Abstract
Plasmacytoid dendritic cells (PDCs) are crucial effectors in innate immunity. In this study, we show that imatinib, a potent inhibitor of BCR/ABL tyrosine kinase activity, in the presence of Flt3-Ligand, could induce CD34+ progenitors from chronic myeloid leukemia (CML) to give rise in vitro to typical BDCA-2+ type I interferon-producing PDCs. The effect of imatinib on PDC generation was related to up-regulation of Flt3 on leukemic CD34+ progenitors. Moreover, patients with chronic myeloid leukemia (CML) who were in complete cytogenetic or molecular response after imatinib treatment restored their blood PDCs both quantitatively and functionally comparable to healthy donors, in contrast to patients not responding to imatinib, further confirming that disease response to imatinib is accompanied by restoration of PDC function in vivo. These findings provide evidence that response to imatinib is capable to restore some DC-related immune functions in CML that might be beneficial for long-term disease control. (Blood. 2004;103:4666-4668)
Introduction
Chronic myelogenous leukemia (CML) is a malignant clonal disorder of primitive hematopoietic progenitors characterized by a balanced translocation between chromosomes 9 and 22, leading to the fusion of a portion of the ABL gene with the BCR gene. The resulting BCR/ABL gene has been shown to play a critical role in the pathogenesis of CML. The BCR/ABL gene product demonstrates constitutive activation of tyrosine kinase activity1 that appears critical for BCR/ABL-induced transformation.2 Imatinib mesylate (Gleevec, STI571) has been demonstrated to be a potent inhibitor of ABL tyrosine kinases.3 Several studies demonstrated high levels of imatinib activity against BCR/ABL-containing cells4 with remarkable results in the treatment of CML.5 Despite the exciting success of this targeted cancer therapy, it is still needed to determine whether imatinib can also influence the immune functions in patients with CML, allowing for immune-mediated durable responses as it has been already shown after allogeneic stem cell transplantation.6 Dendritic cells (DCs) are responsible for the initiation and regulation of immune responses. The plasmacytoid DC (PDC) subset is a crucial effector in innate immunity.7 We and others have reported previously multiple abnormalities in blood DC subsets from leukemic patients, especially PDCs in CML.8-10 Although the exact role of PDCs in antitumor immunity has yet to be established, these results suggest that restoration of PDC function and other immune effectors function may be a goal for CML immunotherapy. Here, we investigated whether imatinib can affect PDC differentiation from patients with CML in vitro, and whether response to imatinib in vivo is accompanied by restoration of quantitative and functional properties of PDCs from patients with CML.
Study design
Patients and control subjects
CML cell samples were obtained after informed consent from 6 patients in chronic phase at diagnosis, and from 9 patients in chronic phase after treatment with imatinib. CML peripheral blood mononuclear cells (PBMCs) analyzed in this study were derived from patients treated at the Institut Paoli-Calmettes (Marseille) or at the Centre Hospitalier et Universitaire (CHU) de Nimes (Nimes). PBMCs from patients and healthy control subjects (Etablissement Français du Sang, Marseille, France) were isolated by standard density gradient centrifugation with Ficoll-Hypaque (Pharmacia, Uppsala, Sweden) prior to cryopreservation.
Blood DC detection and flow cytometry
Blood DCs were identified by 3-color staining performed on PBMCs as previously described.8,9 The following monoclonal antibodies were also used for standard flow cytometry8 : CD3, CD4, CD11c, CD14, CD16, CD19, CD34, ILT3, Flt3 (Beckman-Coulter, Marseille, France), CD56, CD123 (Pharmingen, San Diego, CA), and BDCA-2 (Miltenyi Biotec, Bergisch-Gladbach, Germany). Stained cells were analyzed on a FACSCalibur cytometer using CellQuest software (Becton Dickinson, San Jose, CA).
