Abstract
High hyperdiploidy (HeH) (51 to 65 chromosomes) is found in one third of children with acute lymphoblastic leukemia and is associated with a good prognosis. Cytogenetic features may further refine this prognosis and identify patients with a poor outcome. We examined the effect of sex, age, individual trisomies, modal number, and structural abnormalities on survival among 700 children with HeH. Univariate analysis showed that age. sex, +4, +10, +18, and a high modal number were associated with survival. Multivariate analysis however, revealed that only age, sex, +4, and +18 were independent indicators. Hazard scores for predicting relapse and mortality were constructed. Three risk groups with 5-year event-free survival (EFS) rates of 86%, 75%, and 50% (P < .0001) were identified. The high-risk group comprised boys older than 9 years, boys aged 1 through 9 years without +18, and girls older than 9 years without +18, while girls aged 1 through 9 years with +18 had the best EFS. In terms of mortality, those younger than age 10 years with both +4 and +18 had an improved survival (96% vs 84% at 5 years, P < .0001). These findings confirm that the outcome of children with HeH is heterogeneous and that specific trisomies can identify patients with the greatest and least risk of treatment failure.
Introduction
Up to one third of children presenting with acute lymphoblastic leukemia (ALL) have a high-hyperdiploid (HeH) karyotype, defined as the presence of 51 to 65 chromosomes.1,2 Significantly, HeH has been shown to be an independent risk factor.1 Children with HeH ALL respond well to standard chemotherapy regimens and have consistently shown a superior outcome when compared with their nonhyperdiploid counterparts.2-8 Recent studies have reported event-free survival (EFS) rates of up to 80% at 5 years for children with HeH ALL. Despite the relatively good outlook for these children, around a quarter will suffer an adverse event within 5 years of diagnosis. Therefore, continuing investigation of this subgroup of patients is important to identify those at an increased risk of treatment failure who might then be considered for more intensive or alternative therapy. Three publications have suggested that the gain of specific chromosomes is associated with an improved prognosis: +6,9 +4/+10,10 and +10/+17,2 while one study reported that HeH cases with +5 had a worse prognosis.2 Other studies have proposed that the presence of structural abnormalities11 or a lower modal chromosome number (MCN) (51 to 55 versus 56 to 67 chromosomes)12 predicts relapse. Clearly, these studies do not agree, and whether or not any of these cytogenetic features are true and independent predictors of outcome remains to be established. To evaluate the prognostic importance of specific trisomies, MCN, and structural abnormalities alongside other established risk factors, such as age and sex, we have studied the outcome of 700 children with ALL presenting with an HeH karyotype. The large number of cases accrued has permitted a comprehensive investigation and enabled the construction of hazard scores for predicting relapse and mortality.
Patients and methods
Patients
All patients had a confirmed diagnosis of ALL and were recruited onto the Medical Research Council (MRC) UKALLXI or ALL97 treatment trials.1,13 Individual centers in the United Kingdom obtained approval for the study from their local research ethics committee. Each center obtained informed consent from patients and parents before enrolling patients in the study. Demographic, clinical, and survival data were collected by the Clinical Trial Service Unit in Oxford (United Kingdom). UKALLXI recruited children aged between 1 and 15 years inclusive from October 1990 to March 1997. ALL97 recruitment included patients up to the age of 18 years beginning in January 1997 and continuing until June 2002. The current study includes ALL97 cases diagnosed up to the end of November 1999. Both trials excluded patients diagnosed with mature B-ALL. Full details of the protocols have been published previously.1,13 Briefly, the schedules comprised an induction course, followed by a number of intensification blocks and central nervous system (CNS)–directed treatment. Patients received interim therapy and were treated for a total of 100 (UKALLXI) or 105 (ALL97) weeks. All patients received an intensification block at week 20 and were randomized to receive an additional block at week 5 until May 1991, after which everyone received both blocks. From March 1992, patients were randomized to receive a third intensification block at week 35, when daunorubicin was dropped from induction. This randomization continued until May 1998, when all children who had not yet reached week 35 were recommended to receive the third intensification block. In UKALLXI, patients with a low white blood cell (WBC) count (lower than 50 × 109/L) were randomized to receive high-dose intravenous methotrexate (MTX) as well as intrathecal MTX as part of their CNS therapy. However, in ALL97, all patients with a low WBC count received intrathecal MTX alone. In both UKALLXI and ALL97 patients with a high WBC count (more than 50 × 109/L) were randomized between high-dose MTX and cranial radiotherapy. High-dose MTX did not confer any increase in EFS, whereas patients receiving a third intensification block did have an 8% higher EFS at 5 years but no increase in overall survival (OS).13,14
