Abstract
Interactions between the cyclin-dependent kinase (CDK) inhibitor flavopiridol and the proteasome inhibitor bortezomib were examined in Bcr/Abl+ human leukemia cells. Coexposure of K562 or LAMA84 cells to subtoxic concentration of flavopiridol (150-200 nM) and bortezomib (5-8 nM) resulted in a synergistic increase in mitochondrial dysfunction and apoptosis. These events were associated with a marked diminution in nuclear factor κB (NF-κB)/DNA binding activity; enhanced phosphorylation of SEK1/MKK4 (stress-activated protein kinase/extracellular signal-related kinase 1/mitogen-activated protein kinase kinase 4), c-Jun N-terminal kinase (JNK), and p38 mitogen-activated protein kinase (MAPK); down-regulation of Bcr/Abl; and a marked reduction in signal transducer and activator of transcription 3 (STAT3) and STAT5 activity. In imatinib mesylate-resistant K562 cells displaying increased Bcr/Abl expression, bortezomib/flavopiridol treatment markedly increased apoptosis in association with down-regulation of Bcr/Abl and BclxL, and diminished phosphorylation of Lyn, Hck, CrkL, and Akt. Parallel studies were performed in imatinib mesylate-resistant LAMA84 cells exhibiting reduced expression of Bcr/Abl but a marked increase in expression/activation of Lyn and Hck. Flavopiridol/bortezomib effectively induced apoptosis in these cells in association with Lyn and Hck inactivation. The capacity of flavopiridol to promote bortezomib-mediated Bcr/Abl down-regulation and apoptosis was mimicked by the positive transcription elongation factor-b (P-TEFb) inhibitor DRB (5,6-dichloro 1-β-d-ribofuranosylbenzinida-sole). Finally, the bortezomib/flavopiridol regimen also potently induced apoptosis in Bcr/Abl- human leukemia cells. Collectively, these findings suggest that a strategy combining flavopiridol and bortezomib warrants further examination in chronic myelogenous leukemia and related hematologic malignancies. (Blood. 2004;104:509-518)
Introduction
Chronic myelogenous leukemia (CML) is a myeloproliferative disorder characterized by the 9;22 translocation, resulting in the expression of a fusion oncoprotein, Bcr/Abl, which exhibits constitutively active kinase activity.1 The Bcr/Abl kinase signals to a variety of downstream survival pathways, including the mitogen-activated protein kinase kinase (MEK)/extracellular signal-regulating kinase (ERK) cascade, Akt, signal transducers and activators of transcription (STATs), and nuclear factor κB (NF-κB), among others.2-4 Activation of these pathways in Bcr/Abl+ cells results in increased expression of several antiapoptotic proteins, such as Bcl-xL.5 Collectively, these events provide Bcr/Abl+ cells with a survival advantage over their normal counterparts, thereby contributing to the leukemic phenotype.6 Moreover, Bcr/Abl+ cells display varying degrees of resistance against conventional cytotoxic drugs.7-9 The discovery that the Bcr/Abl kinase not only promotes the proliferation of leukemic cells but is also necessary for their survival prompted the search for specific inhibitors of this kinase. Such efforts culminated in the development of the Bcr/Abl kinase inhibitor imatinib mesylate (Gleevec; STI571), which has revolutionized the treatment of CML. Imatinib mesylate has proved highly active in patients with chronic-phase CML10 and, to a lesser extent, in patents with accelerated and blastic-phase disease.11,12 Unfortunately, the pre-existence or development of imatinib mesylate resistance, generally through Bcr/Abl amplification or mutation,13,14 ultimately leads to disease progression. More recently, imatinib mesylate resistance has been associated with diminished Bcr/Abl expression and activation of other kinases (eg, Lyn).15,16 In view of the continuing problem of imatinib mesylate resistance, new approaches to the treatment of Bcr/Abl+ leukemia remain a high priority.
