demonstrate a novel role of kallistatin in the inhibition of angiogenesis and tumor growth.
Introduction
Angiogenesis is the formation of new capillaries from preexisting vasculature by migration and proliferation of endothelial cells,1 and it is a fundamental process required for a number of physiologic and pathologic events.2 In adults, angiogenesis is essential for the female reproductive cycle and for repair, remodeling, and regeneration of tissues during wound healing.3 Under physiologic conditions, angiogenesis is a highly regulated phenomenon and is under the control of balance between angiogenic stimulators and inhibitors. However, unregulated angiogenesis is observed under pathologic conditions such as tumor growth, diabetic retinopathy, and psoriasis.3,4 Angiogenesis plays an important role in tumor growth, invasion, and metastasis.5 Angiogenesis is not only a prerequisite for tumor growth but also a major factor affecting the metastatic spread of malignant cells.6Antiangiogenesis therapy using endogenous inhibitors has several advantages including decreased toxicity to host, lack of drug resistance, and broad-spectrum efficacy against tumors of varied origins.6
Serine proteinase inhibitors (serpins) are involved in a variety of physiologic events such as coagulation, fibrinolysis, complements activation, and phagocytosis by targeting toward their serine proteinases.7 However, many serpins have alternate functions independent of their regulation of proteolytic events, such as hormone transport and cell differentiation.7 Recently, serpins, such as pigment epithelium-derived factor (PEDF),8 cleaved form of antithrombin III,9and maspin,10 have been shown to have antiangiogenic activity. Kallistatin is a serpin, which was first identified as a tissue kallikrein-binding protein.11,12 Previous studies showed that kallistatin has multiple biologic functions independent of the tissue kallikrein-kinin system, including blood pressure regulation,13 protection against inflammation,14 vasculature relaxation,15 and stimulation of neointima hyperplasia.16 During physiologic or pathologic angiogenesis, kallistatin levels in the plasma of pregnant women and in vitreous fluids from patients with diabetic retinopathy are significantly lower than those in healthy individuals.17,18 Levels of immunoreactive rat kallistatin in vitreous fluids from streptozotocin-diabetic rats are significantly lower than those in normal control animals.19 Furthermore, kallistatin has been localized in vascular smooth muscle cells and endothelial cells of human blood vessels.20 These findings suggest that kallistatin may play a role as a negative regulator of angiogenesis. In this study, we investigated the potential role of kallistatin in angiogenesis in vitro and in vivo.
Materials and methods
Cell culture
Human dermal microvascular endothelial cells (HMVECs) and human breast carcinoma cell line MDA-MB-231 (HTB26) were obtained from Clonetics (San Diego, CA) and American Type Culture Collection (ATCC; Rockville, MD), respectively.
Human kallistatin purification and immunoassay
Preparation of adenovirus carrying human kallistatin cDNA
Human kallistatin full-length cDNA22 was cloned in sense orientation into the adenoviral shuttle vector pAdTrack-CMV.23 The resultant adenoviral plasmid carrying human kallistatin sense cDNA or green fluorescent protein cDNA under control of cytomegalovirus (CMV) promoter/enhancer along with all Ad5 sequences except for the E1 and E3 genes was transfected into human embryonic kidney 293 packaging cells (Quantum, Quebec, QC, Canada). Large quantities of high-titer adenoviruses were produced in human embryonic kidney 293 cells and purified by CsCl banding as previously described.24
[3H]-thymidine incorporation
The [3H]-thymidine incorporation assay was performed as previously described.25 Quiescent HMVECs were treated with recombinant human vascular endothelial growth factor (VEGF; kindly provided by Genentech, South San Francisco, CA) or basic fibroblast growth factor (bFGF; Sigma, St Louis, MO; 15 ng/mL) with or without purified human kallistatin in Medium 199 supplemented with 2% fetal bovine serum (FBS) for 18 hours, and then pulse-labeled with 1 μCi/mL (0.037 MBq) [3H]-thymidine (Dupont NEN, Boston, MA) for another 6 hours. Radioactivity was determined using a liquid scintillation counter (Packard, Downers Grove, IL). Each experiment was performed in quadruplicate.
Cell migration assay
Cell migration was assessed using a modified Boyden chamber (Costar transwell inserts; Corning, Acton, MA).26 The transwell inserts were coated with a solution of fibronectin (5 μg/mL) and type I collagen (100 μg/mL; Sigma) at 4°C overnight and then air-dried. VEGF or bFGF (15 ng/mL) with or without kallistatin (1 μM) dissolved in Medium 199 containing 0.1% bovine serum albumin (BSA) was added in the bottom chamber. HMVECs (2 × 105cells) suspended in a 200-μL aliquot of Medium 199 containing 0.1% BSA was added to the upper chamber. After 4 hours of incubation at 37°C, cells on both sides of the membrane were fixed and stained with Diff-Quik staining set (Baxter Healthcare, Dade Division, Miami, FL). Cells on the upper surface of the membrane were then mechanically removed, and the average number of cells from 5 randomly chosen high-power (× 400) fields on the lower side of the membrane was counted. Each experiment was performed in triplicate.
Cell adhesion assay
Cell adhesion assay was conducted as previously described.26 Before seeding, HMVECs at 5 × 105 cells/mL in Medium 199 supplemented with 0.1% FBS was treated with VEGF or bFGF (15 ng/mL) without or with kallistatin (1μM) for 60 minutes and plated on the fibronectin-coated 48-well plate at 0.25 mL/well. After a 90-minute incubation, cells were gently washed twice with phosphate-buffered saline (PBS) and adherent cells were fixed and stained with Diff-Quik staining set. The number of adherent cells was counted under microscopy in 7 random fields at a magnification of × 200.
