Abstract
Glucocorticoids promote thymocyte apoptosis and modulate transcription of numerous genes. GILZ (glucocorticoid-induced leucine zipper), being one of them, is strongly up-regulated in the thymus. To elucidate its function we generated transgenic mice overexpressing it specifically in the T-cell lineage and characterized its influence on thymus function. In young adult transgenic mice CD4+CD8+ thymocyte number was significantly decreased and ex vivo thymocyte apoptosis was increased. Apoptotic pathway analysis detected reduced antiapoptotic B-cell leukemia XL (Bcl-xL) expression and increased activation of caspase-8 and caspase-3. Time-course experiments showed that in wild-type (WT) thymocytes GILZ up-regulation was followed by sequential Bcl-xL decreased expression and activation of caspase-8 and of caspase-3. Moreover, GILZ delivered inside WT thymocytes by a fusion protein with the transactivator of transcription (TAT) peptide decreased Bcl-xL and promoted their apoptosis. In aged mice perturbation of thymic subset numbers was amplified over time, as demonstrated by a further decrease in CD4+CD8+ cells and increases in CD4+CD8-, CD4-CD8-, and CD8+CD4- cell counts. These results support the hypothesis that GILZ participates in the regulation of thymocyte apoptosis by glucocorticoids. (Blood. 2004;104:4134-4141)
Introduction
Glucocorticoids (GCs) are hormones and drugs that express their functions by binding and activating their specific intracellular receptor (GR), thus acting through genomic and nongenomic mechanisms. The thymus, one of their target organs, promotes thymocyte maturation to functional CD4+ or CD8+ single positive (SP) T lymphocytes that are ready to migrate to the periphery. T-cell development in the thymus is ordered by sequential steps that involve waves of cell proliferation and apoptosis. Apoptosis is a key process in thymus physiology and is triggered in 3 well-known ways: (1) negative selection, involving 5% of all thymocytes, eliminates autoreactive T-cell clones at the level of CD4+CD8+ double-positive (DP) cells; (2) death by neglect involves 90% of DP thymocytes that are neither positively nor negatively selected; and (3) stress-induced cell death.1
GCs promote apoptosis of DP thymocytes2 but are not involved in apoptosis by negative selection.3 Their role in apoptosis by neglect is uncertain, but they certainly mediate stress-induced apoptosis.1 The apoptotic signaling pathway triggered by the synthetic GC dexamethasone (DEX) in thymocytes has recently been clarified to some extent. The GC receptor coordinates activation of gene transcription and caspase-8, -9, and -3 in a sequence that leads to thymocyte apoptosis.4-7
Additionally, GC-mediated thymic apoptosis is regulated by many different molecules, and the B-cell leukemia 2 (Bcl-2) family of proteins is a critical regulator of apoptosis.8 The family is subdivided into antiapoptotic members such as Bcl-2 and Bcl-xL, and proapoptotic members such as Bcl-2-associated X protein (Bax) and BCL-2 homologous antagonist/killer (Bak) and the group of Bcl-2 homology 3 (BH3)-only death proteins.9 Specifically, Bcl-xL is expressed in the thymus only in DP cells10 and is essential for their function.11 In the current model of GC-induced cell death, therefore, the GR, by binding to DNA, up-regulates expression of unknown proteins, which, in turn, influences the balance of Bcl-2 family members resulting in activation of different caspases.2
GILZ (glucocorticoid-induced leucine zipper), one of several genes that are transcriptionally induced by GC-GR binding, was discovered in thymocytes committed to die as a consequence of DEX treatment. Its expression is up-regulated prominently in lymphoid organs.12 Interestingly, GILZ expression is reported to be induced in the kidney,13 in pluripotent mesenchymal cells,14,15 and by GCs in erythroid progenitors,16 thus suggesting GILZ plays a role not only in the immune system but also in several other physiologic systems.
Within the immune system GILZ is strongly up-regulated by GC in the thymus, particularly, and in the bone marrow, spleen, and lymph nodes.12 Expressed in resting B lymphocytes, it is down-regulated when they are activated17 ; in macrophages GC and interleukin 10 (IL-10) up-regulate it.18,19
In thymic hybridoma cells, GILZ expression selectively protects from activation-induced cell death, as triggered by anti-CD3 monoclonal antibody (mAb) but not from apoptosis induced by other apoptotic stimuli.12 Moreover, GILZ inhibits T-cell receptor-induced IL-2/IL-2 receptor expression and nuclear factor κB (NF-κB) activity, by blocking nuclear translocation and DNA binding through a direct protein-to-protein GILZ/NF-κB interaction.20 GILZ-mediated inhibition of Fas/FasL-dependent apoptosis may be explained in part by its inhibition of NF-κB. The role of GILZ overexpression in cell death in the absence of apoptogenic stimuli has not yet been evaluated. GILZ is hypothesized to play a role in regulating T-cell activation because its expression is down-regulated by T-cell receptor (TCR) triggering.20 It inhibits the mitogen-activated protein kinase (MAPK) pathway by binding to RNA polymerase-activating factor-1 (Raf-1),21 and directly binds and inhibits activator protein 1 (AP-1).22
Up to now, as the function of GILZ in the thymus has been analyzed only in in vitro experimental systems, there is a lack of information about its physiologic and/or pathologic role that can only be obtained from in vivo studies. Transgenic (TG) mice, with transgene expression limited to the T-cell lineage, constitute an excellent in vivo model for investigating the influence of a molecule in the thymus.