Recent studies indicate that malignant hematopoietic cells are particularly susceptible to a strategy in which inhibitors of cell cycle progression and survival signaling pathways are combined.17 Flavopiridol (NSC 649890) is a rohitukine alkaloid that acts as a broad inhibitor of cyclin-dependent kinases (CDKs).18 Flavopiridol also exhibits antiangiogeneic activity,19 and inhibits the positive transcription elongation factor-b (P-TEFb) cyclin T/CDK9 complex, thereby functioning as a transcriptional repressor.20 Flavopiridol potently induces apoptosis at nanomolar concentrations in human leukemia cells in vitro,21 and clinical trials combining flavopiridol with established antileukemic agents have recently been initiated in patients with refractory leukemia.22 Furthermore, preclinical studies indicate that flavopiridol enhances the activity of targeted agents such as imatinib mesylate in Bcr/Abl+ leukemia cells, including those displaying imatinib mesylate resistance.23
Bortezomib (Velcade; previously known as PS-341) is an inhibitor of the 20S proteasome, which is responsible for the degradation of diverse intracellular proteins.24 The ubiquitin/proteasome system plays a critical role in cellular homeostasis and contributes to the control of multiple proteins, including those implicated in the regulation of cell proliferation, survival, and differentiation.25 Proteasome inhibitors trigger apoptosis in malignant cells through a mechanism that has not been fully elucidated, although inactivation of the NF-κB pathway (through sparing of IκBα, an endogenous NF-κB inhibitor) has been invoked.26 Bortezomib, a boronic acid anhydride proteasome inhibitor,27 has recently shown remarkable activity in patients with multiple myeloma, including those with refractory disease.28 The role that bortezomib might play in Bcr/Abl+ hematopoietic malignancies remains largely unexplored, although proteasome inhibitors such as bortezomib and tripeptidyl aldehydes (eg, LLnV and LLnL [carbobenzoxyl-l-leucyl-l-leucyl-l-norvalinal and carbobenzoxyl-l-leucyl-l-leucyl-l-leucinal, respectively]) have been reported to down-regulate/inhibit Bcr/Abl and induce cell death in CML cells.29,30 Moreover, combined exposure to bortezomib and histone deacetylase inhibitors potently induces apoptosis in Bcr/Abl+ human leukemia cells.31
Recently, our group reported that flavopiridol interacted synergistically with proteasome inhibitors (eg, MG-132 and lactacystin) to induce mitochondrial dysfunction and apoptosis in human myeloid and lymphoid leukemia cells in vitro.32 Because Bcr/Abl+ cells are relatively resistant to apoptosis induced by conventional agents7 and depend upon unique Bcr/Abl-dependent signaling pathways for their survival, the question arose whether such cells might also be susceptible to such a strategy. To address this issue, we have examined interactions between flavopiridol and bortezomib in Bcr/Abl+ cells, including those resistant to imatinib mesylate. Our results indicate that combined administration of flavopiridol and bortezomib effectively triggers apoptosis in Bcr/Abl+ cells that are both sensitive and resistant to imatinib mesylate through a mechanism that involves inactivation of the NF-κB and STAT3/STAT5 axes. Furthermore, this regimen is active against CML cells displaying a recently described Bcr/Abl-independent form of imatinib mesylate resistance.
Materials and methods
Cells and reagents
K562 and imatinib mesylate-resistant K562 (K562-R) cells were kindly provided by Dr L Varticovski (Tufts University School of Medicine, Boston, MA). LAMA84 cells were purchased from the German Collection of Microorganisms and Cell Cultures (Braunschweig, Germany). Imatinib mesylate-resistant LAMA84 cells (LAMA84-R) were generated by incubation with increasing concentrations of imatinib mesylate as reported previously.33 U937, HL-60, Raji, Jurkat, and CCRF-CEM cells were purchased from the American Type Culture Collection (Manassas, VA).17 Cells were maintained as described previously.17,33 K562-R and LAMA84-R were maintained in the medium containing 1 μM imatinib mesylate (Novartis Pharmaceuticals, Basel, Switzerland) and cultured in drug-free medium before all experimental procedures. All experiments were performed using logarithmically growing cells (4-6 × 105 cells/mL).
Flavopiridol was provided by Dr Edward Sausville (Developmental Therapeutics Program/National Cancer Institute). The proteasome inhibitor bortezomib was provided by Millennium Pharmaceuticals (Cambridge, MA). These agents were dissolved in dimethyl sulfoxide (DMSO) as a stock solution, stored at -80°C. DRB (5,6-dichloro 1-β-d-ribofuranosylbenzimidasole, a P-TEFb inhibitor) was purchased from Sigma (St Louis, MO) and dissolved in sterile DMSO and stored frozen at -20°C. In all experiments, the final concentration of DMSO did not exceed 0.1%.
