Abstract
CC chemokine ligand 2 (CCL2) is constitutively expressed at high levels in human peripheral blood monocytes, and its expression is further up-modulated during their differentiation into macrophages as well as in the course of HIV infection. To investigate the role of endogenous CCL2 on HIV replication and macrophage function, CCL2's activity was neutralized by specific antibodies. Infection of monocyte-derived macrophages with laboratory-adapted HIV-1 or primary viral isolates in the continuous presence of anti-CCL2 antibody resulted in significantly lower p24 Gag antigen release with respect to control cultures. Interestingly, CCL2 neutralization did not affect the early steps of the HIV life cycle but resulted in the intracellular accumulation of p24 Gag antigen. Simultaneously, remarkable changes in cell morphology and size occurred in cell cultures maintained in the presence of anti-CCL2 antibody. These results suggest that CCL2 may represent an autocrine factor important for enhancing virion production likely by affecting the macrophage cytoskeleton. (Blood. 2003;102:2334-2337)
Introduction
Blood monocytes and resident macrophages are important in vivo cell targets of HIV infection, and their role in AIDS pathogenesis is well documented.1 They usually survive HIV infection, serve as a major virus reservoir, and function as immunoregulatory cells through secretion of several proinflammatory cytokines and chemokines in response to HIV infection and to its proteins, thereby recruiting and activating new target cells for the virus, including CD4+ T cells.2-4 Thus, it is important to define those cellular factors and mechanisms involved in the regulation of the virus life cycle in these cells.
CC chemokine ligand 2 (CCL2; formerly monocyte chemotactic protein-1, MCP-1) is a CC chemokine produced by many cell types in response to different signals.5 Peripheral blood monocytes spontaneously secrete CCL2 and its expression is up-regulated during their differentiation into macrophages6,7 and as a consequence of HIV infection, in vitro8 and in vivo.9 Although originally described as a monocyte chemoattractant,10 many activities have been subsequently assigned to CCL2, including modulation of HIV-1 infection.11-15 However, CCL2's mechanism of action remains undefined and no studies have been carried out to evaluate the potential role of endogenous CCL2 in the control of HIV-1 infection in primary human macrophages. In this study, we report that CCL2 acts as an enhancing factor for HIV-1 spreading in monocyte-derived macrophages (MDMs) since its neutralization by specific antibodies (Abs) leads to a marked down-regulation of HIV-1 production. CCL2 does not affect early events in the HIV-1 life cycle, but modulates later steps involved in assembly, maturation, and/or release of new progeny virions, likely by affecting cytoskeleton organization.
Study design
MDM preparation and HIV-1 infection
Primary MDMs were prepared as previously described6 and then infected with 300 tissue culture infective dose (TCID50)/106 cells of CC chemokine receptor 5 (CCR5)-dependent (R5) HIV-1BaL strain or with primary isolates, as specified further. After 2 hours of incubation at 37°C, cells were washed and cultured in complete medium. Culture medium was replaced with fresh medium containing anti-CCL2 Ab twice a week. Aliquots of culture supernatants and cell pellets were harvested at different time points and stored at -80°C.
Reagents
Polyclonal and monoclonal Abs directed against CCL2 and characterized for neutralizing activity, as well as the isotype-matched control Abs, were purchased from PeproTech (London, United Kingdom). There have been 2 different polyclonal Abs against CCL2 used. Both of them were produced in rabbits using highly purified recombinant human CCL2, although they were purified by different procedures.
Measurement of CCL2 content
The levels of CCL2 present in culture supernatants were measured by enzyme-linked immunosorbent assay (ELISA) as previously reported.6
Determination of HIV-1 replication
Viral production was monitored by HIV-1 p24 Gag antigen (Ag) release by an ELISA kit (NEN Life Science Products, Zaventem, Belgium), with a detection range between 12.5 and 100 pg/mL. In some experiments, the cell-associated content of HIV-1 p24 Gag Ag was measured after cell disruption by 3 repeated cycles of freezing/thawing.