In this study, we produced TG mice in which murine GILZ is controlled by the T-cell-specific human CD2 (hCD2) promoter and enhancer that program T-cell-specific transgene expression and are expressed at high levels in all thymocyte subsets, including double negative (CD4-CD8-, DN), DP, and CD4+ or CD8+ SP cells.23 Results indicate that GILZ increased the apoptosis rate of thymocytes and decreased Bcl-xL expression. Increased apoptosis correlates with changes in thymocytes and is associated with altered T-lymphocyte subpopulation counts.
Materials and methods
Generation of TG mice
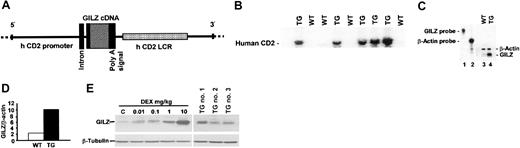
The transgene construct was made by cloning 874-base pair (bp) cDNA fragment containing the full open reading frame (ORF) of GILZ into the hCD2 expression vector (Figure 1A). The construct was injected into fertilized mouse embryos, and the generation of TG mice (DBA × C57BL/6) was tested by Southern blot analysis of their tail genomic DNA (Figure 1B). TG mice were backcrossed to C57BL/6 mice 8 generations, and TG mice were compared with WT littermates in the same experiments. Two independent transgenic lines were produced.
Generation and analyses of TG mice. (A) Construct used for embryo injection. (B) Southern blot from tails of generated mice. Bands (human CD2) indicate the construct integrated in the DNA of TG mice (TG). Bands are absent in wild-type mice (WT). (C) mRNA evaluated by ribonuclease protection assay (RPA). GILZ mRNA levels were analyzed in thymocytes from WT (lane 3) or TG (lane 4) mice. GILZ or β-actin probes are shown in lanes 1 and 2, respectively. (D) Quantitative analysis of RPA experiment shown in panel C. (E) Western blot of GILZ protein levels in thymocytes from WT mice left untreated (control, C; lane 1) or treated with 0.01, 0.1, 1, or 10 mg/kg DEX (lanes 2, 3, 4, and 5, respectively) or in thymocytes from 3 TG mice (TG no. 1, TG no. 2, TG no. 3).
Generation and analyses of TG mice. (A) Construct used for embryo injection. (B) Southern blot from tails of generated mice. Bands (human CD2) indicate the construct integrated in the DNA of TG mice (TG). Bands are absent in wild-type mice (WT). (C) mRNA evaluated by ribonuclease protection assay (RPA). GILZ mRNA levels were analyzed in thymocytes from WT (lane 3) or TG (lane 4) mice. GILZ or β-actin probes are shown in lanes 1 and 2, respectively. (D) Quantitative analysis of RPA experiment shown in panel C. (E) Western blot of GILZ protein levels in thymocytes from WT mice left untreated (control, C; lane 1) or treated with 0.01, 0.1, 1, or 10 mg/kg DEX (lanes 2, 3, 4, and 5, respectively) or in thymocytes from 3 TG mice (TG no. 1, TG no. 2, TG no. 3).
Cell harvesting and cell culture
Thymi were weighed, and the cells were counted with a hemocytometer. Single thymocyte suspensions were cultured in RPMI 1640 medium containing 5% fetal calf serum (FCS), 100 U/mL penicillin/streptomycin, 0.1 mM nonessential amino acids, 5.5 × 102 μM β-mercaptoethanol (β-ME; GIBCO Invitrogen, San Giuliano Milanese, Italy) in flat-bottomed, 96-well plates (Costar, Cambridge, MA).
RPA
Total RNA was extracted using TRIzol (GIBCO Invitrogen). The assay was performed using the RPA III kit (Ambion, Austin, TX). Total RNA was hybridized with GILZ and the β-actin antisense probe. Samples were processed according to the manufacturer's instructions and loaded on to a 6% polyacrylamide/8 M urea denaturing gel. Autoradiographic exposure was carried out using a PhosphorImager (Molecular Dynamics, Sunnyvale, CA). To evaluate Bcl-2 family member mRNA expression, an mAPO-2 multiprobe template set from Pharmingen (San Diego, CA) was used.
Western blot analysis
Total proteins were separated on a 12% or 15% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE). Primary Abs were rabbit polyclonal antiserum anti-GILZ, anti-caspase-8 (Santa Cruz Biotechnology, Santa Cruz, CA), anti-caspase-3, anti-caspase-9 (Cell Signaling Technology, Beverly, MA), anti-Bcl-xL (R&D Systems, Minneapolis, MN), anti-β-tubulin mAbs (Sigma, St Louis, MO) and anti-glutathione S-transferase (GST) mAb (Amersham, Buckinghamshire, United Kingdom). Secondary Abs were horseradish peroxidase-labeled goat anti-rabbit or anti-mouse (Pierce, Rockford, IL).
Flow cytometry analysis
The following mAbs were used: fluorescein isothiocyanate (FITC)-conjugated rat anti-mouse CD8a (clone 53-6.7), Cy-Chrome anti-mouse CD8a (clone 53-6.7), phycoerythrin (PE)-conjugated rat anti-mouse CD4 (clone H129.19), and FITC-conjugated hamster anti-CD3 (clone 145-2C11). All mAbs and their isotype controls were purchased from Pharmingen (San Diego, CA).