Implanted Matrigel model in mice
Each male mouse (FVB, 30 g; Sprague-Dawley Harlan, Indianapolis, IN) was subcutaneously injected with 0.5 mL Matrigel (9-10 mg/mL; Becton Dickinson, Franklin Lakes, NJ) containing VEGF or bFGF (150 ng/mL) with or without kallistatin (2 μM) near the abdominal midline as previously described.27 One week later, Matrigel plugs were removed and fixed in 4% buffered formaldehyde in PBS for histologic analysis using Masson trichrome staining. The capillary-occupied area per field of view (2.26 × 104 μm2) from 15 to 20 fields (× 400 magnification) in tissue sections was measured using a computerized digital camera system (Olympus, Melville, NY) and NIH Image 1.61 (NIH, Bethesda, MD). The vessels are defined as those structures possessing a patent lumen and positive endothelial nuclei. In a parallel experiment, recovered Matrigel plugs were digested in 5 mL Drabkin reagent (Drabkin reagent kit 525; Sigma) to quantify neovessel formation by a hemoglobin assay.27
Hind-limb ischemia model in rats
Male Wistar rats (5-7 weeks old, 200 g; Sprague-Dawley Harlan) were used to create the hind-limb ischemia as previously described.28 Rats were anesthetized by intraperitoneal injection of ketamine (90 mg/kg) and xylazine (10 mg/kg). The proximal end of left femoral artery and the distal portion and side branches of the saphenous artery were ligated with 4.0 silk. The femoral artery was dissected free and excised. Adenovirus (2 × 1010 pfu virus/rat) containing human kallistatin cDNA (Ad.HKBP) or green fluorescent protein cDNA (Ad.GFP) as the control virus was injected into the 5 different sites of adductor muscle using a 27-gauge needle after removing the femoral artery. At 2 weeks after surgery, both hind-limb muscles were removed for biochemical and morphologic analyses. A Laser Doppler Perfusion Imager System (Lisca, North Brunswick, NJ) was used to evaluate blood perfusion of both left (ischemic) and right (nonischemic) hind limbs as previously described.29 Accordingly, laser Doppler color images were recorded twice and the average perfusion levels were calculated on the basis of colored histogram pixels. To minimize variables including ambient light and temperature, perfusion recovery was expressed as the ratio of left (ischemic) to right (nonischemic) hind-limb perfusion from each animal. Perfusion analyses were performed under anesthesia: (1) before surgery, (2) immediately after surgery, and at (3) 3 days, (4) 7 days, and (5) 14 days after surgery. The regional blood flow in both hind limbs of rats was measured using fluorescent microspheres (Molecular Probes, Eugene, OR) at 2 weeks after surgery as previously described.28
RT-PCR and Southern blot analysis
Total RNA was extracted from various tissues by the guanidine isothiocyanate-cesium chloride ultracentrifugation method30 at day 5 after local gene delivery. Reverse transcription (RT) was performed with 2 μg total RNA and 100 pmol random hexamers in a total volume of 20 μL to produce first-strand cDNA. The quality of RNA samples was evaluated by RT–polymerase chain reaction (RT-PCR) using cytoplasmic β-actin specific primers (sense primer, 5′-GAACCCTAAGGCCAACCGTG-3′; antisense primer, 5′-TGGCATAGAGGTCTTTACGG-3′). The levels of human kallistatin cDNAs were evaluated by PCR and Southern blot semiquantitative method. PCR experiments were performed with 1 μL of the first-strand cDNA in a 50-μL reaction mixture. Human kallistatin cDNA was amplified with specific primers for human kallistatin (sense primer, 5′-CGTCTATGAGGCTAAAC-3′; antisense primer, 5′-CTCTGGAGTCAGAACCT-3′). Amplification protocol was as follows: denaturation at 94°C for 1 minute, annealing at 52°C for 1 minute, and extension at 72°C for 1 minute. All PCRs were linear up to 30 cycles. PCR products were resolved on 0.8% agarose gels and transferred to Hybond nylon filters (Amersham Pharmacia, Piscataway, NJ). Hybridization conditions were the same as previously described.21 Oligonucleotides 5′-GTAAATGTAATTCACCAG-3′ and 5′-CGCACGATTTCCCTCTCAGC-3′ were end-labeled with γ-[32P] adenosine triphosphate (ATP) and T4 polynucleotide kinase (Life Technologies, Rockville, MD) and used as nested specific probes for human kallistatin and β-actin, respectively.
Tumor growth assay
Human breast tumor cells MDA-MB-231 (5 × 106cells) in 0.1 mL sterilized Dulbecco modified Eagle medium (DMEM) were injected subcutaneously into the dorsa of 6- to 8-week-old female nude mice (nu/nu, Sprague-Dawley Harlan; 2 injection sites/mouse). When tumors reached a volume of 50 mm3, an intratumoral injection of 109 pfu Ad.HKBP virus or Ad.GFP control virus or the same volume PBS was carried out as previously described.31 Tumor growth was monitored by external measurement in 2 dimensions weekly with calipers as previously described.32 Tumor volume was determined according to the equation: V =(L × W2) × 0.52, where V is volume, L is length, and W is width. At 21 days after virus injection, tumors were harvested and fixed in 4% neutral buffered formaldehyde in PBS for histochemistry analysis.
Immunohistochemistry
Histologic sections, 4 μm thick, prepared from paraffin-embedded tissue samples were used for immunohistochemical analysis as previously described.29 Identification of endothelial cells was performed by immunostaining for platelet endothelial cell adhesion molecule 1 (PECAM-1 or CD31) using a monoclonal antibody against rat or mouse CD31 (Pharmingen, San Diego, CA) at 1:50 dilution at 4°C overnight. Capillary positively stained with CD31 was counted under light microscopy.