Generation of PDCs from leukemic CD34+ circulating progenitors
Circulating CD34+ progenitors from patients with CML were immunomagnetically purified with CD34 monoclonal antibody (mAb)-conjugated microbeads (Miltenyi Biotec). Cultures were established in 24-well culture plates in RPMI 1640 medium containing 10% fetal calf serum (FCS; BioWhittaker, Verviers, Belgium), 0.55 mM L-arginine, 0.24 mM L-asparagine, 2 mM L-glutamine (Life Technologies, Paisley, Scotland), in the presence of 100 ng/mL Flt3-ligand (Flt3L; R&D Systems, Abingdon, United Kingdom), 25 ng/mL stem cell factor (SCF), and 50 ng/mL thrombopoietin (TPO)11 all purchased from R&D Systems, with or without 1 μM imatinib added once at the beginning of culture (kind gift of Dr P. Dubreuil, INSERM U119, Marseille, France). Except for imatinib, the medium was replenished with cytokines every 5 days. For the interferon α (IFN-α) secretion assay, cells were plated in triplicates in 96-well round-bottomed plates either with medium alone, or with herpes simplex virus 1 (HSV; kind gift of Dr C. Zandotti, Hôpital La Timone, Marseille, France) as described previously.8 Supernatants were collected after 48 hours and tested for their IFN-α content by enzyme-linked immunosorbent assay (ELISA; ELISA kits; Beckman-Coulter).
Statistical analysis
Statistical comparisons were performed as previously described.9
Results and discussion
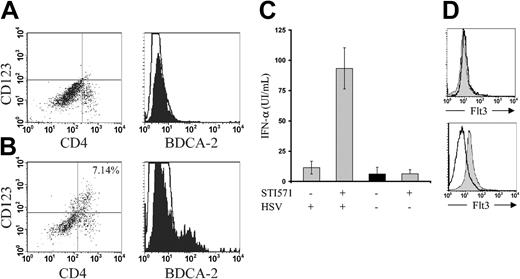
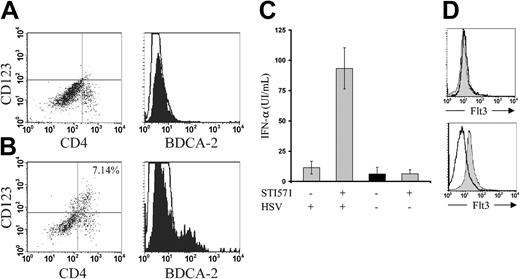
Several reports in humans and mice demonstrated that Flt3L can induce the generation of or can mobilize IFN-α-producing PDCs from CD34+ hematopoietic progenitors both in vitro and in vivo.11-13 Because elevated numbers of CD34+ progenitors have been previously described in the blood of patients with CML,14 we isolated circulating CD34+ progenitors from 6 patients with CML in chronic phase at diagnosis and cultured the progenitors with SCF, TPO, and Flt3L, a condition that is known capable to give rise to functional PDCs from CD34+ hematopoietic progenitors.11 After 17 to 21 days of culture, CML-derived CD34+ stem cells could not give rise to PDCs as shown by phenotypic analysis (Figure 1A), in line with previous data showing altered cell differentiation from CML-derived CD34+ progenitors.15 In contrast, the addition of imatinib at the beginning of culture allowed it to generate significant numbers of PDCs as ascertained by the simultaneous expression of CD4, CD123,11 and the typical PDC marker BDCA-216 (Figure 1B). These cells could secrete significant amounts of IFN-α following exposure to HSV (Figure 1C), further confirming that CD34+ leukemic progenitors can be induced to differentiate in vitro toward genuine type I IFN-producing PDCs11,17 in the presence of imatinib. To elucidate the mechanisms underlying the effect of imatinib on PDC generation, we could show that a 24-hour exposure of CML cells to imatinib up-regulated the expression of Flt3 on CML CD34+ progenitors (Figure 1D), in accordance with recent data suggesting that Flt3 expression and signaling might represent a prerequisite for DC development.18
Generation of functional PDCs from CML CD34+ progenitors in the presence of imatinib. CD34+ hematopoietic progenitors from CML patients in chronic phase at diagnosis were cultured in the presence of Flt3L as described in “Study design” (A) in the absence or (B) in the presence of imatinib. CD4, CD123, and BDCA-2 expression was analyzed by flow cytometry. Empty histograms show the background staining with isotype control monoclonal antibodies, and solid histograms represent specific staining of the indicated cell-surface markers. Representative of 4 independent experiments. (C) IFN-α secretion by PDCs generated from CD34+ CML progenitors in the presence of imatinib. Cells (106) from cultures described in panels A and B were stimulated with HSV without prior PDC sorting or any additional cytokine. Supernatants were harvested after 48 hours of stimulation with HSV. IFN-α secretion was analyzed by ELISA. Results are represented as the mean and SEM of IFN-α concentration obtained from 3 independent experiments. (D) Expression of Flt3 by flow cytometry is shown on CD34+ CML progenitors before (top panel), and after 24 hours of incubation of PBMCs from CML with imatinib. Empty histogram shows the background staining with isotype control monoclonal antibody, and solid histogram represents specific staining of Flt3. Representative of 6 different patients with CML in chronic phase at diagnosis.