Analysis of apoptosis and mitochondrial membrane potential (Δψm)
The extent of apoptosis was evaluated by assessment of Wright Giemsa-stained cytospin preparation as described previously.17 To confirm the results of morphologic analysis, in some cases cells were also evaluated by Annexin V-fluorescein isothiocyanate (FITC) staining (BD PharMingen, San Diego, CA) and flow cytometry.34 To assess Δψm, cells were stained with 3,3-dihexyloxacarbocynine (DiOC6; Molecular Probes, Eugene, OR) and analyzed by flow cytometry. The percentage of cells exhibiting low levels of DiOC6 uptake, which reflects loss of Δψm, was determined.34
Western blot analysis
Whole-cell pellets were lysed in sodium dodecyl sulfate (SDS) sample buffer, and 30 μg protein for each condition was subjected to Western blot analysis following procedures previously described in detail.35 Where indicated, the blots were reprobed with antibodies against actin (Transduction Laboratories, Lexington, KY) to ensure equal loading and transfer of proteins. The following antibodies were used as primary antibodies: phospho-p44/42 MAP kinase (mitogen-activated protein kinase, ERK, Thr202/Tyr204) antibody (Santa Cruz Biotechnology, Santa Cruz, CA), p44/42 MAP kinase antibody (Cell Signaling Technology, Beverly, MA), phospho-SEK1/MKK4 (SAPK/ERK kinase 1/MAP kinase kinase 4, Thr261) antibody (Cell Signaling Technology), phospho-JNK (c-Jun N-terminal kinase, Thr183/Tyr185) antibody (Santa Cruz Biotechnology), SAPK (stress-activated protein kinase)/JNK antibody (Cell Signaling Technology), phospho-p38 MAP kinase (Thr180/Tyr182) antibody (Cell Signaling Technology), p38 antibody (Cell Signaling Technology), phospho-IκBα (Ser32) antibody (Cell Signaling Technology), phospho-STAT3 (Ser727) antibody (Cell Signaling Technology), STAT3 antibody (Santa Cruz Biotechnology), phospho-STAT5 (Tyr694) antibody (Cell Signaling Technology), STAT5 antibody (Santa Cruz Biotechnology), c-Abl antibody (Santa Cruz Biotechnology), phospho-Bcr (Tyr177) antibody (Cell Signaling Technology), Bcl-xL antibody (Cell Signaling Technology), phosph-Akt1/2/3 (Ser473) antibody (Santa Cruz Biotechnology), anti-PARP (poly [adenosine diphosphate [ADP]-ribose] polymerase; Biomol, Plymouth Meeting, PA), phospho-Lyn (Tyr507) antibody (Cell Signaling Technology), Lyn antibody (Cell Signaling Technology), phospho-CrkL (Tyr207) antibody (Cell Signaling Technology), CrkL (32H4) antibody (Cell Signaling Technology), phospho-Hck (Tyr411) antibody (Santa Cruz Biotechnology), anti-Hck antibody (Upstate Biotechnology, Lake Placid, NY), anti-RNA polymerase II (N20) antibody (Santa Cruz Biotechnology), and phospho-RNA polymerase II (CTD4H8) antibody (Upstate Biotechnology).
Analysis of cytosolic cytochrome c and Smac/DIABLO
S-100 cytosolic extract was prepared as described previously.17 The protein samples were quantified, separated by 15% SDS-polyacrylamide gel electrophoresis (PAGE), and subjected to Western blot analysis. Anti-cytochrome c (BD PharMingen) and smac/DIABLO antibody (Upstate Biotechnology) were used as primary antibody.