Statistical analysis
Statistical significance is determined by one-way analysis of variance (ANOVA) with the Fisher multiple comparison test. All data are expressed as mean ± SEM, and differences are considered significant at P < .05.
Results
Effects of kallistatin on the proliferation, migration, and adhesion of cultured endothelial cells
Human kallistatin was purified from plasma and used to determine its effects on cultured human endothelial cells. Cell proliferation was determined by [3H]-thymidine incorporation. Exogenous kallistatin dose-dependently inhibited VEGF- or bFGF-induced endothelial cell proliferation compared to the VEGF or bFGF control, respectively (Figure 1A,B). Kallistatin also significantly inhibited VEGF- and bFGF-induced endothelial cell migration (Figure 1C) and adhesion (Figure 1D) compared to the VEGF or bFGF control, respectively. These results show that kallistatin inhibits VEGF- and bFGF-induced proliferation, migration, and adhesion of cultured endothelial cells and suggest that kallistatin is a potential angiogenesis inhibitor.
Effects of kallistatin on VEGF- and bFGF-induced proliferation, migration, and adhesion of HMVECs.
(A,B) Quiescent HMVECs were incubated with the indicated concentrations of human kallistatin (HKBP) and VEGF or bFGF (15 ng/mL) for 24 hours. DNA synthesis was measured as [3H]-thymidine incorporation. Each value represents mean ± SEM (n = 4). (C) Cell migration was determined using modified Boyden chambers. VEGF or bFGF, 15ng/mL; HKBP, 1μM. Each value represents mean ± SEM (n = 3). (D) Cell adhesion was determined using fibronectin-coated plates. VEGF or bFGF, 15 ng/mL; HKBP, 1μM. Each value represents mean ± SEM (n = 4).
Effects of kallistatin on VEGF- and bFGF-induced proliferation, migration, and adhesion of HMVECs.
(A,B) Quiescent HMVECs were incubated with the indicated concentrations of human kallistatin (HKBP) and VEGF or bFGF (15 ng/mL) for 24 hours. DNA synthesis was measured as [3H]-thymidine incorporation. Each value represents mean ± SEM (n = 4). (C) Cell migration was determined using modified Boyden chambers. VEGF or bFGF, 15ng/mL; HKBP, 1μM. Each value represents mean ± SEM (n = 3). (D) Cell adhesion was determined using fibronectin-coated plates. VEGF or bFGF, 15 ng/mL; HKBP, 1μM. Each value represents mean ± SEM (n = 4).
Kallistatin attenuates VEGF- or bFGF-induced angiogenesis in subcutaneously implanted Matrigel in mice
Based on the in vitro studies, we used the animal model of subcutaneously implanted Matrigel to evaluate the antiangiogenic effect of kallistatin in vivo. Figure 2A shows representative images of Matrigel implants stained with Masson trichrome. VEGF and bFGF significantly increased capillary density as compared to the control. Red blood cells appeared abundantly in the capillaries, indicating that these capillaries are functional. However, the mean capillary area in the Matrigel implant containing both bFGF and kallistatin (HKBP) was significantly lower than that in the bFGF group (1903 ± 149 μm2/field versus 3645 ± 278 μm2/field, n = 6, P < .001; Figure 2B). Capillary formation was also determined by measuring hemoglobin levels in the Matrigel, which was directly proportional to the number of red blood cells. Figure 2C shows that hemoglobin levels in the HKBP plus bFGF group were significantly lower than those in the bFGF group (0.45 ± 0.06 g/dL versus 1.04 ± 0.17 g/dL, n = 5,P < .01). Similarly, the mean capillary area in the Matrigel implant containing both VEGF and kallistatin was significantly lower than that in the VEGF group (1571 ± 89 μm2/field versus 3157 ± 195 μm2/field, n = 6,P < .01; Figure 2D). Quantitative results of hemoglobin assay were consistent with morphologic analysis. The hemoglobin levels in the group containing both VEGF and kallistatin were significantly lower than those in the VEGF group (0.45 ± 0.03 g/dL versus 0.88 ± 0.08 g/dL, n = 5, P < .01; Figure 2E). These data indicate that kallistatin also suppresses VEGF-induced angiogenesis in a manner similar to bFGF in Matrigel implants in mice, although VEGF-mediated angiogenesis response was not as strong as bFGF.
Effect of kallistatin on VEGF- or bFGF-induced angiogenesis in Matrigel implants.
(A) Histologic analysis of implanted Matrigel plugs. Matrigel mixed without or with VEGF or bFGF (150 ng/mL) in the presence or absence of 2 μM kallistatin (HKBP) was injected subcutaneously into mice. The Matrigel plugs were stained with Masson trichrome at 1 week after injection. (B,D) Quantitation of mean capillary area in implanted Matrigel plugs. Each value represents mean area ± SEM (n = 6). (C,E) Hemoglobin levels in implanted Matrigel. Each value represents mean ± SEM (n = 5).
Effect of kallistatin on VEGF- or bFGF-induced angiogenesis in Matrigel implants.
(A) Histologic analysis of implanted Matrigel plugs. Matrigel mixed without or with VEGF or bFGF (150 ng/mL) in the presence or absence of 2 μM kallistatin (HKBP) was injected subcutaneously into mice. The Matrigel plugs were stained with Masson trichrome at 1 week after injection. (B,D) Quantitation of mean capillary area in implanted Matrigel plugs. Each value represents mean area ± SEM (n = 6). (C,E) Hemoglobin levels in implanted Matrigel. Each value represents mean ± SEM (n = 5).
