Intravenous immunoglobulins (IVIGs) are widely used in the supportive therapy of immunodeficient patients and in the treatment of a wide variety of chronic autoimmune and inflammatory diseases.1,2 The proposed mechanisms of action of IVIG in these diseases include the inhibition of phagocytosis and immunomodulatory effects. Inhibition of phagocytosis has been observed in diseases such as immune thrombocytopenia purpura (ITP), in which platelets opsonized by the pathogenic autoantibodies are no longer phagocytosed shortly after IVIG infusion.3 Several mechanisms of inhibition of phagocytosis by IVIG have been proposed and include the direct competitive blockade of the Fc receptors I and III (FcRI and III)4,5 and the interaction with the inhibitory FcRIIB.6 However, the nature and origin of the immune complexes (ICs) that can interact with FcRs have remained unclear. Previous work has focused on the presence of IgG aggregates in IVIG that could be formed during the manufacturing process7 or through anti-idiotypic interactions.8 9
Healthy individuals continuously produce self-reactive IgM and IgG. The production and reactivity of serum IgG autoantibodies are tightly regulated in order to avoid formation of immune complexes, which could result in inflammation.10 It has been shown that the reactivity of autoreactive IgG was constantly inhibited by id–anti-id interactions with IgM and IgG antibodies.10 11IVIG preparations contain mostly IgG (> 98%), with only trace amounts of IgM, IgA, and other plasma proteins. In the present work, we have tested the possibility that the injection of large amounts of IVIG could oversaturate the normal mechanisms of control of autoreactive IgG present in human plasma and result in the formation of soluble autoimmune complexes (auto-ICs).
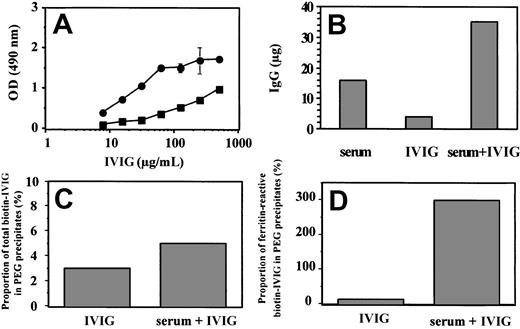
It is known that purified IgGs are much more polyreactive than serum IgGs,12 and we confirmed this observation with human ferritin. IVIGs reacted strongly with ferritin in enzyme-linked immunosorbent assay (ELISA), while serum exhibited a very low antiferritin reactivity at 25 μg/mL of IgGs (OD < 0.1; data not shown). Using this differential reactivity, we determined the ability of a fixed volume of human serum to inhibit the reactivity of increasing concentrations of IVIG. As shown in Figure1A, optical density (OD) results indicated that the addition of a fixed amount of serum resulted in a significant reduction of the IVIG antiferritin reactivity. The inhibition was high (> 75%) up to a dose of about 50 μg/mL of IVIG and then gradually decreased. These results indicated that the ability of serum to inhibit the autoreactivity of exogenously added IgG is saturable. The amount of serum IgG can be increased by a factor of about 3 (25 μg/mL of endogenous IgG and 50 μg/mL of exogenous IgG) before a significant in vitro autoreactivity of the serum-IVIG blend can be detected. Similar IgG increases can be observed in the plasma of IVIG-treated patients, since it has been estimated that the infusion of 100 mg/kg of IVIG increases the IgG plasma level by 2.5 mg/mL.13
Analysis by ELISA of the ferritin reactivity and IgG content of various fractions.
(A) Antiferritin reactivity of IVIG in presence of human serum. Reactivity was measured in ELISA in presence (▧) or absence (●) of a fixed volume of human serum corresponding to a final IgG concentration of 25 μg/mL. (B) Amount of total IgG in PEG precipitates. Quantification of IgG was done by ELISA. (C) Proportion of total biotin-labeled IVIG in PEG precipitates. Biotin-IgG was quantified by ELISA using streptavidin-HRP conjugate and the starting biotin-IVIG solution as standard. (D) Proportion of ferritin-reactive biotin-IVIG in the PEG precipitates. Ferritin reactivity of serial dilutions of the PEG-precipitated fractions was measured by ELISA and detected using a streptavidin-HRP conjugate. One unit of ferritin reactivity was defined as the volume of each fraction, which produced an OD of 0.4.
Analysis by ELISA of the ferritin reactivity and IgG content of various fractions.