Electrophoretic mobility shift assay (EMSA)
Nuclear extracts were prepared as reported previously.36 DNA double-stranded oligonucleotides corresponding to consensus binding site for NF-κB (5′-AGTTGAGGGGACTTTCCCAGGC-3′; Promega, Madison, WI), STAT5 (5′-AGATTTCTAGGAATTCAATCC-3′; Santa Cruz Biotechnology), and STAT3 (5′-GATCCTTCTGGGAATTCCTAGATC-3′; Santa Cruz Biotechnology) were labeled with [γ-32P]-adenosine triphosphate (ATP) and purified as described previously.37 Nuclear extracts (5 μg) were incubated at 4°C for 20 minutes with 105 cpm of labeled oligonucleotide probe in binding buffer. To identify the specificity of DNA binding, nuclear extracts obtained from control cells were incubated at room temperature for 30 minutes with TransCruz gel supershift antibodies specifically against STAT5 and STAT3 (Santa Cruz Biotechnology) prior to addition of 32P-labeled oligonucleotides. Alternatively, 100-fold excess of unlabeled specific oligonucleotides was preincubated for 10 minutes at room temperature with the nuclear extract prior to addition of 32P-labeled oligonucleo-tides. Reaction mixtures were subjected to electrophoresis and autoradiography.
Statistical analysis
For analysis of apoptosis and Δψm, values represent the means ± SD for at least 3 separate experiments performed in triplicate. The significance of differences between experimental variables was determined using the Student t test. Analysis of synergism was performed according to Median Dose Effect analysis38 using a commercially available software program (Biosoft, Ferguson, MO).
Results
Bortezomib interacts synergistically with flavopiridol to induce mitochondrial dysfunction and apoptosis in K562 and LAMA84 cells
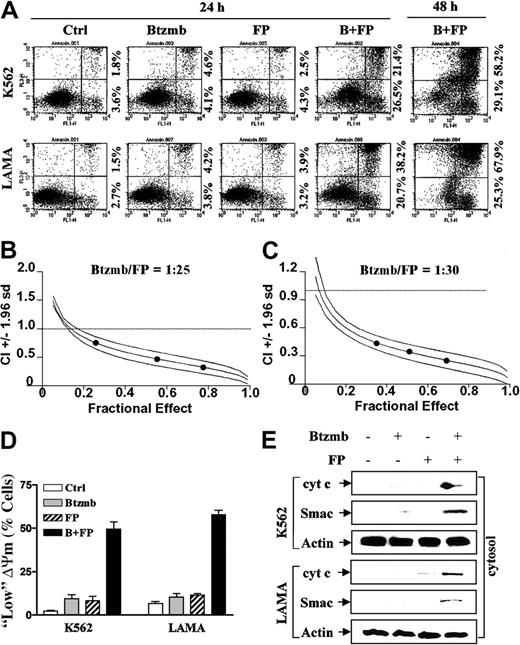
To assess bortezomib/flavopiridol interactions in Bcr/Abl+ cells, K562 and LAMA84 cells were exposed to 150 to 200 nM flavopiridol ± 5 to 8 nM bortezomib for 24 or 48 hours, after which apoptosis was assessed by Annexin V/propidium iodide (PI) analysis. Treatment of cells with these agents individually for 24 hours minimally increased the percentage of early apoptotic (Figure 1A; lower right quadrant; Annexin V+) and late apoptotic (upper right quadrant; Annexin V+/PI+) cells (eg, < 6% total in each case). In contrast, combined flavopiridol/bortezomib treatment resulted in 50% to 60% early and late apoptotic cells by 24 hours, and more than 85% by 48 hours. Median Dose Effect analysis of apoptosis induction by flavopiridol/bortezomib administered at a fixed ratio (K562, 25:1; LAMA84, 30:1) yielded combination index values considerably lower than 1.0, indicating a highly synergistic interaction (Figure 1B-C). Thus, despite resistance to apoptosis induced by conventional cytotoxic agents,7-9 Bcr/Abl+ leukemic cells were highly susceptible to the flavopiridol/bortezomib regimen.