Adenovirus-mediated kallistatin gene delivery suppresses spontaneous angiogenesis in the rat model of hind-limb ischemia
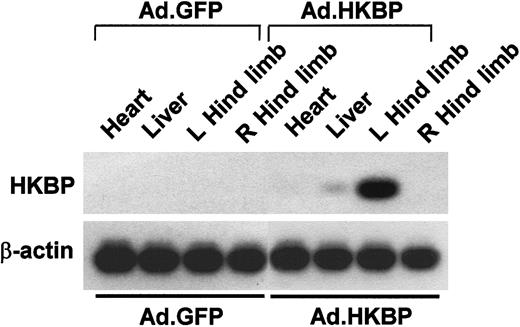
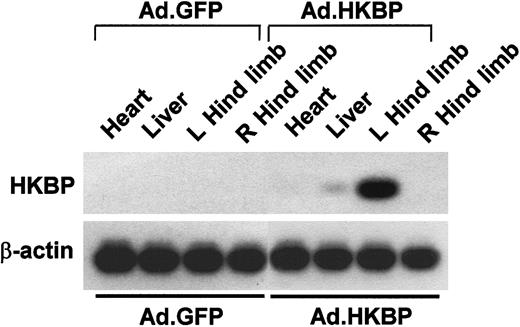
In this animal model, the femoral artery in the left hind limb was removed to create ischemia to induce spontaneous angiogenesis. Immediately after surgery, adenovirus harboring GFP cDNA or human kallistatin cDNA was locally injected into adductor muscles of the left hind limb at multiple sites. Expression of the human kallistatin mRNA in rats was examined using RT-PCR followed by Southern blot analysis. Figure 3 shows that human kallistatin mRNA was mainly identified in the left hind limb and barely detectable in the liver, but not in the right hind limb or heart of rats receiving local injection of Ad.HKBP. Human kallistatin mRNA could not be detected in the corresponding tissues of rats receiving Ad.GFP control virus. Identical levels of β-actin mRNA were detected in tissues of both control and experimental groups, verifying the quality of RNA in these samples. Following local injection of Ad.HKBP, expression of recombinant human kallistatin in the injected hind limb was further confirmed by ELISA. Immunoreactive human kallistatin levels in adductor muscles of the left hind limb at day 5 after human kallistatin gene delivery was 129.0 ± 31.9 ng/g tissue (n = 4), but not detected in animals receiving Ad.GFP control virus.
RT-PCR and Southern blot analysis of human kallistatin mRNAs in tissues at day 5 after gene delivery.
Adenovirus Ad.HKBP or control virus Ad.GFP was locally injected into left hind limb after surgery. Right hind limb did not receive any surgery and virus injection. Amount of loading samples was normalized by using the β-actin housekeeping gene.
RT-PCR and Southern blot analysis of human kallistatin mRNAs in tissues at day 5 after gene delivery.
Adenovirus Ad.HKBP or control virus Ad.GFP was locally injected into left hind limb after surgery. Right hind limb did not receive any surgery and virus injection. Amount of loading samples was normalized by using the β-actin housekeeping gene.
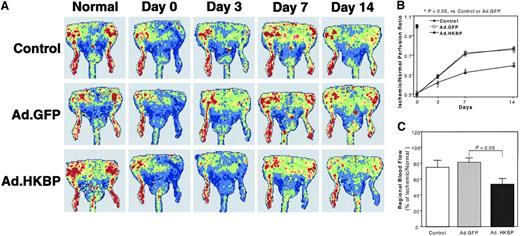
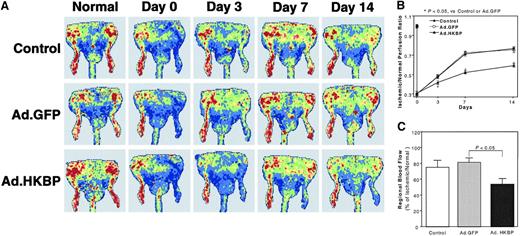
Blood perfusion recovery was monitored at days 3, 7, and 14 after surgery by laser Doppler perfusion imaging analysis. Representative laser Doppler images of one animal from each experimental group showed identical high perfusion in both hind limbs before surgery (Figure4A). Immediately after surgery, blood perfusion in left ischemic hind limbs was significantly reduced in all of the 3 groups. Due to spontaneous angiogenesis, high perfusion pattern was observed in both control groups at day 7 and day 14 after surgery. However, due to antiangiogenic effects of kallistatin, recovery of blood perfusion in the kallistatin group was persistently impaired as compared to 2 control groups. Perfusion was significantly lower in ischemic hind limbs of the Ad.HKBP group. Quantitative results of blood perfusion determined by laser Doppler perfusion imaging analysis (Figure 4B) based on all animals in 3 experimental groups (n = 8) are consistent with the imaging results.
Effects of kallistatin gene delivery on spontaneous angiogenesis in ischemic hind limbs.
(A) Representative laser Doppler images of hind-limb blood perfusion were measured before, right after, and at day 3, day 7, and day 14 after surgery. The perfusion signal is displayed as a different color. Dark blue means low perfusion or no perfusion, whereas red color means the highest perfusion. (B) Quantitative results of Doppler images were based on all of animals in 3 experimental groups. Each value represents mean ± SEM (n = 8). (C) Fluorescent microspheres assay was applied to determine the regional blood flow in hind limbs at 2 weeks after surgery. Each value represents mean ± SEM (n = 7).
Effects of kallistatin gene delivery on spontaneous angiogenesis in ischemic hind limbs.
(A) Representative laser Doppler images of hind-limb blood perfusion were measured before, right after, and at day 3, day 7, and day 14 after surgery. The perfusion signal is displayed as a different color. Dark blue means low perfusion or no perfusion, whereas red color means the highest perfusion. (B) Quantitative results of Doppler images were based on all of animals in 3 experimental groups. Each value represents mean ± SEM (n = 8). (C) Fluorescent microspheres assay was applied to determine the regional blood flow in hind limbs at 2 weeks after surgery. Each value represents mean ± SEM (n = 7).