Cytogenetic analysis
Diagnostic pretreatment bone marrow and/or peripheral blood samples were cultured and analyzed by standard cytogenetic methods in the member laboratories of the United Kingdom Cancer Cytogenetics Group (UKCCG). Slides and karyotypes were reviewed by the Leukaemia Research Fund (LRF) UKCCG Karyotype Database (Database).15 All karyotypes entered to the Database were described according to the International System for Human Cytogenetic Nomenclature.16 The Chromoprobe Mulitprobe-I system (Multiprobe-I; Cytocell, Banbury, United Kingdom),15 which allows the simultaneous enumeration of up to 24 chromosomes, was used to: (1) identify hidden HeH clones in 14 cases with a normal karyotype or failed cytogenetic result or (2) clarify the chromosomes gained in 22 HeH karyotypes with poor chromosome morphology. Fluorescence in situ hybridization (FISH) using alpha satellite centromeric probes (Qbiogene, Illkirch, France) was performed, in accordance with the manufacturer's instructions, on a further 24 cases to confirm the gain of 1, 2, or 3 chromosomes. Karyotypes with a modal chromosome number between 51 and 65 inclusive were classified as having HeH and were included in the present study. HeH karyotypes were classified as being incomplete in cases in which (1) the modal chromosome number could not be accurately determined owing to poor metaphase quality and/or an insufficient level of analysis, or (2) the HeH karyotype was identified solely through the use of the Multiprobe-I. Cases were further classified by modal chromosome number, by the presence or absence of structural chromosomal abnormalities, and by the gain of individual chromosomes. In cases where the abnormal cells had not all gained the same number of chromosomes (ie, composite karyotypes and evolving clones), the modal chromosome number was determined from the total number of clonal gains and/or losses present.
Statistical analyses
EFS was measured from the start of treatment to the first adverse event, whether relapse or death, and included patients who failed to achieve a complete remission (n = 2) and those who died in remission (n = 12). OS was defined as the time from the start of treatment to death. Patients who did not suffer an event or die within the follow-up period were censored at the date of last contact. Kaplan-Meier life tables and curves were constructed by means of the log-rank method.17 Unless otherwise stated, the EFS and OS rates are quoted at 5 years. The observed-expected ratios presented are from unadjusted log-rank tests comparing 2 or more groups. Where 2 groups were compared, the P is for heterogeneity, whereas if more than 2 groups were compared, the P presented is for trend. The large number of cytogenetic variables examined increased the probability that a conventionally significant result (P < .05) would be found by chance. Therefore, to safeguard against spurious results, a more stringent significance level (P < .01) was used throughout the study. Multivariate analysis of variables found to be significant in univariate log-rank tests was performed by means of the Cox proportional hazards model.18 Significant variables were added to the model in a stepwise manner and removed if they failed to retain their significance. The final Cox model was used to generate a hazard score from which the risk groups were derived. All statistical analysis was performed by means of Intercooled Stata v7 (Stata, College Station, TX).
Results
Among 2524 children with ALL and a successful cytogenetic result, 815 (32%) were found to have an HeH karyotype. An established chromosomal translocation was observed in 8 cases: t(1;19)(q23;p13) (n = 4); t(9;22)(q34;q11)(n = 1); t(12;21)(p13; q21)(n = 1); and an 11q23 translocation (n = 2). These 8 cases were excluded from the remainder of the study because (1) they represent biologically distinct subgroups that may have independent prognostic implications; (2) it is impossible to know which was the primary abnormality; and (3) the number of cases was too small to examine the interaction between translocations and numerical abnormalities in terms of prognosis. The median follow-up time for the remaining 807 patients was 5 years and 3 months (range, 9 months to 10 years and 11 months), during which time 201 (25%) patients suffered an adverse event and 76 (9%) died. The resulting 5-year EFS was 73% (95% confidence interval [CI], 69%-76%), and the 5-year OS was 91% (95% CI, 88%-93%). There was no significant difference in EFS or OS between cases with incomplete karyotypes (n = 107) and those with the other karyotypes (n = 700): EFS 73% (95% CI, 62%-80%) versus 73% (95% CI, 69%-76%), and OS 91% (95% CI, 83%-95%) versus 90% (95% CI, 88%-93%), respectively. In addition, there was no difference in the age, sex, or WBC count distributions of the 2 groups of patients. Since incomplete karyotypes could not be reliably classified according to the cytogenetic parameters examined, these cases were excluded from the remainder of the study.