Generation of functional PDCs from CML CD34+ progenitors in the presence of imatinib. CD34+ hematopoietic progenitors from CML patients in chronic phase at diagnosis were cultured in the presence of Flt3L as described in “Study design” (A) in the absence or (B) in the presence of imatinib. CD4, CD123, and BDCA-2 expression was analyzed by flow cytometry. Empty histograms show the background staining with isotype control monoclonal antibodies, and solid histograms represent specific staining of the indicated cell-surface markers. Representative of 4 independent experiments. (C) IFN-α secretion by PDCs generated from CD34+ CML progenitors in the presence of imatinib. Cells (106) from cultures described in panels A and B were stimulated with HSV without prior PDC sorting or any additional cytokine. Supernatants were harvested after 48 hours of stimulation with HSV. IFN-α secretion was analyzed by ELISA. Results are represented as the mean and SEM of IFN-α concentration obtained from 3 independent experiments. (D) Expression of Flt3 by flow cytometry is shown on CD34+ CML progenitors before (top panel), and after 24 hours of incubation of PBMCs from CML with imatinib. Empty histogram shows the background staining with isotype control monoclonal antibody, and solid histogram represents specific staining of Flt3. Representative of 6 different patients with CML in chronic phase at diagnosis.
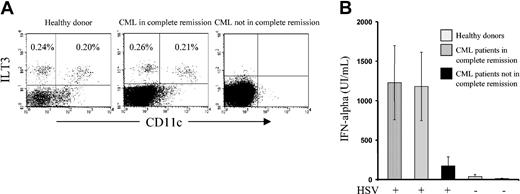
The effect of imatinib on PDC development in vitro prompted us to investigate whether response to imatinib in vivo could restore PDC numbers and function in patients with CML. Analysis of 7 patients who were in complete cytogenetic or molecular response under imatinib treatment demonstrated that these patients restored normal PDC numbers in comparison to healthy donors (P = NS; Figure 2A). In contrast, results obtained from 2 patients who could not reach cytogenetic responses under imatinib treatment showed that these 2 patients still had a severe depletion and altered function of their circulating blood PDC compartment (Figure 2A-B). In addition, we found that PDCs from patients responding to imatinib could secrete significant amounts of IFN-α, comparable to healthy donors (P = NS; Figure 2B), further confirming that response to imatinib is accompanied by restoration of the major PDC function in vivo.
Imatinib restores PDC function in vivo. (A) PBMCs isolated from healthy volunteers or patients with CML treated with imatinib were analyzed by flow cytometry after 3-color staining with a combination of FITC-labeled monoclonal antibodies against lineage markers (CD3, CD14, CD16, CD19, and CD56), phycoerythrin (PE)-labeled anti-CD11c and phycoerythrin-cyanin 5.1 (PC5)-labeled anti-ILT3. Two distinct populations of lin-/ILT3+ cells were observed with respect to the expression of CD11c with the phenotypes of lin-/CD11c+/ILT3+ (myeloid DCs) and lin-/CD11c-/ILT3+ (PDCs). Examples of results obtained from more than 15 healthy volunteers (left panel), 7 patients with CML in complete cytogenetic or molecular remission after imatinib treatment (middle panel), and 2 patients with CML not reaching cytogenetic or molecular remission after imatinib treatment (right panel). P = not significant for comparison of PDC numbers between healthy donors (left panel) and patients with CML in complete cytogenetic or molecular remission after imatinib treatment (middle panel). Percentages in upper left quadrants denote PDCs; in upper right quadrants, myeloid DCs. (B) IFN-α secretion by PDCs from healthy donors and patients with CML receiving imatinib treatment following stimulation with HSV. Cells were stimulated with HSV without any additional cytokine. Supernatants were harvested after 48 hours of stimulation. IFN-α secretion was analyzed by ELISA. Concentrations obtained from 104 PDCs are represented as the mean and SEM of IFN-α secretion obtained from 5 healthy donors, 5 patients with CML in complete cytogenetic or molecular remission after imatinib treatment, and 2 patients with CML not reaching cytogenetic or molecular remission after imatinib treatment. P = not significant for comparison of IFN-α secretion between healthy donors and patients with CML in complete cytogenetic or molecular remission after imatinib treatment. Control conditions that were not stimulated with HSV did not contain detectable or significant amounts of IFN-α.
