Gene therapy for the β-globin disorders β-thalassemia (β-thal) and sickle cell disease (SCD) is now a fast-moving field. The momentum was generated in 2000 when May et al demonstrated that in contrast to oncoretroviral vectors, lentivirus vectors containing human globin genes and regulatory regions from the β-globin locus control region could be faithfully transduced into mouse hematopoietic stem cells and expressed in erythroid cells.1 Subsequent studies demonstrated that globin lentivirus vectors could produce therapeutic levels of β-like globin, allowing the successful treatment of mouse models of β-thal intermedia2,3 and β-thal major4 by gene therapy. In the wake of the original result, Pawliuk et al developed a lentivirus containing a modified human β-globin gene and showed that this vector could produce enough of the transgenic β-globin protein to suppress erythrocyte sickling and improve the pathology of 2 mouse models of SCD.5
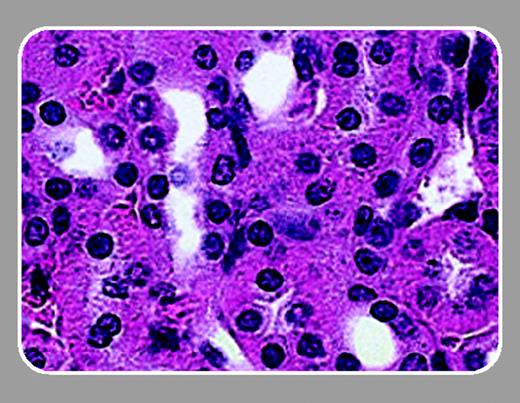
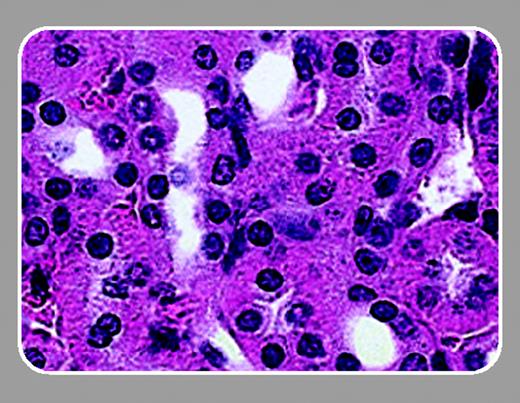
In this issue of Blood, Lavasseur and colleagues (page 4312) have followed up on the original description of successful correction of SCD in the mouse model. Similar to Pawliuk et al,5 Lavasseur et al demonstrate that lentivirus-mediated gene transfer of a modified human β-globin gene could inhibit the sickling of mouse SCD erythrocytes. In addition, they describe significant improvements in all clinical parameters measured, including liver and spleen necrosis and kidney function.
Lavasseur et al make 3 important points that should interest the readers of Blood. First, they have refined both the mouse model and the lentivirus vector. This group has developed an inbred SCD mouse model that allows transplantations to be done without the complications of graft-versus-host disease. In addition, Lavasseur et al used inbred SCD mice as both donors and recipients, ensuring that there were no normal mouse erythrocytes in the circulation. Thus, the improvements seen in the animals were the direct result of the globin transgene. Lavasseur et al also engineered the human β-globin gene to produce more potent antisickling activity and a greater affinity for α-globin.
Second, Lavasseur et al provide direct evidence of the number of erythroid cells that are expressing the transgene. Using a single-cell polymerase chain reaction (PCR), they showed that up to 85% of the reticulocytes were producing transgene mRNA at levels that correlated with the level of β-globin protein in erythrocytes. Lavasseur et al calculated that each vector copy generated approximately 20 g hemoglobin/L (2 g/dL).
Finally, Lavasseur et al have addressed issues about the safety of gene therapy raised by the French X-linked severe combined immune deficiency trial in which 2 of 11 patients developed a T-cell leukemia associated with oncoretrovirus insertion. The self-inactivating lentivirus vector developed by Lavasseur et al prevents the lentivirus long-terminal repeat sequences from functioning as either a promoter or an enhancer for any nearby gene. In addition, Lavasseur et al transduced and transplanted only 1000 highly enriched hematopoietic stem cells, minimizing the number of lentiviral integrations.
The application of this technology to the treatment of human SCD is coming closer, but several important questions need to be addressed. The minimum percentage of corrected cells needed to successfully treat SCD must be determined, since it is unlikely that complete bone marrow ablation would be well tolerated by patients with SCD. Also, most SCD mice have β-thal in addition to SCD. It must be determined exactly how much of the clinical improvement is due to the suppression of sickling and how much is due to the normalization of globin chain levels. The inbred SCD mouse model is ideal for all of these studies. It appears that the talented workers in this field will rapidly address these problems and continue the progress toward gene therapy for SCD.