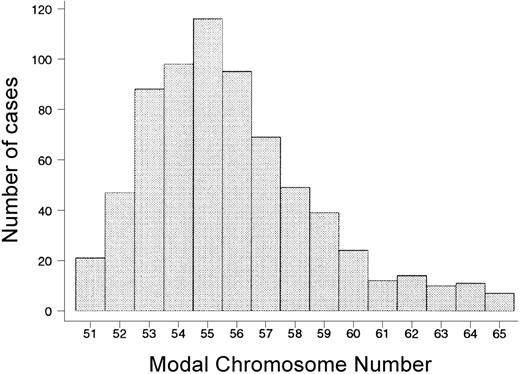
A total of 6917 chromosomes were gained across the remaining 700 karyotypes, averaging nearly 10 extra chromosomes per case. The vast majority of cases (92%) had gained between 5 and 14 chromosomes (MCN, 51 to 60 inclusive), and the most frequent MCN was 55 chromosomes (Figure 1). The gain of chromosomes was nonrandom, and 8 chromosomes accounted for 77% of all gains: +4 (78% of cases), +6 (85%), +10 (63%), +14 (84%), +17 (68%), +18 (76%), +21 (99%), and +X (89%) (Figure 2). Gains of chromosomes 5, 8, 9, 11, 12, 22, and Y represented 14% of the total and were present in between 14% and 37% of cases. The gain of chromosomes 1, 2, 3, 7, 13, 15, 16, 19, and 20 was rare, in total making up just 5% of chromosomes gained. In most cases (73%), all the chromosome gains were identified. Only 4% of additional chromosomes were undefined and thus described as marker chromosomes. Trisomy (1 extra copy) was much more common than tetrasomy or pentasomy (2 or 3 extra copies) (85% versus 15%), with the exception of tetrasomy 21 which was present in 70% of cases.
Distribution of 700 cases of childhood high-hyperdiploid acute lymphoblastic leukemia cases by modal chromosome number.
Distribution of 700 cases of childhood high-hyperdiploid acute lymphoblastic leukemia cases by modal chromosome number.
Number of childhood high-hyperdiploid acute lymphoblastic leukemia cases with trisomy, tetrasomy, and pentasomy of each chromosome (N = 700). □ indicates trisomy; ▦, tetrasomy; and ▪, pentasomy. mar indicates marker chromosome.
Number of childhood high-hyperdiploid acute lymphoblastic leukemia cases with trisomy, tetrasomy, and pentasomy of each chromosome (N = 700). □ indicates trisomy; ▦, tetrasomy; and ▪, pentasomy. mar indicates marker chromosome.
Structural chromosomal abnormalities were evident in 371 (53%) cases. Abnormalities of the long arm of chromosome 1 (1q) were the most frequent type (n = 105, 15%) and usually included a partial duplication of 1q (n = 100), via either a duplication (n = 66) or an unbalanced translocation (n = 34). Deletions of 6q (del(6q)) were seen in 49 (7%) cases and were usually independent of 1q abnormalities, with only 4 cases having both aberrations. Isochromosomes were present in 28 cases (4%), the most frequent of which was i(17)(q10), present in 12 cases (2%).
The effect of age, sex, and WBC count on outcome among the 700 HeH children is shown in Table 1. Younger children (aged 1 year through 9 years) fared better than older ones (aged 10 through 16 years): EFS of 75% (95% CI, 71%-78%) compared with 57% (95% CI, 42%-70%). There was no significant difference in outcome between children aged 1 through 4 years and those aged 5 through 9 years. Although boys had a lower EFS (67% [95% CI, 62%-72%]) than girls (82% [95% CI, 76%-86%]), this difference was not reflected in a significantly decreased OS at 5 years (89% [95% CI, 85%-92%] versus 93% [95% CI, 90%-96%]). Over half of the patients had a WBC count below 10 × 109/L and 90% had one below 50 × 109/L (Table 1). There was no evidence of an association between EFS or OS and WBC count, whether the analysis was performed across the 5 groups listed in Table 1 or as a comparison between patients with lower than or more than 50 × 109/L (data not shown).
