Molecular therapy of chronic myeloid leukemia (CML) since the advent of imatinib mesylate (Glivec, Gleevec) is a developing paradigm for oncology in general and for hematologic malignancies in particular. Our understanding of the basic biology of the disease, and the availability of high-throughput drug screens, arms us with small-molecule drugs that inhibit the key steps in the genesis, maintenance, and proliferation of the tumor. However, imatinib, at the vanguard, has shown that responses to single specific inhibitors alone may be short-lived and relapse is most often associated with a loss of drug binding caused by the exquisitely powerful selection of random cells carrying mutations in the Bcr-Abl tyrosine kinase domain that render them resistant to imatinib. Even as it becomes increasingly likely that imatinib does confer long-term benefit in the treatment of CML, the addition of other drugs will have an important role in improving clinical responses to imatinib used as a single agent or in managing resistance to this drug.FIG1
In addition to Bcr-Abl, other downstream proteins essential for transducing the oncogenic signal are good candidates for targeted therapy. For example, a key player is the oncoprotein Ras, known to be active only when tethered to the cytoplasmic membrane. This attachment depends on a spe cific posttranslational modification (called prenylation, usually of the farnesylation type) of Ras, although the exact mechanism underlying this location-dependent activity, and the cast of other proteins that behave similarly, is only partly understood. An important observation is that mutagenesis of one specific cysteine residue in oncogenic Ras, whereby farnesylation and localization to the cell membrane cannot occur, prevents transformation of fibroblasts via loss of Ras/MAPK (mitogen-activated protein kinase) signaling.1 Therefore, Ras signaling might represent an excellent target for intervention in many areas of oncology.
At present, clinical trials of inhibitors of the farnesyl transferases (known as FTIs) in CML are underway, and the in vitro data for these drugs are encouraging, even where responses to imatinib are poor.2 However, it appears that when Ras farnesylation is prevented, other lipid modifications such as geranylgeranylation may be possible, leading to restoration of Ras/MAPK signaling and the loss of the therapeutic effect.
In this issue, Kuroda and colleagues (page 2229) present in vitro and in vivo data describing the cytotoxic effects on CML cells of the third-generation bisphosphonate zoledronic acid (ZOL). ZOL is known to prevent both farnesylation and geranylgeranylation of Ras-related proteins and is thus potentially more efficient than conventional FTIs. Kuroda et al found that ZOL selectively inhibits the growth of CML cells in vitro and in vivo, at least partly via the induction of apoptosis, and is not ef fluxed by the P-glycoprotein pump. ZOL also combines well with imatinib exhibiting clear in vitro synergistic effects, a highly desirable interaction. Using a murine transplantation model, the authors showed that ZOL, like imatinib, prolongs survival of mice via the selective killing of the transplanted human leukemic cells, and this effect was even more significant when ZOL was combined with imatinib. A phase 1 clinical trial of ZOL has defined well-tolerated doses that are of the same relative magnitude as those used in the murine study. Perhaps most intriguingly, ZOL is known to rapidly localize to bone, raising the desirable prospect of a high local concentration and level of effect in the bone marrow, although this may reduce the effi-cacy against circulating leukemic cells.
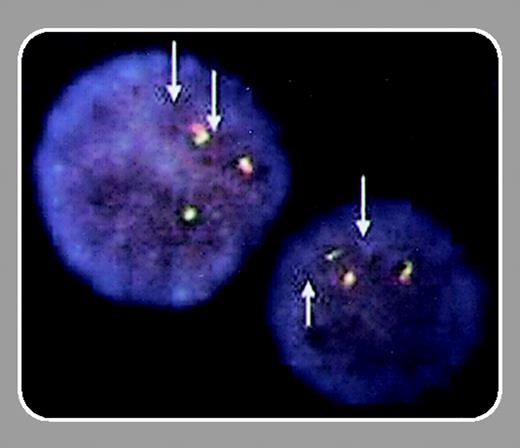
The possible addition of ZOL to the armamentarium of drugs that can be effective against CML is a significant step forward. Many questions remain unanswered, however: Are the antiproliferative and proapoptotic effects of ZOL due solely to inhibition of Ras localization to the cell membrane or are other prenylated proteins also involved? Will the preferential concentration of ZOL in the bone marrow encourage proliferation of leukemic cells in ZOL-free extramedullary “sanctuaries”? And will ZOL be effective for killing imatinib-resistant CML cells? As previously shown for Bcr-Abl,3,4 the localization of a protein to the “correct” cellular compartment makes a world of difference to signal transduction and leukemogenesis...