Apoptosis evaluation
Apoptosis was evaluated by TUNEL (transferase-mediated deoxyuridine triphosphate [dUTP] nick end labeling) technology using an In Situ Cell Death Detection Kit (Roche Diagnostics, Mannheim, Germany). Briefly, cells (2 × 106/mL) were washed in phosphate-buffered saline (PBS) and fixed in 4% formaldehyde for 60 minutes at room temperature (RT), washed again, and incubated on ice for 2 minutes with the permeabilization solution (0.1% Triton X-100 in 0.1% sodium citrate). Cells were then stained by incubating them with 50 μL TUNEL reaction mixture for 60 minutes at 37°C. Cells were analyzed by flow cytometry.
Apoptosis was also measured by flow cytometry. After 24 hours of culture, cells were centrifuged, and the pellets were gently resuspended in 1.5 mL hypotonic propidium iodide (PI) solution (50 μg/mL in 0.1% sodium citrate plus 0.1% Triton X-100). The tubes were kept in the dark at 4°C for 1 hour. The PI fluorescence of individual nuclei was measured by flow cytometry using standard FACScan equipment (Becton Dickinson, Franklin Lakes, NJ). The nuclei traversed a 488-nm Argon laser light beam. A 560-nm dichroid mirror and a 600-nm band pass filter (band width 35 nm) were used to collect the red fluorescence because of PI DNA staining. The data were recorded in logarithmic scale in a Hewlett Packard (HP 9000, model 310; Palo Alto, CA) computer. The percentage of apoptotic cell nuclei (subdiploid DNA peak in the DNA fluorescence histogram) was calculated with specific FACScan research software (Lysis II).
Δψm measurement
The thymocyte suspension was incubated in complete medium with 10 μg/mL JC-1 for 10 minutes in the dark at RT. Cells were then washed, resuspended in 400 μL, and analyzed by flow cytometry. JC-1 was from Molecular Probes (Eugene, OR)
TAT fusion proteins
The GILZ-GST-TAT expression vector was constructed by inserting GILZ cDNA in the TAT-C vector to produce an in-frame fusion protein. Fusion protein were purified as previously described.12
[3H]-Thymidine incorporation assay
[3H]-thymidine (2.5 μCi [0.0925 MBq]) per well was added 15 hours before harvesting cells. Cells were collected with a multiple suction-filtration apparatus (Mash II) on a fiberglass filter (Whittaker, Walkersville, MD) and counted in a β counter (Packard, Milan, Italy).
Statistical analysis
Data are presented as the mean ± 1 standard error of the mean (SEM). Student t test was calculated for all suitable experiments. Values with P greater than .05 were not considered significantly different (*P < .05, **P < .005, ***P < .0005).
Results
Expression of GILZ mRNA and protein in TG mice
Generation of TG mice was tested and confirmed by Southern blot of DNA extracted from their tail (Figure 1A,-B and “Materials and methods”).
GILZ expression in the thymus was determined by using the RPA and Western blot analysis on TG and WT thymocytes to assess the amount of GILZ mRNA and protein, respectively. Basal levels of GILZ mRNA were about 5-fold higher in TG than in WT thymocytes, as shown by the quantitative analysis (Figure 1D) of a representative RPA (Figure 1C).
Western blots showed protein levels (Figure 1E) were higher in the thymus of TG than in WT mice. GILZ overexpression was compared in TG and in WT thymocytes from mice that were left untreated or treated with different doses of DEX in dose-response experiments. As shown in Figure 1E, thymic GILZ protein levels in 3 TG mice were higher than in untreated WT control mice (in which the protein was barely detectable) and were similar to levels in WT mice treated with 0.1 to 1 mg/kg DEX. To prevent confounding effects which could be due to genetic differences (other than the transgene) between the TG and WT mice, TG mice were backcrossed to C57BL/6 mice 8 generations, and single experiments were performed comparing TG and WT littermates.
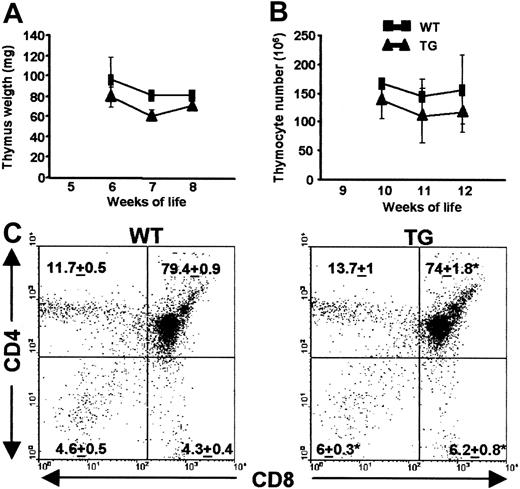
Phenotypic analyses of freshly isolated thymi
To determine whether T-cell development was influenced by constitutive GILZ overexpression, thymi from TG and WT animals were weighed, total thymocytes were counted by hemocytometer, and thymocyte subsets were analyzed by flow cytometry using mAbs specific for CD4 and CD8 T-cell surface antigens. As shown in Figure 2A, in young adult mice, thymus weight was not significantly different in TG or WT mice. Figure 2B shows the total thymocyte count from young adult TG mice was not significantly different than in controls.
Phenotype of thymus from WT and TG mice. (A) Thymus weights of 6-, 7-, or 8-week-old WT (▪) or TG(▴) female mice are reported as the mean values ± 1 SEM. (B) Thymocyte number in 10-, 11-, or 12-week-old female mice are reported as the mean values ± 1 SEM. (C) CD4 and CD8 2-color flow cytometry analysis. Representative dot plot panels of thymocyte subsets from 8-week-old WT or TG mice are shown. Numbers represent the mean ± 1 SEM from 10 independent experiments.