Fluorescent microspheres assay was also used to determine the regional blood flow in both ischemic and control hind limbs at 2 weeks after surgery. Kallistatin gene delivery significantly inhibited spontaneous recovery of regional blood flow in ischemic hind limbs as compared to controls (Figure 4C). The percentage of fluorescence intensity in ischemic hind limbs to that in the contralateral nonischemic hind limbs in Ad.HKBP group was 54% ± 6% (n = 7, P < .05) as compared with 81%± 5% (n = 7) for Ad.GFP control group and 75% ± 8% (n = 8) for ischemic control group. The data are consistent with the laser Doppler perfusion image measurements. These results indicate that kallistatin gene delivery significantly inhibits spontaneous angiogenesis in ischemic hind limbs.
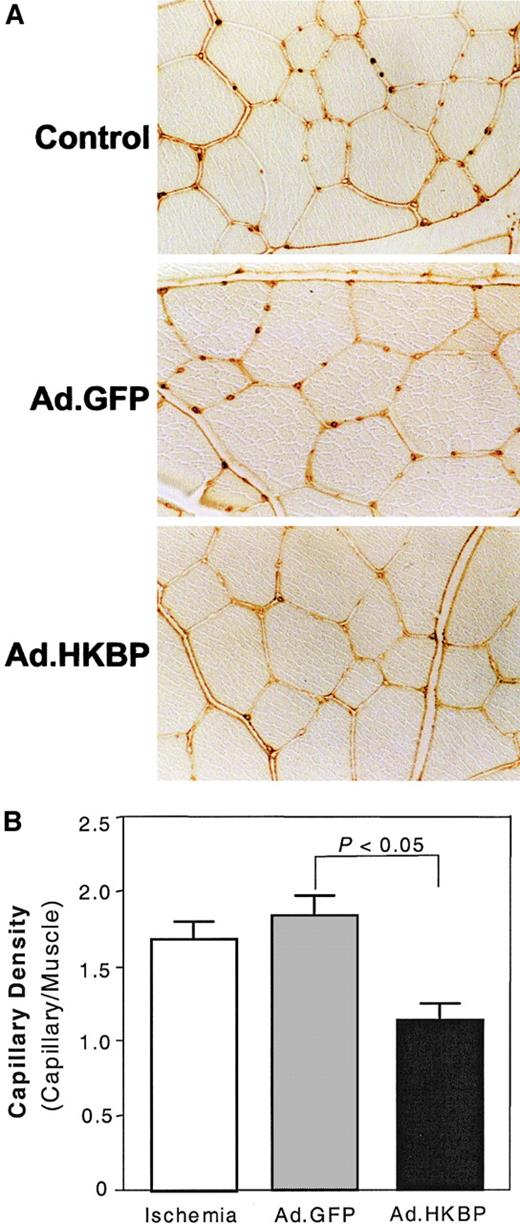
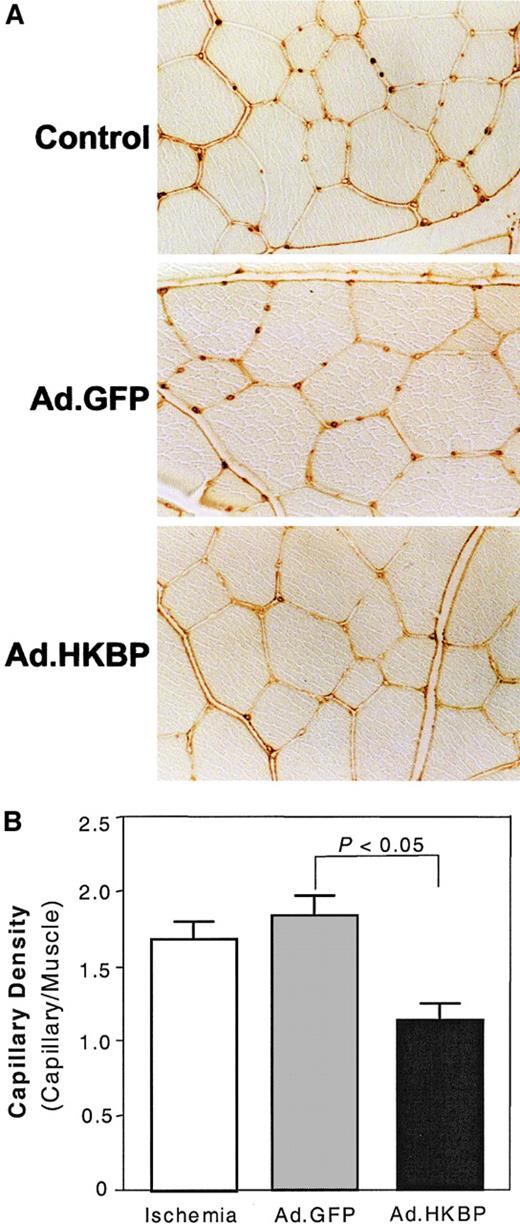
To elucidate whether the impairment of regional blood perfusion was due to the inhibition of spontaneous angiogenesis, capillary formation in ischemic muscles was examined by immunostaining with antibody to rat CD31. The representative histologic image (Figure5A) showed that capillary density in ischemic hind limbs receiving kallistatin gene delivery was significantly lower than control groups receiving PBS or control virus Ad.GFP. Quantitative results (Figure 5B) showed that capillary density in the Ad.HKBP group was 1.1 ± 0.1 capillary/muscle (n = 9,P < .01) versus 1.8 ± 0.2 (n = 5) and 1.7 ± 0.1 (n = 4) for the Ad.GFP control group and the ischemic control group, respectively. These results indicate that kallistatin gene delivery markedly impaired ischemia-induced capillary formation.
