Abstract
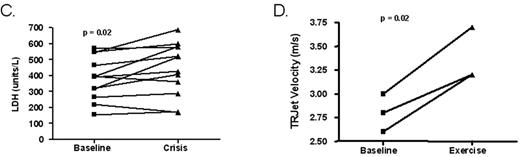
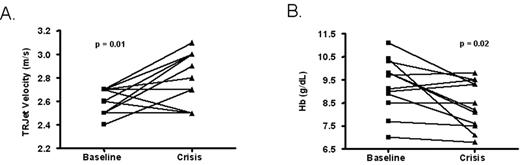
Secondary pulmonary hypertension (PHT), defined as a tricuspid regurgitant jet velocity (TRV) > 2.4 meters/second at rest, has been identified as an emerging complication in patients with sickle cell disease, with 32% prevalence. Patients with sickle cell pulmonary hypertension tend to have a higher mortality rate than patients with primary PHT at comparable pulmonary artery pressures (PAP). We analyzed prospectively obtained Doppler echocardiography measurements from 11 patients in steady-state and during vaso-occlusive crisis episodes or during exercise to determine whether pulmonary pressures became further elevated during stress. We found that tricuspid regurgitant jet velocity is significantly further elevated during vaso-occlusive crisis (2.61 ± 0.03 vs. 2.81 ± 0.06 m/sec (mean ± SEM), p = 0.01)(Fig. A). We assessed other laboratory parameters and found associated significant decreases in hemoglobin concentration (9.3 ± 0.3 vs. 8.4 ± 0.3 gm/dL, p = 0.02)(Fig. B), and significant elevations in lactate dehydrogenase (381 ± 39 vs. 442 ± 49 IU/L, p = 0.02)(Fig. C). These data are consistent with increased hemolysis during vaso-occlusive crisis, and the association of increased hemolysis with acute exacerbation of PHT in patients with SCD. In three patients at steady state, exercise echocardiograms were performed, showing acute marked rise in TRV during exercise (2.80 ± 0.12 vs. 3.37 ± 0.17 m/sec, p = 0.02)(Fig. D). These data bring to light several important points in the clinical assessment of tricuspid regurgitant jet velocity in patients with sickle cell disease. First, the relatively mild steady state PHT in patients with SCD is associated with previously unappreciated acute increases in PAP that may explain the high mortality rate in this population. This might be responsible for sudden death occurring during vaso-occlusive crisis or physical exertion. Second, this acute rise is associated with markers of increased hemolysis, further implicating hemolysis-associated derangement of nitric oxide homeostasis, endothelial function and PHT. Third, exercise measurements of TRV may be indicated in the clinical evaluation of patients with SCD and dyspnea on exertion, since it may unmask otherwise unappreciated PHT.
Author notes
Corresponding author