Phenotype of thymus from WT and TG mice. (A) Thymus weights of 6-, 7-, or 8-week-old WT (▪) or TG(▴) female mice are reported as the mean values ± 1 SEM. (B) Thymocyte number in 10-, 11-, or 12-week-old female mice are reported as the mean values ± 1 SEM. (C) CD4 and CD8 2-color flow cytometry analysis. Representative dot plot panels of thymocyte subsets from 8-week-old WT or TG mice are shown. Numbers represent the mean ± 1 SEM from 10 independent experiments.
The relative percentage of thymocyte subsets was analyzed by 2-color flow cytometry. Figure 2C shows there was a significant (P < .05) decrease in DP (from 79.4% ± 0.9% to 74% ± 1.8%), and a parallel consistent (P < .05) increase in DN (from 4.6% ± 0.5% to 6% ± 0.3%) and CD8+ SP (from 4.3% ± 0.4% to 6.2% ± 0.8%) cells. No significant differences were detected in the relative number of the CD4+ SP subset. Thus, basal GILZ overexpression appears to perturb thymic subsets significantly in young adult TG mice.
Apoptosis of WT or TG thymocytes
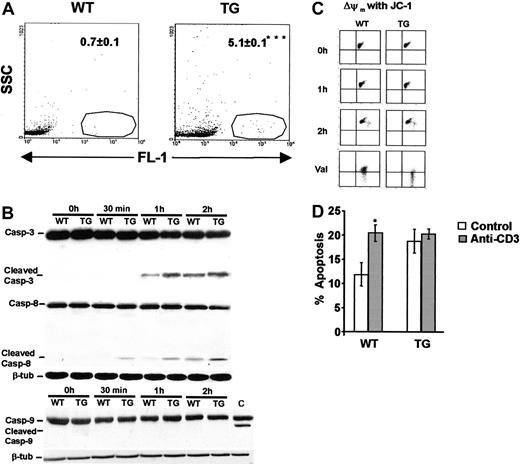
To see whether increased cell death contributed to the decrease in DP thymocytes, apoptosis was evaluated by TUNEL technology on fresh thymocytes harvested immediately after mice were killed. TUNEL technology detects apoptosis in vivo in the thymus (usually ranging from 0.5% to 1%24) before apoptotic cells are cleared by macrophages. Figure 3A shows that apoptosis of fresh thymocytes from TG was notably higher than WT control mice (from 0.7 ± 0.1 to 5.1 ± 0.1; P < .0005).
Apoptosis analyses of thymocytes from WT and TG mice. (A) Histograms show apoptosis, measured by TUNEL technology, of freshly isolated WT and TG thymocytes from a representative experiment. Numbers indicate the percentage apoptosis values from 6 independent experiments. ***P < .0005. (B) Western blot analyses of thymocytes from WT and TG mice left uncultured (0 h), or after 30 minutes, 1 hour, or 2 hours of culture. In each Western blot, bands that represent procaspase-3 or -9 are labeled “casp-3” or “casp-9,” Whereas activated forms of caspases are labeled “cleaved casp-3,” “cleaved casp-8,” or “cleaved casp-9.” respectively. In the caspase-9 panel, C indicates the positive control DEX-treated thymocytes. β-Tubulin expression for each Western blot is also reported. (C) Dot plots represent Δψm of fresh thymocytes (0 h), or thymocytes cultured for 1 or 2 hours. Dot plots labeled “val” show the positive controls (thymocytes treated with valinomycin). (D) Bars represent percentage apoptosis of thymocytes cultured with (▦) or without coated anti-CD3 mAb (□). *P < .05.
Apoptosis analyses of thymocytes from WT and TG mice. (A) Histograms show apoptosis, measured by TUNEL technology, of freshly isolated WT and TG thymocytes from a representative experiment. Numbers indicate the percentage apoptosis values from 6 independent experiments. ***P < .0005. (B) Western blot analyses of thymocytes from WT and TG mice left uncultured (0 h), or after 30 minutes, 1 hour, or 2 hours of culture. In each Western blot, bands that represent procaspase-3 or -9 are labeled “casp-3” or “casp-9,” Whereas activated forms of caspases are labeled “cleaved casp-3,” “cleaved casp-8,” or “cleaved casp-9.” respectively. In the caspase-9 panel, C indicates the positive control DEX-treated thymocytes. β-Tubulin expression for each Western blot is also reported. (C) Dot plots represent Δψm of fresh thymocytes (0 h), or thymocytes cultured for 1 or 2 hours. Dot plots labeled “val” show the positive controls (thymocytes treated with valinomycin). (D) Bars represent percentage apoptosis of thymocytes cultured with (▦) or without coated anti-CD3 mAb (□). *P < .05.
Increased apoptosis of TG thymocytes prompted us to investigate the role of the caspase cascade. Analysis was performed on cultured thymocytes because the apoptosis signaling pathway in fresh thymocytes is difficult to detect because of the in vivo apoptotic cell clearance by macrophages.24 We first examined caspase-3, which is considered one of the terminal caspases involved in DEX-induced apoptosis.5,7 After cells from TG or WT mice were harvested, 1 aliquot was taken for immediate total protein extraction, and the others were cultured for 30 minutes, 1 hour, or 2 hours before extracting the proteins to be used in Western blot experiments. Figure 3B shows that activated cleaved caspase-3 was absent in proteins from freshly isolated WT thymocytes (0 h) and after 30 minutes; its activation was detectable after 1 hour of culture but was fully evident after 2 hours of culture. In TG thymocytes caspase-3 activation, after 1 hour or 2 hours, was stronger than in WT thymocytes. Analysis of β-tubulin showed a similar protein content in WT and TG samples. So increased apoptosis in TG thymocytes correlated with augmented caspase-3 activation.
