Abstract
Older adults with AML have a poor prognosis as a result of clinical characteristics and disease biology, including chemotherapy resistance. When older adults are treated with standard anthracycline-based remission induction therapy dosed by body surface area, the efficacy and toxicity of therapy may differ due to altered pharmacokinetics, metabolism, and clearance compared to younger patients. This may be reflected in the WBC nadir following therapy. Risk group stratification using pretreatment characteristics can be improved by incorporating parameters of early response to therapy for the prediction of outcome. The prognostic impact of time to WBC nadir and of the absolute WBC nadir value, both of which can be more readily assessed than bone marrow (BM) blast clearance, has not yet been determined. We present updated data on 123 older adults (age ≥55 years) diagnosed with AML and treated with anthracycline-based remission induction chemotherapy from 1994 to 2002 at the Cleveland Clinic Foundation. Time to nadir WBC and absolute WBC nadir value were assessed by univariable and multivariate analyses, controlling for cytogenetics, baseline WBC count, history of bone marrow disease, and reinduction. Survival tree methodology was used to define optimal nadir WBC groups and time to nadir WBC. Three nadir WBC groups were identified: <0.05×10³/μL (low), 0.05–0.11×10³/μL (medium), and > 0.11×10³/μL (high). Time to nadir WBC was defined as <10 days or >10 days after the start of chemotherapy. Pretreatment characteristics were typical of other studies in older adults with AML: the median age was 69 years (range 55–81), 54.5% were male, 31.1% had secondary AML, and the median WBC at presentation was 10.6 × 10³/μL. Cytogenetics (available in 87.8%) were classified as favorable, intermediate, and unfavorable based on CALGB 8461 in 4.6%, 60.2% and 35.2%, respectively. The median time to WBC nadir was 19 days (range 6–50) and the median absolute WBC nadir was 0.12×10³/μL (range 0.02–1.13). The median overall survival was 6.9 months. The complete remission (CR) rate was 50.8%, 27% of patients had resistant leukemia, and 4.9% had early death.
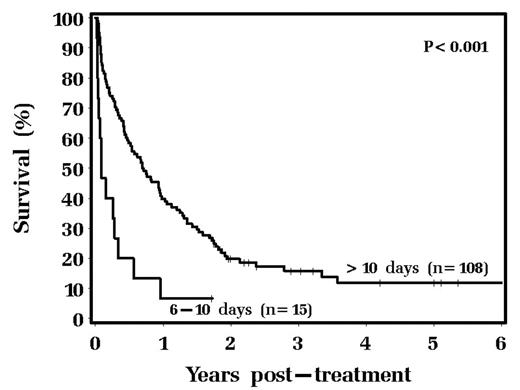
In univariable analysis, time to nadir WBC of ≤10 days was significantly associated with worse survival (Hazard Ratio (HR) 3.01, p<0.001, see figure) and both low and high nadir WBC values correlated with decreased survival when compared to medium (HR 2.2, p=0.031 and HR 1.47, p=0.08, respectively). In multivariate analysis, time to nadir WBC remained predictive (HR=2.36, p=0.008) as did WBC nadir value (HR 3.09, p=0.008 for low nadir and HR 1.62, p=0.05 for high nadir value).
In conclusion time to WBC nadir and absolute WBC nadir are useful, independent, and easily obtainable prognostic factors in older adults and may help stratify patients for eligibility for further chemotherapy.
Author notes
Corresponding author