Overall, the presence of structural abnormalities had no effect on survival. The 5-year EFS and OS were similar in cases with and without structural aberrations: EFS of 75% (95% CI, 70%-79%) versus 71% (95% CI, 65%-76%) and OS of 91% (95% CI, 87%-94%) versus 90% (95% CI, 85%-93%). Patients with 1q abnormalities, del(6q), or i(17)(q10) had comparable EFS and OS rates compared with those without these abnormalities (data not shown).
When the prognostic effect of the gain of individual chromosomes was examined, only trisomies of chromosomes 4, 10, and 18 showed any significant effect (Table 2). In each case, patients with these trisomies had a better outcome than those without the relevant trisomy. Trisomy 18 conferred a lower relapse risk and increased OS, whereas trisomy 4 patients had an improved OS but no reduction in relapse risk. The opposite was true for trisomy 10 patients, who showed a better EFS but no overall gain in survival. There was no material difference in the results obtained whether or not cases with a marker chromosome, which could be an unidentified trisomy 4, 10, or 18, were excluded from the comparison group (ie, those without the relevant trisomy) when the log-rank test was performed.
The large number of cases in this series permitted an extensive analysis of the effect of chromosome number on EFS and OS (Table 3). Cases with 61 to 62 and 63 to 65 chromosomes were grouped together to ensure that each group had a minimum of 20 cases. There was no evidence for a strong trend effect, that is, an association of increasing MCN with increasing survival, as the P for trend were greater than .01. However, the observed-expected ratios derived from the log-rank analysis did suggest a threshold MCN level: cases with an MCN of 51 to 53 suffered a greater number of relapses and deaths than expected, whereas those with an MCN of 54 to 65 experienced fewer adverse events than expected. The log-rank test comparing patients having 51 to 53 chromosomes with those having 54 to 65 chromosomes showed a significantly better prognosis in terms of both EFS and OS for children with 54 to 65 chromosomes (P = .0002).
Cox models were fitted to assess the relative prognostic importance of age; sex; trisomies 4, 10, and 18; and MCN (Table 4). In the EFS model, trisomy 18, sex, and age all had significant multivariate effects, unlike trisomy 10 and MCN. In the OS model, the variables remaining significant were trisomy 18, age, and trisomy 4, but with MCN again not proving significant in multivariate analysis. HeH karyotypes with an MCN of 54 to 65 chromosomes are more likely to have trisomies of chromosomes 4, 10, and 18 (P < .0001 for each) compared with cases with an MCN of 51 to 53 chromosomes, a finding that explains why MCN was significant in univariate, but not multivariate, analysis.
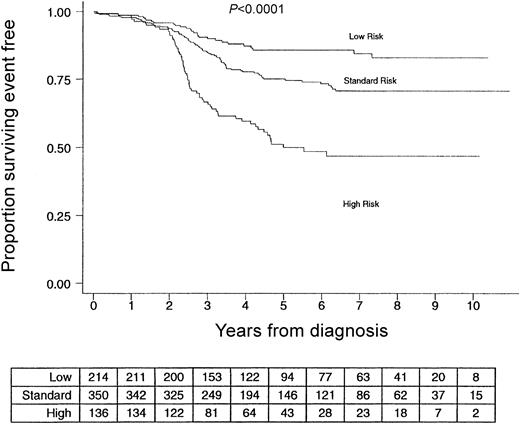
The results from the Cox analysis were used to construct 2 hazard scores from which EFS and OS risk groups were derived (Table 5). Age, sex, and trisomy 18 status can be used to define groups of children with either a low, standard, or high risk of relapse (Figure 3). Girls younger than 10 years old with trisomy 18 have a 5-year EFS of 86% (95% CI, 80%-90%). In contrast, boys older than 10 years or without trisomy 18, along with girls without trisomy 18 and older than 10 years, had a 5-year EFS of just 50% (95% CI, 40%-59%). When OS was considered, the relevant variables were age, trisomy 4, and trisomy 18. Children younger than the age of 10 years with both trisomy 4 and trisomy 18 had an OS of 96% compared with 84% for the remaining patients.
Event-free survival of 700 children with high-hyperdiploid acute lymphoblastic leukemia by risk group based on age, sex, and trisomy 18 status. Table shows the number of patients in each risk group who are at risk of relapse at the start of each year.
Event-free survival of 700 children with high-hyperdiploid acute lymphoblastic leukemia by risk group based on age, sex, and trisomy 18 status. Table shows the number of patients in each risk group who are at risk of relapse at the start of each year.