The executioner caspase-3 is activated by at least 2 different pathways. The mitochondrial pathway leads to sequential activation of caspase-8, BID, release of cytochrome c from mitochondria, and activation of caspase-9 which directly cleaves and activates caspase-3. The second pathway involves activation of caspase-8 that directly activates caspase-3.25 We analyzed both pathways to see which accelerates activation of caspase-3 in TG mice. The filters we had used to analyze caspase-3 activation by Western blot were again adopted to probe caspase-8. It was activated after 30 minutes (Figure 3B) and activation increased after 1 or 2 hours of culture. In WT thymocytes caspase-8 was weakly active only after 1 or 2 hours of culture. Western blots were performed to determine whether caspase-8 activated caspase-3 directly or through the so-called “mitochondrial pathway.” Caspase-9 activation was not detectable at any time either in TG or WT thymocytes, suggesting caspase-3 is directly activated by caspase-8.
The change in mitochondrial transmembrane potential (Δψm) is widely accepted as an index of mitochondrial activity because Δψm is involved in release of cytochrome c and the ensuing caspase-9 activation in the mitochondrial pathway. Figure 3C shows a representative experiment. Δψm, as evaluated by JC-1 flow cytometry analysis, was at the same levels in TG thymocytes and WT thymocytes after 0, 1, or 2 hours of culture, providing further evidence that in our culture system caspase-3 is not activated through the mitochondrial/caspase-9 pathway.
In vitro pull-down experiments with the fusion protein GILZ-GST demonstrated that GILZ activated caspase-8 neither by directly binding to it nor by binding to Fas-associated death domain protein (FADD), the caspase-8 recruiting molecule (not shown). However, we cannot exclude that the interactions happen in vivo.
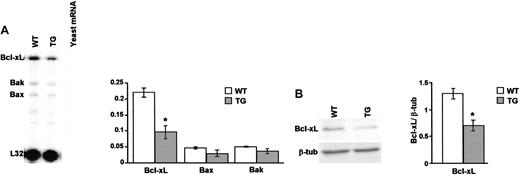
Analysis of the Bcl-2 family members in thymocytes of WT and TG mice
Caspase activation is regulated by balancing expression of antiapoptotic (Bcl-2, Bcl-xL) and proapoptotic (Bax, Bak) Bcl-2 family molecules. Bcl-xL is almost exclusively expressed in, and selectively regulates, DP but not DN or SP thymocyte apoptosis.10 With the aim of dissecting the role of Bcl-2 family, and particularly of Bcl-xL, RPA experiments with a multiprobe template kit and Western blotting were performed in WT or TG thymocytes to assess the mRNA and protein levels, respectively. Figure 4A shows a representative experiment (left) and quantitative analysis of all experiments (right). The antiapoptotic Bcl-xL mRNA levels were significantly lower in fresh thymocytes from TG mice than in controls, whereas mRNA levels of the proapoptotic Bax or Bak were unchanged. Expression of the other family molecules was too low for quantification. Low mRNA levels correlated with a parallel significant decrease in the amount of protein as shown in a representative experiment (Figure 4B, left side) and quantitative protein analysis from a series of experiments (right side). Thus, thymocytes from TG mice have a reduced Bcl-xL mRNA and protein expression which may account for increased thymocyte apoptosis.
Thymocyte Bcl-xL expression. (A) RPA analysis shows mRNA levels of Bcl-xL, Bak, and Bax from a representative experiment. Bars represent quantitative analysis of Bcl-xL (Bcl-xL/L32 mRNA ratio), Bax (Bax/L32 mRNA ratio), or Bak (Bak/L32 mRNA ratio) mRNA levels in WT and TG thymocytes from 3 independent experiments. (B) Western blot analysis of Bcl-xL (labeled “Bcl-xL”) and β-tubulin (“β-tub”) proteins and, on the right, the quantitative analysis (bcl-xL/β-tubulin ratio) of WT and TG thymocytes from 3 independent experiments. Bars represent the mean values ± 1 SEM. *P < .05.
Thymocyte Bcl-xL expression. (A) RPA analysis shows mRNA levels of Bcl-xL, Bak, and Bax from a representative experiment. Bars represent quantitative analysis of Bcl-xL (Bcl-xL/L32 mRNA ratio), Bax (Bax/L32 mRNA ratio), or Bak (Bak/L32 mRNA ratio) mRNA levels in WT and TG thymocytes from 3 independent experiments. (B) Western blot analysis of Bcl-xL (labeled “Bcl-xL”) and β-tubulin (“β-tub”) proteins and, on the right, the quantitative analysis (bcl-xL/β-tubulin ratio) of WT and TG thymocytes from 3 independent experiments. Bars represent the mean values ± 1 SEM. *P < .05.