Confocal laser-scanning microscopy (CLSM) analysis
For CLSM analysis, MDMs were seeded in 24-well cluster plates on cover glasses (diameter, 12 mm). At the indicated time points, cells were washed with phosphate-buffered saline (PBS), fixed, permeated, and stained as previously described.16
Statistical analysis
Statistical analysis was performed by the nonparametric Kruskall-Wallis test. P values less than .05 were considered significant.
Results and discussion
To investigate the role of endogenous CCL2 in macrophage susceptibility to HIV infection, MDMs were infected with the R5 HIV-1BaL in the presence/absence of a polyclonal anti-CCL2 Ab and the kinetics of viral replication extent were monitored at different times after infection. As shown in Figure 1A, a significant reduction of HIV-1 p24 Gag Ag release, maximal at the peak of viral replication, was observed in infected cultures in the presence of anti-CCL2 Ab but not of a control Ab. HIV-induced CCL2 up-modulation preceded the peak of virus replication and remained sustained up to 35 days after infection (Figure 1A), as reported.8 A similar inhibition of HIV-1 replication was observed in MDM cultures treated with a monoclonal anti-CCL2 Ab (data not shown). The effect of CCL2 neutralization was concentration-dependent with the maximal activity at Ab concentrations ranging from 500 to 1000 ng/mL (Figure 1B). As shown in Figure 1C, lower levels of p24 Gag Ag were also detected in the culture supernatants of MDMs infected with primary isolates, previously characterized as monotropic (R5) and dualtropic (R5X4) viruses,17 in the continuous presence of anti-CCL2 Ab, whereas no effect was observed with a control Ab. We next investigated which step(s) of the HIV life cycle was affected by CCL2 neutralization. To this purpose, the kinetics of accumulation of HIV-1 DNA were measured by real-time polymerase chain reaction (PCR), according to a published method.18 A comparable number of viral DNA copies were observed in both control and Ab-treated cultures up to 72 hours after infection (data not shown). In consideration that a single round of replication occurs in macrophages in approximately 48 hours,19 these results suggested that the inhibitory effect on HIV replication by anti-CCL2 Ab likely involved a postentry step of the virus life cycle. In keeping with this hypothesis, comparable levels and ratios between unspliced and multiply-spliced HIV-1 mRNA were detected in anti-CCL2 Ab-treated and control Ab-treated MDM cultures 3, 6, and 13 days after infection (data not shown). Thus, the suppressive effect of anti-CCL2 Ab unlikely involved either viral entry or the synthesis and steady-state accumulation of viral transcripts. Accordingly, despite the reduction of p24 Gag Ag release from MDM cultures infected in the presence of anti-CCL2 Ab, the cell-associated content of p24 Gag Ag was significantly higher in the latter with respect to control cultures (Figure 1D). Overall, these results indicated that CCL2 secretion modulates HIV particle production by affecting late stages of the retroviral life cycle.
Neutralization of endogenous CCL2 inhibits HIV-1 replication in MDMs by promoting the intracellular accumulation of p24 Gag Ag. (A) MDM cultures were infected with HIV-1BaL (300 TCID50/106 cells) in the presence (▴) or in the absence (○) of a polyclonal anti-CCL2 Ab (2.5 μg/mL). Some cultures were maintained in the continuous presence of a control Ab (•). After 2 hours, cells were washed and maintained in complete medium either in the presence or in the absence of anti-CCL2 or control Ab. At the indicated time points, culture supernatants were collected and tested for p24 Gag Ag and CCL2 content (gray bars indicate uninfected cells; hatched bars, infected cells). Shown is 1 representative experiment of 7 independently performed. (B) Concentration-dependent effect of the Ag affinity-purified polyclonal Ab to CCL2 on HIV-1BaL p24 Gag Ag release. MDMs were infected as described above in the presence of different concentrations of Ab to CCL2, ranging from 62.5 ng/mL to 1000 ng/mL, or control Ab. At the indicated time points, culture supernatants were collected and tested for p24 Gag Ag content. Shown is 1 representative experiment of 2 independently performed. (C) MDMs were infected with primary R5 and R5X4 isolates. At the indicated time points, culture supernatants were collected and tested for p24 Gag Ag release. (D) MDMs were infected with HIV-1BaL. At the indicated time points, cells were harvested and lysed. The cell-associated content of p24 Gag Ag was quantified by ELISA and normalized to 105 cells. The results represent an individual experiment of 3 performed. The intersample SD calculated in all experiments did not exceed 10%. Statistical analysis showed a significant decrease in terms of p24 Gag Ag released in the culture medium (A-C) and a significant increase in terms of intracellular p24 Gag Ag accumulation (D) in HIV-1-infected anti-CCL2-treated cultures with respect to control cultures (P < .05).
