Chronic myelogenous leukemia (CML) is a malignant disease of hematopoietic stem cells that develops in a biphasic or triphasic course. The initial chronic phase (CML-CP) is characterized by massive expansion of granulocytic cell series. Although immature myeloid cells appear in the peripheral blood in this phase, the CML progenitor cells retain the ability to terminally differentiate. Progression of the disease after 3 to 5 years to fatal blast phase (CML-BP) is characterized by the accumulation of myeloid or lymphoid blast cells. The BCR/ABL fusion gene, a product of the t(9;22)(q34;q11) translocation found in the vast majority of human CMLs, plays an essential role in initiation as well as maintenance and progression of the disease. BCR/ABL has been found to activate many signaling pathways, including Ras, phosphatidylinositol 3-kinase, signal transducers and activators of transcription (STATs), c-Myc, and Bcl-2 or Bcl-XL, that regulate cell growth, survival, and adhesion/migration. Despite the strong mitotic activity of BCR/ABL, both clinical and laboratory studies demonstrate that BCR/ABL is not sufficient to block the terminal differentiation of myeloid cells in vivo. This indicates that the cell-autonomous developmental/differentiation program can override BCR/ABL's mitotic signal. Blocking cell differentiation seen in CML-BP is likely caused by cooperation of BCR/ABL and additional genetic abnormalities acquired during disease development.1
Interferon consensus sequence binding protein (ICSBP)/IRF-8 is a hematopoietic-specific transcription factor belonging to the interferon (IFN) regulatory factor (IRF) family. It plays an important role in regulating immune responses and hematopoiesis. ICSBP-deficient mice exhibit enhanced susceptibility to viral and intracellular parasite infections, possibly due to impaired interleukin-12 (IL-12) production. Interestingly, ICSBP-deficient mice also manifest a CML-like syndrome.2 Consistent with the latter ICSBP-null phenotype, it was shown recently that ICSBP controls myeloid cell development by stimulating macrophage differentiation while inhibiting granulocyte differentiation, in both cases inhibiting cell growth.3 In addition, ISCBP was shown to facilitate apoptosis.
The negative regulatory function of ICSBP on cell growth and survival seems to play a role in the pathogenesis of CML. It was found that ICSBP transcripts were decreased in patients with CML and that this reduction of ICSBP transcripts could be reversed by IFN-α treatment.4 In addition, experiments using a mouse model showed that ICSBP was downregulated in BCR/ABL-induced murine CML-like disease and that forced coexpression of ICSBP inhibited the BCR/ABL-induced myeloproliferative disorder.5 However, the precise mechanism by which ICSBP suppresses CML is not known.
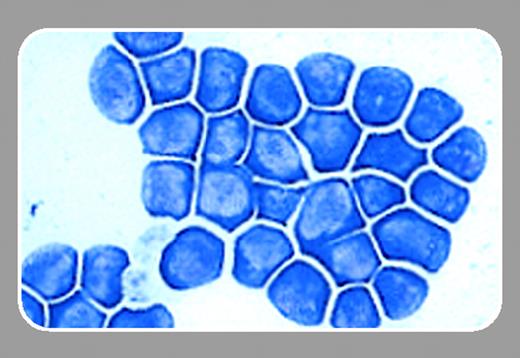
In this issue, Tamura and colleagues (page 4547) report that ICSBP modulates the growth-promoting activity of BCR/ABL in a previously established granulocyte-macrophage colony-stimulating factor (GM-CSF)-dependent ICSBP-/- myeloid progenitor cell line, Tot2. As in several other cytokine-dependent hematopoietic cell lines, expression of BCR/ABL renders Tot2 cells growth factor-independent. Interestingly, when ICSBP was ectopically expressed, like the parental Tot2 cells, BCR/ABL-transformed cells underwent complete growth arrest and differentiated into mature macrophages. These results suggest that ICSBP, either directly or through the differentiation program it induces, overrides the BCR/ABL mitotic signal.
In searching for the molecular basis for ICSBP-induced growth arrest and differentiation of BCR/ABL-expressing Tot2 cells, Tamura and coworkers found that ICSBP repressed c-Myc expression through direct induction of the expression of c-Myc re-pressors, B lymphocyte-induced maturation protein-1 (Blimp-1) and mitogenic ETS transcriptional suppressor/PUETS-related (METS/PE1). Both Blimp-1 and METS/PE1 have been shown to play critical roles in macrophage differentiation, whereas c-Myc overexpression was found to be important for BCR/ABL transformation. Thus, the study by Tamura and coworkers provides a mechanistic basis for ICSBP-induced macrophage differentiation and for ICSBP's potential to antagonize the leukemogenic activity of BCR/ABL. Further study is needed to determine whether ICSBP, when it is induced or ectopically expressed, suppresses BCR/ABL-positive myeloproliferative disorder through a similar mechanism.