Abstract
Background: Cancer is associated with thrombosis, but the frequency of thromboembolism in hospitalized cancer patients receiving contemporary chemotherapy regimens is not known. We investigated the frequency of arterial and venous thromboembolism in hospitalized cancer patients receiving active therapy (as identified by the presence of neutropenia) and characterized its association with in-hospital mortality.
Methods: We conducted a retrospective cohort study using the discharge database of the University HealthSystem Consortium. This included 66,106 adult neutropenic cancer patients with 88,074 hospitalizations between 1995 and 2002 at 115 academic medical centers. Patients were identified using ICD-9-CM codes that contained at least one diagnosis of malignant disease and agranulocytosis. Patients with thromboembolism were identified using codes for venous thrombosis, pulmonary embolism, arterial embolism, acute cerebrovascular disease, and acute coronary arterial disease. The association of VTE with clinical variables was studied in univariate analysis and in a multivariate logistic regression model. The chi-square test was used to compare categorical variables, and Cochran-Armitage test to determine trend.
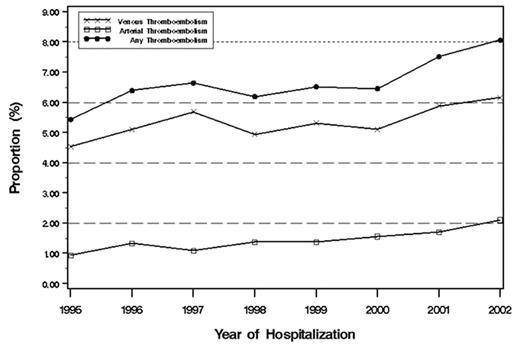
Results: Thromboembolism was reported in 5,272 patients (8%), with 5.4% patients developing venous and 1.5% arterial thromboembolism during the first hospitalization. There was a significant association between the occurrence of venous and arterial thromboembolism (OR 1.73, 95%CI, 1.38–2.16). Venous thromboembolism was more frequent in patients with metastatic disease (OR, 1.23, 95% CI 1.13–1.34), but arterial thromboembolism was not (OR, 0.59, 95% CI, 0.51–0.69). In-hospital mortality was significantly greater in patients with venous (OR 2.01, 95% CI 1.83– 2.22) or arterial thromboembolism (OR 5.04, 95% CI, 4.38–5.79), even in patients without metastatic disease. Patients with lymphoma or leukemia accounted for one-third of venous events and one-half of arterial events. Clinical variables most frequently associated with thromboembolism in a multivariate logistic regression analysis were age ≥ 65 years, primary sites of cancer including lung, gastrointestinal, gynecologic and brain, length of stay ≥ 10 days, and comorbidities including infection, pulmonary and renal disease, and obesity. From 1995 to 2002, there was a 36% increase in venous and a 124 % increase in arterial events (P for trend <0.0001) (see Figure).
Conclusions: The incidence of thromboembolism is high across all cancer subgroups including patients with hematologic malignancies and with non-metastatic disease, commonly perceived to be at lower risk for thromboembolism. Of particular concern is the increasing frequency of venous and arterial thromboembolism. Prospective studies are necessary to characterize the risks and benefits of thromboprophylaxis in this patient population.
Author notes
Corresponding author