Bortezomib interacts synergistically with flavopiridol to induce mitochondrial dysfunction and apoptosis in CML cells. (A) K562 and LAMA84 cells were exposed to flavopiridol (FP, K562: 200 nM; LAMA: 150 nM) ± bortezomib (Btzmb or Bz, K562: 8 nM; LAMA: 5 nM) for 24 hours and 48 hours, after which the percentage of apoptotic cells was determined by Annexin V-FITC staining and flow cytometry as described in “Materials and methods.” Annexin V+/PI-corresponds to early apoptosis and Annexin V+/PI+ to late apoptosis. Numbers reflect the percentage of cells in the corresponding quadrants. Results are representative of 3 separate experiments. (B-C) K562 (B) and LAMA84 (C) cells were treated with a range of FP and Btzmb concentrations alone and in combination for 48 hours at a fixed ratio as indicated. At the end of this period, the percentage of cells exhibiting apoptotic morphology was determined by evaluation of Wright Giemsa-stained cytospin preparations for each condition; fractional effect values were determined by comparing results to those of untreated controls (Ctrl), and Median Dose Effect analysis was used to characterize the nature of the interaction. Combination index (CI) values less than 1.0 denote a synergistic interaction. An additional 2 studies yielded equivalent results. (D) K562 and LAMA84 cells were treated for 24 hours as described for panel A, after which the percentage of cells exhibiting reduced mitochondrial membrane potential (Δψm) was determined by monitoring DiOC6 uptake as described in “Materials and methods.” Results represent the means ± SDs for 3 separate experiments performed in triplicate. (E) Alternatively, cytosolic (S-100) fractions were prepared as described in “Materials and methods,” and expression of cytochrome c (cyt c) and Smac/DIABLO in cytosol was monitored by Western blot. Each lane was loaded with 30 μg protein; blots were stripped and reprobed with antiactin antibodies to ensure equal loading and transfer of protein. An additional 2 studies yielded equivalent results.
Bortezomib interacts synergistically with flavopiridol to induce mitochondrial dysfunction and apoptosis in CML cells. (A) K562 and LAMA84 cells were exposed to flavopiridol (FP, K562: 200 nM; LAMA: 150 nM) ± bortezomib (Btzmb or Bz, K562: 8 nM; LAMA: 5 nM) for 24 hours and 48 hours, after which the percentage of apoptotic cells was determined by Annexin V-FITC staining and flow cytometry as described in “Materials and methods.” Annexin V+/PI-corresponds to early apoptosis and Annexin V+/PI+ to late apoptosis. Numbers reflect the percentage of cells in the corresponding quadrants. Results are representative of 3 separate experiments. (B-C) K562 (B) and LAMA84 (C) cells were treated with a range of FP and Btzmb concentrations alone and in combination for 48 hours at a fixed ratio as indicated. At the end of this period, the percentage of cells exhibiting apoptotic morphology was determined by evaluation of Wright Giemsa-stained cytospin preparations for each condition; fractional effect values were determined by comparing results to those of untreated controls (Ctrl), and Median Dose Effect analysis was used to characterize the nature of the interaction. Combination index (CI) values less than 1.0 denote a synergistic interaction. An additional 2 studies yielded equivalent results. (D) K562 and LAMA84 cells were treated for 24 hours as described for panel A, after which the percentage of cells exhibiting reduced mitochondrial membrane potential (Δψm) was determined by monitoring DiOC6 uptake as described in “Materials and methods.” Results represent the means ± SDs for 3 separate experiments performed in triplicate. (E) Alternatively, cytosolic (S-100) fractions were prepared as described in “Materials and methods,” and expression of cytochrome c (cyt c) and Smac/DIABLO in cytosol was monitored by Western blot. Each lane was loaded with 30 μg protein; blots were stripped and reprobed with antiactin antibodies to ensure equal loading and transfer of protein. An additional 2 studies yielded equivalent results.
To assess the effects of flavopiridol/bortezomib on mitochondrial function, K562 and LAMA84 cells were exposed to flavopiridol ± bortezomib for 24 hours, after which loss of mitochondrial membrane potential (Δψm) and release of cyto-chrome c and Smac/DIABLO into the S-100 cytosolic fraction were monitored. In both cell lines, treatment with flavopiridol or bortezomib individually resulted in minimal reductions in Δψm, whereas combined treatment caused extensive loss of Δψm (Figure 1D). Furthermore, exposure of cells to flavopiridol or bortezomib alone failed to increase release of cytochrome c or Smac/DIABLO, whereas redistribution of these proteins could be clearly discerned in cells treated with both agents (Figure 1E). Thus, combined flavopiridol/bortezomib exposure significantly increases mitochondrial dysfunction in Bcr/Abl+ human leukemia cells.