Effect of kallistatin gene delivery on capillary formation in rat ischemic hind limbs.
Adductor muscles were collected at 2 weeks after gene delivery for histologic analysis. (A) Representative histologic sections were stained with antibody against rat CD31. (B) Quantitative analysis of CD31 immunostaining. Each value represents mean ± SEM (n = 4-9).
Effect of kallistatin gene delivery on capillary formation in rat ischemic hind limbs.
Adductor muscles were collected at 2 weeks after gene delivery for histologic analysis. (A) Representative histologic sections were stained with antibody against rat CD31. (B) Quantitative analysis of CD31 immunostaining. Each value represents mean ± SEM (n = 4-9).
Adenovirus-mediated kallistatin gene delivery suppresses tumor growth and angiogenesis in human breast carcinoma xenografts of athymic mice
To further evaluate the effect of kallistatin on tumor growth, tumor xenografts were created by implanting MDA-MB-231 human breast carcinoma cells into the dorsa of athymic mice. Adenovirus carrying human kallistatin cDNA was intratumorly injected when tumors reached the size of 50 mm3. Immunoreactive human kallistatin levels in tumors receiving Ad.HKBP reached 155.4 ± 64.1 ng/mg protein (n = 4) and 89.0 ± 32.1 ng/mg protein (n = 3) at 1 week and 3 weeks after gene delivery, respectively, but remained undetectable in the control groups. Kallistatin gene delivery markedly inhibited tumor growth when compared to both PBS and Ad.GFP control groups (Figure6A). The average volume of breast tumors in Ad.HKBP-injected group at 3 weeks after gene delivery was 71 ± 9 mm3 (n = 16, P < .05) versus 189 ± 21 mm3 (n = 17) and 208 ± 34 mm3 (n = 16) for Ad.GFP- and PBS-injected groups, respectively.
Effects of kallistatin gene delivery on tumor growth.
(A) Kallistatin gene delivery inhibits tumor growth. MDA-MB-231 carcinoma cells were subcutaneously implanted into athymic mice. When the tumor had reached a volume of 50 mm3 (day 0), mice received an intratumoral injection of PBS (n = 16), 109pfu adenovirus carrying GFP cDNA (Ad.GFP, n = 17), or kallistatin cDNA (Ad.HKBP, n = 16). Each value represents mean ± SEM. (B) Kallistatin gene delivery inhibits tumor angiogenesis. Tumor tissues were collected at 3 weeks after gene delivery. Immunostaining with an anti–mouse CD31 monoclonal antibody demonstrated rarefication of small tumor blood vessels in kallistatin-treated tumors (Ad.HKBP) as compared with control tumors (Ad.GFP). (C) The number of CD31-stained blood vessels in 6 different microscopic fields from 3 different hot spots from each tumor section (8-11 tumors in each group) was evaluated. Each value represents mean ± SEM.
Effects of kallistatin gene delivery on tumor growth.
(A) Kallistatin gene delivery inhibits tumor growth. MDA-MB-231 carcinoma cells were subcutaneously implanted into athymic mice. When the tumor had reached a volume of 50 mm3 (day 0), mice received an intratumoral injection of PBS (n = 16), 109pfu adenovirus carrying GFP cDNA (Ad.GFP, n = 17), or kallistatin cDNA (Ad.HKBP, n = 16). Each value represents mean ± SEM. (B) Kallistatin gene delivery inhibits tumor angiogenesis. Tumor tissues were collected at 3 weeks after gene delivery. Immunostaining with an anti–mouse CD31 monoclonal antibody demonstrated rarefication of small tumor blood vessels in kallistatin-treated tumors (Ad.HKBP) as compared with control tumors (Ad.GFP). (C) The number of CD31-stained blood vessels in 6 different microscopic fields from 3 different hot spots from each tumor section (8-11 tumors in each group) was evaluated. Each value represents mean ± SEM.
The effects of kallistatin gene delivery on tumor angiogenesis were evaluated by CD31 immunostaining for capillaries in tumor tissues. The density of capillaries in the kallistatin-treated group was significantly lower than that in both control groups (Figure 6B) at 3 weeks after gene delivery. Microvessel density was assessed from CD31-stained tumor tissue sections. Microvessel density in tumors receiving Ad.HKBP reduced to 25% as compared with that in Ad.GFP-injected tumors and in PBS-injected tumors (25 ± 3 vessels/mm2, n = 10 versus 103 ± 12 vessels/mm2, n = 11 and 111 ± 12 vessels/mm2, n = 8, P < .01; Figure 6C). These results demonstrate that kallistatin gene delivery markedly suppressed the angiogenic response in tumor tissues.
Discussion
VEGF and bFGF are 2 major angiogenic stimulators.6Our results show that human kallistatin significantly inhibited both VEGF- and bFGF-induced proliferation, migration, and adhesion of primary cultured human endothelial cells in vitro, and attenuated VEGF- and bFGF-induced increases in capillary density and hemoglobin content in subcutaneously implanted Matrigel plugs in vivo. The inhibitory effect of kallistatin is not caused by a contaminant in the native kallistatin preparation because recombinant human kallistatin purified from an Escherichia coli expression system was also active. Our results showed that wild-type recombinant kallistatin, but not kallistatin mutant lacking heparin-binding activity, inhibited endothelial cell proliferation dose dependently (data not shown). These results indicate that kallistatin is a naturally occurring angiogenesis inhibitor that is capable of blocking vascular endothelial cells from responding to both VEGF and bFGF.
