Abstract
INTRODUCTION: Blood substitutes can alleviate problems related to blood typing and blood availability in civilian and combat trauma casualties. The aim of this study was to assess the effect of transfusions of a blood substitute, HBOC-201 (Biopure Corp, Cambridge, MA) (HBOC), as a resuscitation fluid in severe controlled hemorrhagic shock (HS).
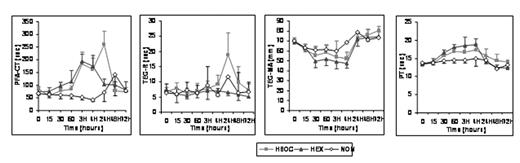
METHODS: Yucatan pigs underwent a 55% EBV controlled hemorrhage by catheter withdrawal. Animals (n=24) were either non-resuscitated (NON) or resuscitated with HBOC or with buffered hydroxyethyl starch (HEX) at an initial rate of 10 ml/kg. Additional infusions were given at 5 ml/kg if hypotension or tachycardia persisted during the 4 hr period following HS. Thereafter, animals received simulated hospital care up to 72 hr with access to blood transfusions for Hb < 7g/dl. In-vivo parameters (vital signs and in vivo bleeding time (BT)), as well as coagulation (PT, PTT, fibrinogen), thromboelastography (TEG) and in vitro bleeding time (PFA-CT) were assayed on blood samples obtained at various times after HS.
RESULTS: Although not statistically significant, HBOC allowed 100% survival compared to 75% with HEX and 25% for NON. It also restored the mean arterial pressure more rapidly compared to HEX. HBOC and HEX groups received similar resuscitation fluid volumes and showed similar hemodilution during the prehospital phase with comparable BT. PFA-CT increased abruptly for both groups remaining elevated at 24 h for HBOC. Other hemostasis parameters were better controlled in the HBOC group compared to HEX: TEG-MA was less suppressed and PT was lower with HBOC. TEG-R was unchanged but indicated delayed hypocoagulation in the HBOC group by 24 hr. At simulated hospital arrival 4 hr after HS, only 10% of animals in the HBOC group required blood transfusions compared to 100% in HEX group. By 72 hr most hematological parameters returned to normal.
CONCLUSIONS: Although HBOC-201 caused less coagulopathy than HEX during fluid resuscitation, it resulted in mild, delayed, and transient coagulopathy by 24 hr. Moreover, HBOC-201 reduced blood transfusion requirements, supporting use of this oxygen-carrying fluid for hemorrhagic shock.
The opinions contained herein are the ones of the authors and are not to be construed as official or reflecting the views of the Navy department or the naval service at large.
Author notes
Corresponding author