Correlation between GILZ and Bcl-xL expression in time-course experiments on WT and TG thymocytes
During the course of this study, we observed that cultured thymocytes induced GILZ expression even in WT cells with their very low or undetectable basal GILZ expression. Expression induction by cell culture is a known property of some molecules because also serum- and glucocorticoid-regulated kinase 1 (SGK-1) is induced by glucocorticoids and by culture serum.26 We exploited this feature to correlate GILZ and Bcl-xL expression and caspase-8 and -3 activation in time-course experiments by culturing aliquots of WT or TG thymocytes for 30 minutes, 1 hour, or 2 hours before extracting the RNA or proteins to be used in RPA or Western blot experiments, respectively. Figure 5A shows very low GILZ expression in proteins from freshly isolated WT thymocytes (0 h), which increased after 30 minutes, 1 hour, or 2 hours of culture; TG thymocytes showed the same phenomenon, although GILZ expression was higher. The same filters, reprobed for expression of Bcl-xL, showed a marked decrease in Bcl-xL expression in WT thymocytes starting 30 minutes after the increase in GILZ (1-hour culture). Bcl-xL expression in TG thymocytes was very low (as shown in Figure 4) in freshly isolated thymocytes and remained unchanged at all time points. In RPA (Figure 5B), Bcl-xL mRNA decreased after 1 hour of culture; the decrease was significantly stronger after 2 hours in WT thymocytes, reaching levels similar to the TG thymocytes. Bax or Bak mRNA from WT or TG thymocytes did not show any significant change with culture, thus demonstrating a specific effect on Bcl-xL expression.
Time-course experiments of cultured thymocytes. (A) Western blot analysis of GILZ (top), Bcl-xL (middle), and β-tubulin (bottom) proteins expressed in WT or TG thymocytes freshly isolated (0 h) or after 30 minutes, 1 hour, or 2 hours of culture. Data are representative of 3 independent experiments. (B) RPA analysis shows mRNA levels of Bcl-xL, Bak, and Bax of a representative experiment (left), and bars represent quantitative analysis of Bcl-xL (Bcl-xL/L32 mRNA ratio), Bax (Bax/L32 mRNA ratio), or Bak (Bak/L32 mRNA ratio) mRNA levels in WT (□) and TG (▦) uncultured thymocytes (0 h) or from thymocytes cultured for 1 or 2 hours from 3 independent experiments. (C) Apoptosis of WT (□) or TG(▦) thymocytes cultured for 24 or 48 hours. Bars represent the mean values ± 1 SEM from 10 independent experiments. *P < .05.
Time-course experiments of cultured thymocytes. (A) Western blot analysis of GILZ (top), Bcl-xL (middle), and β-tubulin (bottom) proteins expressed in WT or TG thymocytes freshly isolated (0 h) or after 30 minutes, 1 hour, or 2 hours of culture. Data are representative of 3 independent experiments. (B) RPA analysis shows mRNA levels of Bcl-xL, Bak, and Bax of a representative experiment (left), and bars represent quantitative analysis of Bcl-xL (Bcl-xL/L32 mRNA ratio), Bax (Bax/L32 mRNA ratio), or Bak (Bak/L32 mRNA ratio) mRNA levels in WT (□) and TG (▦) uncultured thymocytes (0 h) or from thymocytes cultured for 1 or 2 hours from 3 independent experiments. (C) Apoptosis of WT (□) or TG(▦) thymocytes cultured for 24 or 48 hours. Bars represent the mean values ± 1 SEM from 10 independent experiments. *P < .05.
The decrease in Bcl-xL correlated with apoptosis of WT or TG thymocytes cultured for 24 or 48 hours. As shown in Figure 5C, after 24 hours, apoptosis in TG thymocytes was still significantly higher than in WT cells, despite their Bcl-xL decreased expression, although the differences were smaller when compared with apoptosis in fresh thymocytes (compare with Figure 3). After 48 hours of culture, differences in apoptosis rates were further decreased and became nonsignificant.
To further support the correlation between GILZ, Bcl-xL, and thymocyte apoptosis, we produced a fusion protein GST-TAT-GILZ in which the transactivator of transcription (TAT) peptide pulls the fusion protein across the cell membrane, inside cells27 (Figure 6A). WT thymocytes, treated with GST-TAT-GILZ (0.2 μg/mL) showed a marked decrease in Bcl-xL protein expression after 2 hours of culture when compared with controls (Figure 6B). This was followed (after 24 hours) by a dramatic increase in apoptosis compared with the group treated with the GST-TAT control fusion protein (Figure 6C, left panel). As a control of specificity, the GST-TAT-GILZ fusion protein did not increase apoptosis of spleen cells (Figure 6C, right panel). Our controls, in agreement with previous reports,27 demonstrated that TAT fusion proteins are not toxic.
Effect of GST-TAT-GILZ fusion protein on WT thymocytes. (A) Western blot analysis of thymocyte protein untreated or treated for 30 minutes, 1 hour, or 2 hours with either GST-TAT (1) or with GST-TAT-GILZ (2), revealed with the anti-GST mAb. (B)Western blot of Bcl-xL expression on WT thymocytes untreated or treated for different times (30 minutes, 1 hour, or 2 hours) with either GST-TAT-GILZ (GILZ) or GST-TAT (TAT). (C) Bars indicate apoptosis of WT thymocytes (left) or splenocytes (right) after 24 hours of treatment with either GST-TAT (TAT; □) or GILZ-GST-TAT (GILZ; ▦). Bars represent the mean values ± 1 SEM from 3 independent experiments. *P < .05.
Effect of GST-TAT-GILZ fusion protein on WT thymocytes. (A) Western blot analysis of thymocyte protein untreated or treated for 30 minutes, 1 hour, or 2 hours with either GST-TAT (1) or with GST-TAT-GILZ (2), revealed with the anti-GST mAb. (B)Western blot of Bcl-xL expression on WT thymocytes untreated or treated for different times (30 minutes, 1 hour, or 2 hours) with either GST-TAT-GILZ (GILZ) or GST-TAT (TAT). (C) Bars indicate apoptosis of WT thymocytes (left) or splenocytes (right) after 24 hours of treatment with either GST-TAT (TAT; □) or GILZ-GST-TAT (GILZ; ▦). Bars represent the mean values ± 1 SEM from 3 independent experiments. *P < .05.