In this study, adenovirus-mediated kallistatin gene delivery significantly impaired the progressive recovery of blood perfusion in the ischemic hind limb as determined by laser Doppler perfusion imaging analysis. Ischemic hind limb is a well-established model of ischemia-induced spontaneous angiogenesis. In ischemic diseases, hypoxia is generally considered to be a fundamental stimulus for angiogenesis.33,34 The main mechanism of hypoxia-induced angiogenesis involves the induction of hypoxia-inducible factor-1α (HIF-1α) protein resulting in increased expression of VEGF, a specific angiogenic factor.35 To address the possible contribution of induced VEGF expression to spontaneous angiogenesis in ischemic tissues, serial examinations by laser Doppler perfusion imaging analysis disclosed that hind-limb blood flow was progressively augmented over the course of 14 days.36 Morphometric analysis of capillary density confirmed that the histologic sequence of neovascularization corresponded temporally to blood flow recovery detected in vivo.36 Impaired neovascularization after administration of a neutralizing VEGF antibody confirmed that ischemia-induced VEGF was the principal regulatory mediator of spontaneous neovascularization in ischemic tissues.36 This model has proved useful for studies designed to assess the impact of gene targeting on neovascularization of ischemic tissues.28,29,34 Moreover, it has been demonstrated that high incidence of autoamputation and limb necrosis occurs if blood perfusion recovery is less than 50%. Blood perfusion recovery of 70% to 80% in untreated ischemic hind limb normally results in residual ischemia, whereas exogenous angiogenesis stimulators can improve blood perfusion to 100% or more and result in limb salvage.37Consistent with these findings, we observed spontaneous blood flow recovery and neovascularization in both control and Ad.GFP groups. However, due to the inhibitory effect of kallistatin on angiogenesis, kallistatin gene delivery significantly inhibited ischemia-induced regional blood flow recovery and capillary formation as determined by fluorescent microsphere assay and CD31 immunostaining. Furthermore, impaired blood perfusion recovery resulted in atrophy of ischemic hind limb in the kallistatin-treated group. These results suggest that kallistatin is an effective inhibitor of ischemia-induced angiogenesis.
The invasiveness of breast carcinoma is angiogenesis-dependent. An iris angiogenic response was observed in 30% of fragments from biopsies of human hyperplastic lobules of the breast versus 65% of those from invasive breast carcinoma.38 Tumor angiogenesis correlated with metastasis in invasive breast carcinoma by examining histologic sections of human breast cancer stained with a specific marker for endothelial cells.39,40 In this study, we evaluated the effect of kallistatin gene delivery on tumor growth using human breast tumor xenografts in nude mice. The tumor xenograft created by implantation of MDA-MB-231 human breast carcinoma cells has been used widely to study the tumorigenicity of estrogen-receptor–negative human breast carcinoma cells in vivo.31 Tumor angiogenesis in the breast tumor xenografts was examined using CD31 immunostaining. Our results show that rarefaction of small blood vessels was found in kallistatin-treated tumor tissue sections as compared with the control, indicating a role of kallistatin in suppressing tumor angiogenesis. The inhibitory effect of kallistatin on tumor growth in vivo may be attributed to the inhibitory effect of kallistatin on tumor neovascularization because kallistatin did not have any effect on the proliferation and growth of MDA-MB-231 human breast carcinoma cells in vitro (data not shown). Previous studies showed that adenovirus-mediated gene delivery of angiostatin or endostatin inhibited tumor growth by about 70% at 3 weeks after gene delivery in tumor xenografts implanted with human breast tumor cell line (MDA-MB-231) or a murine breast cancer cell line (JC).41,42 Kallistatin gene delivery thus compared favorably with angiostatin and endostatin in its ability to inhibit tumor growth in vivo. In addition, tissue kallikrein is highly expressed in adenocarcinomas43 and can efficiently activate 2 matrix-degrading metalloproteinases, progelatinase (MMP-2) and procollagenase (MMP-9).44,45 Like plasmin, tissue kallikrein may have a role in degrading extracellular matrix to promote tumor invasion. In support of this notion, a recent study has shown that a specific peptide-based tissue kallikrein inhibitor attenuated the invasiveness of human breast tumor cells.46 Similarly, recombinant wild-type kallistatin, a specific tissue kallikrein inhibitor, significantly inhibited the invasiveness of human breast tumor cell lines (data not shown). However, a recombinant kallistatin mutant lacking inhibitory activity toward tissue kallikrein had no effect on tumor cell invasion. These results suggest that unlike angiostatin or endostatin, kallistatin may inhibit tumor invasion by 2 distinct and complementary mechanisms.
The concentrations of kallistatin used in in vitro studies seem higher than the expression levels of recombinant kallistatin detected in tissues. There are 2 possible explanations for this difference. First, recombinant kallistatin levels detected are average levels in adductor muscles or in tumor tissues, not in situ expression levels in the area of angiogenesis. Therefore, local expression levels of recombinant kallistatin could be higher than the detected levels. Second, multiple forms of serpins have been identified: native inhibitory, inactivated, or latent forms, and noninhibitory forms such as cleaved, polymerized, and oxidized. Conformationally modified serpins have other biologic activities in addition to their role as proteinase inhibitors.47 For example, it has recently been shown that antithrombin, which functions as an inhibitor of thrombin and other enzymes, in its cleaved conformation has potent antiangiogenic and antitumor activity in a mouse model. Cleaved form of antithrombin, which is produced by incubation with human pancreatic cancer cells or human neutrophil elastase, has at least 100-fold increase in inhibitory effect on angiogenesis as compared to its native form.9Kallistatin may also have multiple forms with different reactivity. Whether tumor cells or ischemic tissues can produce a cleaved form of kallistatin with more potent antiangiogenic activity remains to be investigated.
