Abstract
Purpose: Few recent studies have examined approaches to transfusion practice in high-risk patients. We therefore documented practice variation following repair of hip fracture or cardiac surgery, as well as those requiring intensive care following a surgical intervention or multiple trauma.
Methods: We documented rates of red cell transfusion in 41,568 patients admitted to 11 hospitals across Canada between August 1998 and August 2000 as part of a retrospective observational cohort study. Adjusted odds of transfusion, median number of transfusions per patient and median number of transfusions per patient day were compared across sites. We also compared mean nadir hemoglobin concentrations from center to center in the subgroup of 7,552 patients that received red cells.
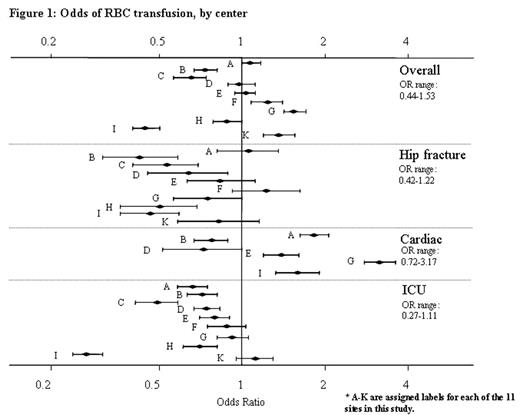
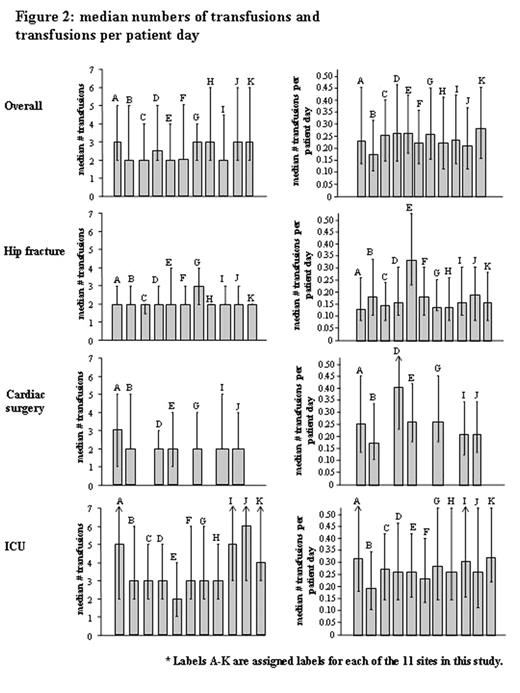
Results: The overall rate of red cell transfusion was 38.7 %, and ranged from 23.8% to 51.9% across centers among the 41,568 peri-operative and critically ill patients. Women were more likely to be transfused (43.7% versus 35.3%, p<0.0001), with higher rates of transfusion in 8 of 11 centers. Following adjustment for the effects of age, gender, severity of illness and the presence of twelve different comorbidities, the odds of transfusion ranged from 0.44 to 1.53 overall, from 0.42 to 1.22 in patients undergoing a hip fracture repair, from 0.72 to 3.17 in cardiac surgical patients undergoing cardiac surgery, and from 0.27 to 1.11 in critically ill and trauma patients (figure 1). Examination of both median number of units transfused and median number of units transfused per patient day also revealed between-site variation (figure 2). In the 7,552 transfused patients, the mean adjusted nadir hemoglobin was 74.0±4.83g/L overall, and ranged from 66.9±1.7g/L to 84.5±1.6g/L across centers. Similar differences among centers were observed amongst hip fracture patients (71.2±2.9g/L to 82.8±1.7g/L), cardiac surgical patients (65.7±1.1g/L to 77.3±1.0g/L) and critically ill and trauma patients (66.1±3.04g/L to 87.5±2.5g/L).
Conclusions: We noted significant differences in the rates of red cell transfusion and nadir hemoglobin concentrations in various surgical and critical care settings. Such variation provides the impetus for investigators to explore its potential causes, and furthermore to attempt to define optimal transfusion practice in a variety of clinical settings by conducting randomized controlled trials.
Author notes
Corresponding author