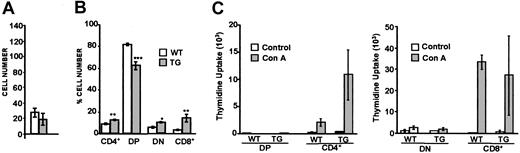
Number of thymocytes from aged mice and proliferation potential
In young adult mice, functional phenomena (namely proliferation versus apoptosis) balance thymus weight, total cell number, and small changes in the relative number of thymocyte subsets. As we wondered whether differences are amplified as mice age, elderly animals (between 18 and 20 months of age) were killed, their thymocytes counted and analyzed by flow cytometry to determine the relative number of cell subsets. Figure 7A shows no differences were seen in total thymocyte number, whereas strongly significant differences which were not seen in young adult mice appeared in subset cell numbers (Figure 7B). Specifically, the number of CD4+ SP TG thymocytes was significantly greater than WT thymocytes (9 ± 0.7 and 12.7 ± 0.6 in WT and TG, respectively); DP cells from aged TG mice were very low (81.5 ± 1.3 WT versus 62.8 ± 3.6 TG); more DN (5.7 ± 0.7 WT versus 9.9 ± 0.8) and CD8+ SP cells (3.8 ± 0.3 WT versus 14.7 ± 3.7 TG) were found in aged mice. In conclusion, phenotypic experiments in aged mice suggest age-related impairments in the thymus subsets in elderly TG mice.
Analysis of thymocytes from aged mice and proliferation potential. (A) Bars indicate the cell number of thymocytes from WT and TG mice. (B) Bars indicate the relative cell number of thymocyte subsets CD4+ SP, DP, DN, or CD8+ SP from WT (white) and TG (gray) mice. (C) Bars indicate cpm thymidine uptake of different thymocyte subsets from WT and TG mice. White or gray bars represent WT or TG mice, respectively. *P < .05; **P < .005; ***P < .0005. Analyses were performed on 15 mice. Bars show the mean ± 1 SEM.
Analysis of thymocytes from aged mice and proliferation potential. (A) Bars indicate the cell number of thymocytes from WT and TG mice. (B) Bars indicate the relative cell number of thymocyte subsets CD4+ SP, DP, DN, or CD8+ SP from WT (white) and TG (gray) mice. (C) Bars indicate cpm thymidine uptake of different thymocyte subsets from WT and TG mice. White or gray bars represent WT or TG mice, respectively. *P < .05; **P < .005; ***P < .0005. Analyses were performed on 15 mice. Bars show the mean ± 1 SEM.
Finally, the proliferation potential of thymocytes from young adult mice was tested. Aliquots of each isolated thymic subset were cultured alone or with concanavalin A (ConA) mitogen for thymidine uptake experiments and analyzed after 48 hours of culture. As shown in Figure 7C, despite the appearance of thymidine uptake greater in TG than in WT thymocytes (mean values ± 1 SEM) in the CD4+ SP cells, there was no statistical difference between the 2 samples (P > .05).
Discussion
In this study, we demonstrated that GILZ is involved in thymic apoptosis. Three experimental systems were used: (1) overexpressing-GILZ transgenic mice, (2) cultured WT thymocytes, and (3) a GILZ-TAT fusion protein. Thanks to these systems, it has been shown that GILZ promotes spontaneous thymic apoptosis (by stress and/or neglect) and inhibits apoptosis by negative selection. Moreover, analysis of the biochemical events determining spontaneous apoptosis possibly delineates an unknown pathway based on a decrease in Bcl-xL and activation of caspase-8 and -3 without involving the mitochondria. Loss of GILZ experimental systems will tell us whether the reported observations are important events in the physiology of thymus and in development of normal and autoreactive T lymphocytes.
Transgenic mice with the transgene specifically expressed in the T-cell lineage appeared to be a suitable experimental system. We chose the vector based on the hCD2 minigene,23 with the gene of interest under the control of the hCD2 promoter and locus control region. This expression vector confers 3 important features on the TG mice: (1) tissue specificity, because the gene is expressed only in the T-cell lineage (thymocytes and peripheral T lymphocytes); (2) copy dependence; and (3) position-independent expression of the gene.23,28,29 Expression studies performed by RPA and by Western blot confirmed the thymus in TG mice expressed about 5-fold more mRNA and protein than in WT mice. GILZ is strongly up-regulated by GC treatment. In our TG mice GILZ overexpression is constitutive, matching physiologic levels of expression achieved with 0.1 to 1 mg/kg DEX, a dose that causes low 15% to 20% thymocyte apoptosis (data not shown).
No significant differences were detected in thymus weight or total thymocyte number. A significant decrease in DP and increases in DN and CD8+ SP thymocytes in young adult mice were amplified with aging.
The functional analysis focused on thymocyte apoptosis. Although 95% thymocytes undergo cell death,30 apoptosis detected in vivo on fresh thymocytes is usually very low (0.5%-1%) because of continuous clearance of apoptotic cells.24,31 Our results indicate a strong increase, of up to 6%, in ex vivo thymic apoptosis, as evaluated by TUNEL, in TG mice, which was associated with an augmented activation of the caspase-8/caspase-3 pathway. This rise in apoptosis apparently contrasts with reports, indicating that GILZ inhibits apoptosis induced by anti-CD3 stimulation13,20 or IL-2 withdrawal.32 However, some molecules are known to play opposing roles in apoptosis. GCs promote thymic apoptosis but inhibit ovary apoptosis.33 Moreover, although they determine thymocyte apoptosis, they also protect thymocytes from anti-CD3-induced apoptosis, a mechanism known as mutual exclusion. Our data suggest that GILZ behaves like GCs.