Both VEGF and bFGF are heparin-binding growth factors, and binding of VEGF and bFGF to heparan-sulfate proteoglycans on endothelial cell surfaces can modulate the binding of VEGF and bFGF to their specific receptors.48,49 Kallistatin is also a heparin-binding protein.21 The major heparin-binding domain was identified in the region between the H helix and C2 sheet of kallistatin that contains clusters of positively charged residues.50Site-directed mutagenesis of the basic residues within this domain resulted in a loss of specific heparin-binding capacity.50Kallistatin may act by competing with VEGF and bFGF binding to heparan-sulfate proteoglycans, a low affinity-binding site, and thus suppressing VEGF- and bFGF-binding activity and the angiogenesis signaling cascades induced by VEGF and bFGF. In our preliminary study, we showed that recombinant wild-type kallistatin competed with the specific binding of 125I-labeled VEGF to HMVECs. However, kallistatin mutant, lacking heparin-binding activity, did not interfere with VEGF binding to these cells (data not shown). These results suggest that kallistatin interferes with VEGF binding at the heparin-binding site and the heparin-binding domain in kallistatin may play an important role in the inhibition of angiogenesis. This action of kallistatin is similar to that of endostatin because the inhibitory effect of endostatin on bFGF-induced angiogenesis is mediated by its heparin-binding activity.51 52 Recent trial failure of SU5416, an angiogenesis inhibitor targeting VEGF receptor, results in revisiting the strategy applied in the inhibition of angiogenesis and further exploring more broad-acting drugs. In this regard, kallistatin might fulfill the role as a broad-spectrum inhibitor. It is capable of inhibiting VEGF and bFGF-mediated angiogenesis as well as preventing the activation of metalloproteinases by inhibiting tissue kallikrein activity.
In conclusion, kallistatin markedly inhibits angiogenesis by suppressing VEGF- and bFGF-induced proliferation, migration, and adhesion of endothelial cells. This is the first study to demonstrate that kallistatin is an inhibitor of angiogenesis and tumor growth. This study provides new insights into the biologic function of kallistatin as an angiogenesis inhibitor.
Prepublished online as Blood First Edition Paper, July 5, 2002; DOI 10.1182/blood-2002-01-0185.
Supported by the National Institutes of Health grant HL 44083.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Julie Chao, Department of Biochemistry and Molecular Biology, Medical University of South Carolina, Charleston, SC 29425; e-mail: chaoj@musc.edu.

![Fig. 1. Effects of kallistatin on VEGF- and bFGF-induced proliferation, migration, and adhesion of HMVECs. / (A,B) Quiescent HMVECs were incubated with the indicated concentrations of human kallistatin (HKBP) and VEGF or bFGF (15 ng/mL) for 24 hours. DNA synthesis was measured as [3H]-thymidine incorporation. Each value represents mean ± SEM (n = 4). (C) Cell migration was determined using modified Boyden chambers. VEGF or bFGF, 15ng/mL; HKBP, 1μM. Each value represents mean ± SEM (n = 3). (D) Cell adhesion was determined using fibronectin-coated plates. VEGF or bFGF, 15 ng/mL; HKBP, 1μM. Each value represents mean ± SEM (n = 4).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/100/9/10.1182_blood-2002-01-0185/4/m_h82123311001.jpeg?Expires=1766078248&Signature=N1Fo3ou85QOSnpPxDZ8sykT~omBfyW5ztZaewSwZrUGDj6mo4zOqcOphLVHmby5F7pLMNfLlQqgYo1HyXkJHv2ZIT4eoV2DhJMaMUUFttniXNDkAnMgm-DQEnWpwPdhiUvZ7CwrzYG2rV4dnG2y7KikiI8Hq5BZ8uXNhy~hBevGZFC6FfAPx2ziZ0GnlB1fLv3cR2DgekLbSDx93Gm88KZkqtkgOiCQ9uG9SqeKaBX32rKy-EK0TNehIqZzVSPy8DU4IwobQTsi3jpbVxZsECTqpp0GZNw7Fv-mW0TiRsMAxdSTxxkdDJcZCODZ4M~lfEFVA9ahU6rHXOkY9o1cq3A__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)



![Fig. 1. Effects of kallistatin on VEGF- and bFGF-induced proliferation, migration, and adhesion of HMVECs. / (A,B) Quiescent HMVECs were incubated with the indicated concentrations of human kallistatin (HKBP) and VEGF or bFGF (15 ng/mL) for 24 hours. DNA synthesis was measured as [3H]-thymidine incorporation. Each value represents mean ± SEM (n = 4). (C) Cell migration was determined using modified Boyden chambers. VEGF or bFGF, 15ng/mL; HKBP, 1μM. Each value represents mean ± SEM (n = 3). (D) Cell adhesion was determined using fibronectin-coated plates. VEGF or bFGF, 15 ng/mL; HKBP, 1μM. Each value represents mean ± SEM (n = 4).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/100/9/10.1182_blood-2002-01-0185/4/m_h82123311001.jpeg?Expires=1766078249&Signature=KKUtmN3ktLJXdYWs6oT7VWOgEv5dG5ZYckAyapKxdtjtNf5XzeRSp3zJ8qtlppXfUK0l19VpT1zawW0~J03LCrloU2cpY8oTBncRJpeVzrb-OQu5f6JX8luaaRKWCJYWgyQlrs2zkpsRX12wXijnDfRSYa3J7mfh6EVwnYFKOiPVa-ZyKj-KG4uiOVV5fPwl3j5JkSCxYdhXxmWEUIR8BSsUf-Rzc8YP5aGB9ezpN1Gyg7-1X-9nfwL3I1kaISmop0TU8LDwN6W6-4erv6B~mjw7mcBp1-7KYlq8SecLprKkpneomyTQLN7Mod6d28zuy9lbT9ZQUW6itwnnz7NN4A__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)