Neutralization of endogenous CCL2 inhibits HIV-1 replication in MDMs by promoting the intracellular accumulation of p24 Gag Ag. (A) MDM cultures were infected with HIV-1BaL (300 TCID50/106 cells) in the presence (▴) or in the absence (○) of a polyclonal anti-CCL2 Ab (2.5 μg/mL). Some cultures were maintained in the continuous presence of a control Ab (•). After 2 hours, cells were washed and maintained in complete medium either in the presence or in the absence of anti-CCL2 or control Ab. At the indicated time points, culture supernatants were collected and tested for p24 Gag Ag and CCL2 content (gray bars indicate uninfected cells; hatched bars, infected cells). Shown is 1 representative experiment of 7 independently performed. (B) Concentration-dependent effect of the Ag affinity-purified polyclonal Ab to CCL2 on HIV-1BaL p24 Gag Ag release. MDMs were infected as described above in the presence of different concentrations of Ab to CCL2, ranging from 62.5 ng/mL to 1000 ng/mL, or control Ab. At the indicated time points, culture supernatants were collected and tested for p24 Gag Ag content. Shown is 1 representative experiment of 2 independently performed. (C) MDMs were infected with primary R5 and R5X4 isolates. At the indicated time points, culture supernatants were collected and tested for p24 Gag Ag release. (D) MDMs were infected with HIV-1BaL. At the indicated time points, cells were harvested and lysed. The cell-associated content of p24 Gag Ag was quantified by ELISA and normalized to 105 cells. The results represent an individual experiment of 3 performed. The intersample SD calculated in all experiments did not exceed 10%. Statistical analysis showed a significant decrease in terms of p24 Gag Ag released in the culture medium (A-C) and a significant increase in terms of intracellular p24 Gag Ag accumulation (D) in HIV-1-infected anti-CCL2-treated cultures with respect to control cultures (P < .05).
Besides these modulatory effects on HIV-1 replication, anti-CCL2 Ab-treated MDM cultures revealed remarkable morphologic changes and an increase in cell size with respect to control cultures, which were unrelated to HIV infection (data not shown). This observation suggests that CCL2 neutralization induced changes in cytoskeleton organization, leading to cell morphology alterations. In this regard, it has been reported that cytoskeleton organization affects chemokine response and migration20 and HIV-1 release by monocytoid cells.21
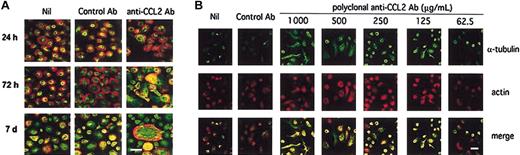
Thus, we carried out fluorescence CLSM experiments to evaluate whether endogenous CCL2 neutralization could induce rearrangements in cytoskeleton components. As shown in Figure 2A, time-dependent changes of α-tubulin, actin distribution, and cell size increase were observed in MDM cultures treated with anti-CCL2 Ab with respect to control cultures. In particular, a marked anteroposterior actin polarization was already observed after 24 hours of treatment, whereas a massive polarization of actin, exhibiting a similar localization with α-tubulin on uropodes, and activated macrophage morphology were consistently detected after 72 hours. After 7 days of culture, anti-CCL2 Ab-treated MDMs showed a significantly lower actin polarization with respect to cultures at 72 hours of treatment. Furthermore, the appearance of giant cells exhibiting a normal pattern of cytoskeleton organization was observed (Figure 2A). Moreover, concentration-dependent morphologic changes were observed in the presence of different concentrations of polyclonal (Figure 2B) as well as monoclonal (data not shown) Ab to CCL2, but not in the presence of control Ab.
