Abstract
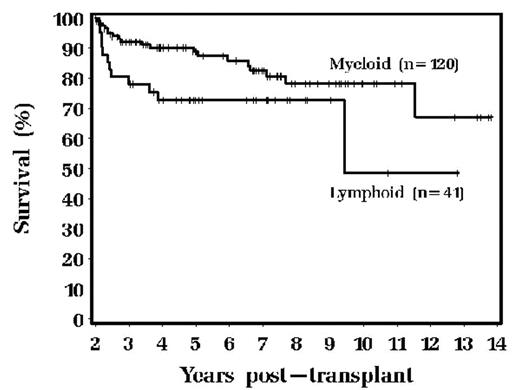
We have previously demonstrated the value of evaluating patients with NHL undergoing autologous HSCT at 2 years post-transplant; high grade lymphoma patients in CCR 2 years post-transplant are cured, whereas patients with intermediate and low grade histologies are at ongoing risk of relapse. We elected to perform a similar analysis of AHSCT patients. We retrospectively reviewed 161 consecutive AHSCT recipients who had a minimum of 2 years follow-up and who were alive 2 years post AHSCT. Patients received their transplants from 7/1988 to 7/2002. Median age was 36 years; 75% had myeloid malignancies and 25% lymphoid; AML was the most common diagnosis (39%) followed by CML (29%), ALL (14%), NHL (10%), MDS (6%), and myeloma (2%). 98% received bone marrow alone as the hematopoietic stem cell source; 98% received a busulfan/cyclophosphamide-based preparative regimen. 129 (80%) had a matched related donor. Of those patients alive 2 years post AHSCT, 31 patients (19%) have subsequently died, with a median follow up of 6 years. Relapse was the cause of death in 29%; GVHD in 35%; secondary malignancy in 7%; infections in 16%. Patients with myeloid malignancies faired better than those transplanted with lymphoid malignancies, as shown below; (p= 0.04)
When we analyzed the pts who developed their first episode of any chronic GVHD or extensive chronic GVHD there were no significant differences between lymphoid and myeloid malignacy patients. Patients receiving a matched sibling donor transplant did not have a plateau in their survival curve, and it continued to inexorably decline. Patients receiving a matched unrelated donor transplant did have a plateau of their survival curve if patients survived at least 3 years (p=0.03). We conclude that the significant majority of patients alive after AHSCT do well with extended follow-up. The graft vs. tumor effect appears to be more robust in myeloid malignancies as compared to lymphoid malignancies. Although most of these patients do well with extended follow-up, the lack of a plateau in the survival curve for patients receiving a matched sibling donor allogeneic BMT warrants additional study.
Author notes
Corresponding author