(A) Antiferritin reactivity of IVIG in presence of human serum. Reactivity was measured in ELISA in presence (▧) or absence (●) of a fixed volume of human serum corresponding to a final IgG concentration of 25 μg/mL. (B) Amount of total IgG in PEG precipitates. Quantification of IgG was done by ELISA. (C) Proportion of total biotin-labeled IVIG in PEG precipitates. Biotin-IgG was quantified by ELISA using streptavidin-HRP conjugate and the starting biotin-IVIG solution as standard. (D) Proportion of ferritin-reactive biotin-IVIG in the PEG precipitates. Ferritin reactivity of serial dilutions of the PEG-precipitated fractions was measured by ELISA and detected using a streptavidin-HRP conjugate. One unit of ferritin reactivity was defined as the volume of each fraction, which produced an OD of 0.4.
The above findings and the observation that IVIG reacted with multiple plasma proteins in Western blot experiments (data not shown) suggested the formation of auto-ICs in serum in the presence of IVIG. This possibility was tested directly by precipitating the IC in the presence of 2.5% polyethylene glycol (PEG).14 The results of a representative experiment (Figure 1B) showed that the amount of PEG-precipitated IgG in the serum-IVIG blend was significantly higher than the sum of precipitated IgG obtained with the 2 isolated fractions. To determine if the added IVIG contributed to this synergistic effect, the experiment was repeated with biotin-labeled IVIGs, which were specifically detected using a streptavidin–horseradish peroxidase (HRP) conjugate. The result (Figure 1C) confirmed the involvement of IVIG, since 60% more biotin-labeled IVIGs were present in the PEG precipitate of the serum-IVIG blend compared to the PEG precipitate of IVIG alone. To determine if autoantibodies were involved, the precipitated ICs were tested for ferritin reactivity, which was also detected with a streptavidin-HRP conjugate. The PEG precipitate of IVIG contained about 10% of the initial ferritin reactivity. But the PEG precipitate of the serum-IVIG blend contained almost 3 times more ferritin-reactive antibodies than the starting blend. This unexpected result indicated first that ferritin-reactive autoantibodies are found mostly in the IC fraction. The higher ferritin reactivity of the isolated IC is reminiscent of the higher polyreactivity of purified IgG compared to serum,12 and suggested that the ferritin reactivity of the soluble IC is inhibited by undefined serum components, which are not precipitated by PEG.
The results support the hypothesis that therapeutic doses of IVIG can oversaturate the normal mechanisms of inhibition of natural autoantibodies and result in the formation of soluble IC. Soluble plasma ICs have been observed in a number of autoimmune diseases,15 but the possible formation of soluble IC containing IVIG and normal plasma proteins has not been specifically studied so far. It is possible that these ICs are rapidly cleared from the circulation after interaction with FcR-bearing cells, thus making them difficult to detect in the plasma of IVIG-treated patients. However, there is evidence that auto-IC may be involved in the therapeutic effects of IVIG in some diseases. The reactive macrophage activation syndromes are characterized by a massive increase in plasma ferritin levels.16 It was recently reported that the successful treatment of this disease by injection of large doses of IVIG was associated with immune clearance of ferritin, which could be detected in plasma IC one day after IVIG injection.16Further characterization of the IC formed in human serum following IVIG addition is under way in our laboratory and will permit better definition of their composition and biological activity. The work may permit the defining of ways to purify the IgG responsible for the formation of IC starting from currently used IVIG preparations. Such a procedure could result in the preparation of different subpreparations of IVIG for use in different diseases, and may thus permit treatment of more patients with the available amounts of IVIG.
For precipitation of IC, PEG 6000 (Sigma, Oakville, ON, Canada) was added to a final concentration of 2.5% to the diluted IVIG and serum solutions containing about 5 mg/mL of IgG as described previously.14 After overnight incubation at 4°C, precipitates were collected by centrifugation at 1500g for 20 minutes, washed twice in 2.5% PEG, and dissolved by incubation for 30 minutes at 37°C in phosphate buffered saline (PBS) containing 0.05% Tween 20, 10 mM EDTA (ethylenediaminetetraacetic acid), and 0.01% thimerosal.
For ELISA, microplate wells were coated with human ferritin (Calbiochem, La Jolla, CA) or anti–human IgG (Fc-specific; Jackson ImmunoResearch Laboratories, West Grove, PA) in 100 mM carbonate buffer, pH 9.7. After overnight incubation at 4°C, wells were blocked with 5% bovine serum albumin (BSA) in 0.05% Tween 20–PBS for one hour at 37°C. After washing with 0.85% NaCl, samples diluted in 1% BSA-0.05% Tween 20–PBS were distributed into triplicate wells, and the plate was incubated for 1 hour at 37°C. After washing, bound antibodies were detected with peroxidase-labeled goat anti–human IgG (Fc specific; Jackson ImmunoResearch Laboratories; Figure 1A-B) or peroxidase-labeled streptavidin (Jackson ImmunoResearch Laboratories; Figure 1C-D) and revealed with the ortho-phenylenediamine (OPD) substrate (Abbott Laboratories; Abbott Park, IL). Optical densities were read at 490 nm with a reference at 630 nm.