Neutralization of endogenous CCL2 results in cytoskeleton rearrangements and cell size modification in MDMs. (A) Dual-fluorescence CLSM analysis was performed on fixed MDMs double stained for α-tubulin (green) and actin (red) at different time points of culture. Shown is 1 representative experiment of 3 performed. (B) Dual fluorescence CLSM analysis was performed on MDMs maintained in the presence of different concentrations of the Ag affinity-purified polyclonal Ab to CCL2 or control Ab for 72 hours, fixed and double stained for α-tubulin and actin. The bars, indicated in the lower right panels, correspond to 20 μm.
Neutralization of endogenous CCL2 results in cytoskeleton rearrangements and cell size modification in MDMs. (A) Dual-fluorescence CLSM analysis was performed on fixed MDMs double stained for α-tubulin (green) and actin (red) at different time points of culture. Shown is 1 representative experiment of 3 performed. (B) Dual fluorescence CLSM analysis was performed on MDMs maintained in the presence of different concentrations of the Ag affinity-purified polyclonal Ab to CCL2 or control Ab for 72 hours, fixed and double stained for α-tubulin and actin. The bars, indicated in the lower right panels, correspond to 20 μm.
Thus, our study supports the hypothesis that CCL2 affects HIV replication in macrophages with a mechanism(s) clearly distinct from the inhibition of viral entry typical of CCR5-binding chemokines or of CXC chemokine ligand 12 (CXCL12).2 Indeed, early events of HIV life cycle were not affected by CCL2 neutralization that down-regulated either assembly or release of new progeny virions. In this regard, independent studies have already provided evidence on the importance of cytoskeleton structures in late events of the HIV-1 life cycle, including virion assembly and release21-23 as well as in the regulation of chemotactic response and chemokine receptor binding affinity.24-26 In keeping with our hypothesis, Choudhury et al23 reported that polarization of F-actin, induced by cell-to-cell adhesion, might facilitate HIV retention inside infected T cells. However, previous studies have implicated the host cell cytoskeleton not only in late events of the viral life cycle, but also in early steps of infection. In particular, Bukrinskaya et al27 suggested that cytoskeleton components played a crucial role in HIV entry, promoting establishment of the reverse-transcription complex in the host cells as well as the process of reverse transcription within this complex.
Although we do not have direct proof linking morphologic changes induced by CCL2 neutralization with virus production efficiency, our study supports the hypothesis that the constitutive production of CCL2 might contribute to the maintenance of the macrophage morphology by affecting cytoskeleton organization. These modifications might play some role in the increased intracellular accumulation of viral proteins and virions without substantial cytopathic effect. It is also possible that CCL2 neutralization could result in some changes at the level of plasma membrane, ultimately affecting the efficiency of viral assembly and release. A similar mechanism of action may also be responsible, at least in part, for the anti-HIV activity of other chemokines and cytokines.2 For instance, type I interferons (IFNs), secreted during the course of viral infections, including HIV-1, have been described to interfere with either viral assembly, release, or the infectivity of viral progeny, an effect that has been correlated to changes in membrane rigidity, microfilament organization, cell metabolism, and expression of cell surface molecules.28 More recently, a similar mechanism has been observed in differentiated monocytoid cells chronically infected with HIV and treated with urokinase-type plasminogen activator,29 underscoring that multiple signaling pathways may lead to similar effects on HIV particle assembly and release.
These results together suggest that chemokines may influence HIV replication in macrophages by acting at postentry levels in the HIV life cycle in addition to their well-known ability to compete for gp120 binding to entry coreceptors. It remains to be determined whether the striking effect of CCL2 neutralization on cell morphology and cytoskeleton organization may ultimately influence viral replication and spreading by affecting cell components important for viral assembly and release from macrophages.
Prepublished online as Blood First Edition Paper, June 12, 2003; DOI 10.1182/blood-2002-10-3275.
Supported by the grants 40D.7 of the III and 40D.68 of the IV National Program on AIDS from the Italian Ministry of Health (S.G. and F.B.).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank Sabrina Tocchio and Anna Maria Fattapposta for excellent editorial assistance, Stefano Billi for preparing drawings, and Barbara Varano for technical help.