The GILZ-activated caspase-8/-3 apoptotic pathway we observed strengthened the similarities with GC-induced apoptotic mechanisms. This raises the question of whether GILZ is one of the molecules that are part of the apoptotic pathway triggered by GCs in thymocytes. GILZ is transcriptionally induced by DEX and DEX triggers apoptosis by achieving gene transcription and protein synthesis.5,7 In addition, like GCs, GILZ determines apoptosis by sequential activation of caspase-8/caspase-3.7 Opinions are divergent on caspase-9 activation. Some reports claim it is crucial in DEX-induced apoptosis,6,34,35 whereas others claim it amplifies DEX-induced apoptosis after triggering by caspase-8/caspase-3 activation.7,36 We therefore speculate that GILZ is involved in the caspase-9-independent part of GC-induced thymocyte apoptosis.
Of interest, increased thymocyte apoptosis was a late event in cultured cells (24 hours), following the Bcl-xL decrease (2 hours), thus suggesting that the former event was possibly a consequence of the latter. This strongly suggests that decreased expression of Bcl-xL is limited to the DP cells, and that the increased apoptosis may be confined inside the DP subset because Bcl-xL is expressed almost exclusively in DP cells and selectively regulates their survival but does not influence the survival of SP cells.10 However, concurring with the small changes observed in our young adult TG mice, Bcl-xL down-regulation in Bcl-xL+/- and Bcl-xL-/- mice is associated with normal thymocyte and peripheral T-cell counts.10 It seems improbable that diminished Bcl-xL expression was due to fewer DPs because the DP decrease was only about 5%, whereas 50% less Bcl-xL was expressed in TG than in WT thymocytes. Furthermore, the unchanged proapoptotic Bax and Bak expression confirms the specificity of the Bcl-xL decrease. It is hardly surprising that a strong percentage decrease in Bcl-xL expression did not determine apoptosis of a similar percentage of thymocytes. In fact, it has previously been shown that in Bcl-xL+/- mice with a 50% Bcl-xL decrease, “TUNEL-positive apoptotic cells increased drastically from 1.2% to 4.3% in male fetal germ cells.”37,p210 Administration of GILZ protein in fusion with the TAT peptide strengthened the correlation with the Bcl-xL down-regulation and with the increase of apoptosis. We do not know what mechanism underlines the GILZ inhibition of Bcl-xL. Because GILZ is able to bind to the gene promoter, thus acting as a transcriptional repressor,15 it may directly repress Bcl-xL transcription. However, Bcl-xL could also be repressed indirectly as the NF-κB family directly activates Bcl-xL38 and protects from apoptosis.39 As GILZ binds and inhibits NF-κB,20 one might presume it counters both expression of Bcl-xL and its antiapoptotic effect, thus promoting apoptosis. The decrease in Bcl-xL usually triggers the mitochondrial apoptotic pathway, with release of cytochrome c in the cytoplasm and activation of caspase-9 “apoptosome.”25 In our model, decreased Bcl-xL did not correlate with caspase-9 activation, suggesting alternative “non-mitochondrial” mechanisms. For example, like Bcl-2 the antiapoptotic prototype of the family, Bcl-xL may regulate caspase activation independently of the cytochrome c/caspase-9 apoptosome.36 Alternatively, Bcl-xL may regulate activation of caspase-8 which is bound to the outer mitochondrial membrane40 or present inside the endoplasmic reticulum.41 Altered Bcl-xL expression features in many diseases such as tumors,42 disorders in the central nervous system,43 and vascular diseases.44 Specifically, Bcl-xL is overexpressed in many cancers, including different lymphomas in which it (1) increases survival of cancer cells, thus augmenting their invasive and metastatic abilities, and (2) determines resistance of cancer cells to chemotherapeutic agents. The GILZ-dependent down-regulation of Bcl-xL expression indicates GILZ may play a role in protecting cells from the tumorigenic potential of Bcl-xL overexpression45 and/or in rendering cancer cells responsive to antitumor therapies.
As we also wondered whether the dysfunctions could disrupt thymus balance over time, we analyzed thymic cells from aged mice. Although the total thymocyte count was normal, the thymic perturbation that we had observed in young TG mice was amplified in older animals: 20% fewer DP cells than in WT mice, the differences in CD8+ SP and DN counts were even greater, and an increase appeared in CD4+ SP cells. This pattern of amplified thymocyte number perturbation with aging concurs with previous reports in which a 2-fold increase Bcl-xL in thymocytes of Bcl-xL TG mice is associated with age-related abnormalities in thymic subset counts.46 Further studies of in vivo challenge of TG mice will show whether thymic impairments generate an abnormal immune response and, possibly, pathologic alterations.
In conclusion, constitutive GILZ overexpression in the thymus of TG mice determined diverse functional and phenotypic abnormalities. Of importance, this in vivo model will be used to investigate the role of GILZ in the anti-inflammatory and immunosuppressive actions of glucocorticoids, with the aim of selecting specific therapeutic effects without the wide array of side effects that limit the pharmacologic usage of GCs.
Prepublished online as Blood First Edition Paper, August 19, 2004; DOI 10.1182/blood-2004-03-0920.
Supported by a grant from Associazione Italiana Ricerca sul Cancro (AIRC).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank Dr Geraldine A. Boyd for her help in writing this paper in English, D. Kioussis for providing the hCD2 vector, and L. D'Adamio for providing the TAT-C vector.