As both UKALLXI and ALL97 were randomized clinical trials, not all children in this study received identical treatment. Even though the randomizations were independent of karyotype, we sought to confirm that the hazard scores retain their prognostic relevance among patients randomized to different treatment arms. The 2 randomizations that accrued sufficient numbers of cases for consideration in this analysis were the administration of the third intensification block and the addition of high-dose MTX to the CNS therapy of cases with a low WBC count (lower than 50 × 109/L). Therefore, we performed stratified log-rank tests on reduced data sets, comprising only those patients randomized to a particular treatment arm. For both randomizations, the 2 hazard scores remained statistically significant among the patients randomized to each of the relevant treatment arms (data not shown).
Discussion
We have assessed the prognostic importance of age, sex, WBC count, and a range of cytogenetic characteristics in a large series of children with HeH ALL. The main finding of this study was that the outcome of children in this subgroup was not uniformly favorable. Although, the well-established risk factors of age and sex retained their prognostic importance within this subgroup, the presence of specific trisomies (+4 and +18) also had strong independent effects. In this study, boys were more likely to relapse than girls, although there was little or no sex difference in overall survival. Boys are known to have an increased risk of bone marrow relapse and also have the additional risk of testicular relapse.19 This observation implies either a good response to their postrelapse treatment or that the follow-up period was insufficient to detect a difference in OS. When the variables with significant multivariate effects are used, children can be classified into risk groups that identify patients with an increased risk of relapse or mortality. Patients with the highest risk of relapse were boys older than the age of 10 years, girls older than the age of 10 years without trisomy 18, and boys aged 1 to 9 years without trisomy 18. Collectively, this group of patients had an EFS of just 50% at 5 years. This poor EFS was in contrast to girls aged 1 to 9 years with +18, who had an excellent EFS: 86% at 5 years. Patients aged younger than 10 years with trisomies of both chromosomes 4 and 18 had the best OS: 96% at 5 years. Not only are both these hazard scores simple to implement, but the distribution of cases across the groups is such that the scores could be clinically relevant. The advent of interphase FISH methods, for example Multiprobe-I, will allow cytogenetically normal and failed cases to be routinely screened for hidden HeH cases. Therefore, in theory the hazard scores described in this study should be applicable to all children with HeH ALL.
One of the main strengths of this study is its size. To date, this is the largest cohort of children with HeH ALL to be investigated with this approach. It is also the first analysis of this kind to emerge from Europe. All the children were diagnosed within a single decade and were treated on successive MRC UKALL trials, giving rise to the most uniformly treated group of patients possible for this type of analysis. The study had a long follow-up with a median of 5 years and includes only 14 patients with fewer than 2 years' follow-up. All karyotypes were centrally reviewed by a small team of cytogeneticists highly experienced in the analysis of ALL metaphases. The large number of cases collected not only allowed ill-defined karyotypes to be removed from the main part of the analysis, but also enabled us to repeat the analysis excluding cases with unidentified marker chromosomes. The observation that this exclusion did not materially alter the results, further endorses the validity of our findings. In addition, both hazard scores retained their prognostic relevance among patients randomized to different arms, indicating that the scores can still predict patients with the greatest and least chance of relapse over and above any beneficial effects derived from the treatment randomizations. In an attempt to safeguard against chance significant results in a study that necessitated multiple testing, we chose to use a P value of less than .01 as our level of significance.