Imatinib restores PDC function in vivo. (A) PBMCs isolated from healthy volunteers or patients with CML treated with imatinib were analyzed by flow cytometry after 3-color staining with a combination of FITC-labeled monoclonal antibodies against lineage markers (CD3, CD14, CD16, CD19, and CD56), phycoerythrin (PE)-labeled anti-CD11c and phycoerythrin-cyanin 5.1 (PC5)-labeled anti-ILT3. Two distinct populations of lin-/ILT3+ cells were observed with respect to the expression of CD11c with the phenotypes of lin-/CD11c+/ILT3+ (myeloid DCs) and lin-/CD11c-/ILT3+ (PDCs). Examples of results obtained from more than 15 healthy volunteers (left panel), 7 patients with CML in complete cytogenetic or molecular remission after imatinib treatment (middle panel), and 2 patients with CML not reaching cytogenetic or molecular remission after imatinib treatment (right panel). P = not significant for comparison of PDC numbers between healthy donors (left panel) and patients with CML in complete cytogenetic or molecular remission after imatinib treatment (middle panel). Percentages in upper left quadrants denote PDCs; in upper right quadrants, myeloid DCs. (B) IFN-α secretion by PDCs from healthy donors and patients with CML receiving imatinib treatment following stimulation with HSV. Cells were stimulated with HSV without any additional cytokine. Supernatants were harvested after 48 hours of stimulation. IFN-α secretion was analyzed by ELISA. Concentrations obtained from 104 PDCs are represented as the mean and SEM of IFN-α secretion obtained from 5 healthy donors, 5 patients with CML in complete cytogenetic or molecular remission after imatinib treatment, and 2 patients with CML not reaching cytogenetic or molecular remission after imatinib treatment. P = not significant for comparison of IFN-α secretion between healthy donors and patients with CML in complete cytogenetic or molecular remission after imatinib treatment. Control conditions that were not stimulated with HSV did not contain detectable or significant amounts of IFN-α.
Potential consequences pertaining to both PDC physiology and CML therapy can arise from the previous observations. “Dendritopoiesis” in CML is likely to be affected by the leukemic process9,10,19 that induces a marked expansion of granulopoietic progenitors to the detriment of other populations, especially DCs. Flt3L was shown to drive PDC development both in vitro and in vivo.11,20 The effect of imatinib on Flt3 expression and PDC development correlates with data showing that Flt3+ hematopoietic progenitors have DC developmental potential, whereas Flt3-fractions do not.21,22 However, it remains uncertain whether Flt3 expression and signaling is mandatory for all DC subset development, because Flt3-monocytes, for example, generate DCs in vitro and likely in vivo.23 Thus, the PDC/CML/imatinib model might represent a valuable tool to test whether overexpression or stimulation of Flt3 or other cytokine receptors can “rescue” progenitors to the DC lineage that normally have lost DC developmental potential. On the therapeutic level, in addition to inhibition of BCR-ABL activity, our findings provide some evidence that response to imatinib is accompanied by restoration of important DC-related immune functions in CML. It is yet still unclear whether imatinib can completely eliminate malignant CML primitive progenitors, abrogating the risk of disease relapse.24 However, in addition to its beneficial action on the attachment of CML cells to bone marrow stroma,25 although the exact role of PDCs in antitumor immunity has yet to be established, reconstitution of the DC system after response to imatinib might be beneficial for long-term disease control.6
Prepublished online as Blood First Edition Paper, January 8, 2004; DOI 10.1182/blood-2003-09-3220.
Supported by grants from the Association Sang pour Cent la Vie (Paris, France), from the Ligue Départementale contre le Cancer du Gard (Nimes, France), and the Association Méditerranéenne pour le Développement de la Transplantation (AMDT; Marseille, France).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank J. Wolfers (Immunotech, Beckman-Coulter, Marseille) for kindly providing the ILT3 mAb. We thank F. Brière (Schering-Plough Laboratory for Immunological Research, Dardilly, France) and L. Galibert (AMGEN, Seattle, WA) for critical reading of the manuscript. We thank D. Maraninchi and C. Mawas (Institut Paoli-Calmettes and INSERM U119, Marseille) for their continuous support. We also thank the Association pour la Recherche sur le Cancer (ARC), the Ligue Nationale contre le Cancer and the GEFLUC for their generous and continuous support for our ongoing work.