The initial observation, that the presence of structural abnormalities in HeH patients affected prognosis,11 was not confirmed by a subsequent study12 or by this one, and therefore it now seems unlikely that such abnormalities are of prognostic importance. This included the presence of i(17)(q10), previously thought to confer a poor prognosis,12 which also had no effect on survival. Patients with an established translocation were excluded from the analysis in this study, but the number of exclusions (n = 8) was too small to affect the interpretation of the results. This study was not able to assess the prognosis of cases with both HeH and an established translocation because of a lack of cases. Clearly the interaction of HeH with a chromosomal translocation is an important clinical question that is best addressed at the international level. Additionally, this study, like previous ones, cannot comment on the prognostic importance of cytogenetically invisible structural abnormalities with an HeH karyotype. A low MCN (fewer than 54 chromosomes) had also been associated with a poor prognosis2,12 ; however, our results suggested that this association was not independent of the effect of specific trisomies. This finding was not surprising given the relationship between the gain of individual chromosomes and MCN,20 which in turn is a consequence of the fact that the gain of chromosomes is nonrandom and tetrasomy (excluding tetrasomy 21) is a rare event. In agreement with previous studies,2,9,10 we have concluded that the gain of specific chromosomes confers a survival advantage. We did not find that trisomy 5 was associated with a poor prognosis, as suggested by the Children's Cancer Group (CCG).2 While other groups concluded that trisomies of 6, 4/10, and 10/17 are the chromosomes of principal interest,2,9,10 we have found +4 and +18 to be the most useful predictors of outcome. This does not, however, imply a complete disagreement between the studies. Examining the 3 main studies (the current study, Pediatric Oncology Group [POG],10 and the CCG2 ) in more detail revealed some common ground. In univariate analysis, all 3 groups found +10, +17, and +18 to be associated with improved survival (+17 was borderline in this study), while this study and POG found +4 to be linked to an improved outcome. Clearly, the differences between the 3 groups stem from the conclusions drawn from multivariate analysis. While the differences may have arisen owing to methodologic variation among the 3 groups, they could simply reflect the fact that this study was based on a larger number of cases and a data set that was diagnosed and analyzed more recently. However, given that two thirds of the cases have gained at least 3 of these 4 chromosomes (data not shown), it is perhaps not surprising that there is some variation among these studies. During routine FISH screening, we have found that chromosomes 17 and 18 are gained together more frequently than suggested by cytogenetics alone (N. Sumption, unpublished observation, September 2000). This is one possible explanation as to why our analysis considers +18 to be of greater prognostic relevance than +17, in contrast to the CCG study.
Although we do not know why high hyperdiploidy is associated with a good prognosis, several studies have suggested that HeH cells are more sensitive to certain drugs (especially methotrexate, mercaptopurine, and l-asparaginase) than nonhyperdiploid cells.21-24 Cellular drug resistance is derived largely from the genetic makeup of the individual; therefore, the hypothesis that the gain of whole chromosomes and the associated gene-dosage effects might alter drug sensitivity seems plausible. Moreover, cases with +4 and +10 may be even more susceptible to certain drugs than HeH cases without these trisomies.22,25 These suggestions support the assertion made in this paper and by CCG and POG that within HeH the gain of a particular chromosome is sufficient to alter prognosis. If drug sensitivity is indeed linked to specific trisomies, treatment differences may be the reason we found +18 and the CCG found +17 to be the chromosome most closely associated with survival. The widespread use of interphase FISH to detect specific trisomies will, it is hoped, provide future studies with more precise cytogenetic data from which to derive even more predictive hazard scores. Furthermore, the use of DNA microarray technology and comparative expressed-sequence hybridization (CESH) will undoubtedly shed light on the molecular consequences of hyperdiploidy and its potential role in drug sensitivity.
Appendix
The members of the MRC Childhood Leukaemia Working Party during the period of these studies were as follows: C. C. Bailey, C. J. Barton, V. A. Broadbent, M. Caswell, J. M. Chessells, P. J. Darbyshire, S. I. Dempsey, I. J. Durrant, T. O. B. Eden, K. M. Forman, B. E. S. Gibson, A. Goodman, R. Gray, I. M. Hann, C. J. Harrison, C. Haworth, F. G. H. Hill, M. Jenney, J. Kernahan, D. J. King, S. E. Kinsey, M. Madden, J. R. Mann, J. Martin, S. T. Meller, C. D. Mitchell, A. Oakhill, M. Radford, M. M. Reid, S. M. Richards, O. P. Smith, R. F. Stevens, A. Thomas, F. Vargha-Khadem, A. J. Vora, D. Walker, D. Webb, K. Wheatley, A. M. Will, and K. P. Windebank.
Prepublished online as Blood First Edition Paper, June 26, 2003; DOI 10.1182/blood-2003-04-1128.
A list of the members of the Medical Research Council's Childhood Leukaemia Working Party during the period of these studies appears in the “Appendix.”
Supported by the Leukaemia Research Fund, the Medical Research Council, and Cancer Research UK.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
The authors would like to thank all the member laboratories of the United Kingdom Cancer Cytogenetics Group (UKCCG); all the pediatric hematologists/oncologists who entered patients into either trial; and previous LRF UKCCG Karyotype Database staff, especially Jackie Hawkins, Dianna Farrell, Roslyn Clark, Kathryn Roberts, and Natalia Sumption. A full list of the UKCCG laboratories is available on request.