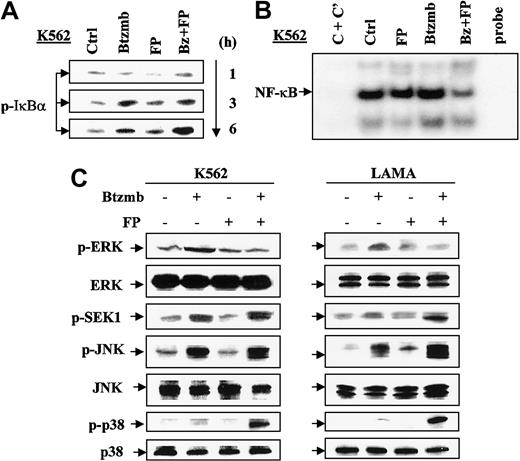
Coadministration of bortezomib/flavopiridol results in blockade of the IκB/NF-κB pathway and activation of the SAPK/JNK cascade
Flavopiridol/bortezomib interactions were then examined in relation to perturbations in the NF-κB and MAP kinase signaling pathways. Treatment of K562 cells with bortezomib ± flavopiridol resulted in a modest increase in levels of phospho-IκBα by 1 and 3 hours of drug exposure. However, at 6 hours, a clear increase in phospho-IκBα levels was noted in cells exposed to both agents (Figure 2A). Consistent with the net increase in IκB levels (data not shown), a clear reduction in NF-κB/DNA binding, reflected by EMSA analysis, was observed in cells exposed to the bortezomib/flavopiridol combination (Figure 2B).
Exposure of CML cells to bortezomib/flavopiridol induces perturbations in the IκB/NF-κB, SAPK, and MAPK pathways. (A) K562 cells were exposed to 8 nM bortezomib (Btzmb or Bz) ± 200 nM flavopiridol (FP) for 1 to 6 hours, after which the cells were lysed and subjected to Western blot analysis to monitor expression of phosphorylated IκBα. (B) Alternatively, K562 cells were treated for 24 hours as described for panel A, after which nuclear extracts were prepared and subjected to electrophoretic mobility shift assay (EMSA) as described in “Materials and methods.” For C + C′ (lane 1), 100-fold excess of unlabeled NF-κB oligonucleo-tides was preincubated for 10 minutes with the nuclear extract obtained from untreated cells prior to addition of labeled NF-κB oligonucleotides. Lane 6 was loaded with labeled NF-κB oligonucleotides. Results are representative of 3 separate experiments. (C) K562 (left) and LAMA84 (right) cells were incubated with Btzmb (K562: 8 nM; LAMA: 5 nM) ± FP (K562: 200 nM; LAMA: 150 nM) for 24 hours, after which cells were lysed and subjected to Western blot using the indicated antibodies. For panels A and C, each lane was loaded with 30 μg protein. An additional 2 studies yielded equivalent results.
Exposure of CML cells to bortezomib/flavopiridol induces perturbations in the IκB/NF-κB, SAPK, and MAPK pathways. (A) K562 cells were exposed to 8 nM bortezomib (Btzmb or Bz) ± 200 nM flavopiridol (FP) for 1 to 6 hours, after which the cells were lysed and subjected to Western blot analysis to monitor expression of phosphorylated IκBα. (B) Alternatively, K562 cells were treated for 24 hours as described for panel A, after which nuclear extracts were prepared and subjected to electrophoretic mobility shift assay (EMSA) as described in “Materials and methods.” For C + C′ (lane 1), 100-fold excess of unlabeled NF-κB oligonucleo-tides was preincubated for 10 minutes with the nuclear extract obtained from untreated cells prior to addition of labeled NF-κB oligonucleotides. Lane 6 was loaded with labeled NF-κB oligonucleotides. Results are representative of 3 separate experiments. (C) K562 (left) and LAMA84 (right) cells were incubated with Btzmb (K562: 8 nM; LAMA: 5 nM) ± FP (K562: 200 nM; LAMA: 150 nM) for 24 hours, after which cells were lysed and subjected to Western blot using the indicated antibodies. For panels A and C, each lane was loaded with 30 μg protein. An additional 2 studies yielded equivalent results.
Treatment with bortezomib alone modestly increased phospho-ERK1/2 in both K562 and LAMA84 cells, but this effect was abrogated by flavopiridol (Figure 2C). Consistent with earlier reports involving other cell types,32 exposure of K562 and LAMA84 cells to bortezomib alone resulted in increased phosphorylation (activation) of the stress-related SEK1 and JNK kinases (Figure 2C). However, coadministration of flavopiridol with bortezomib led to further activation of SEK1 and JNK. Neither flavopiridol nor bortezomib alone increased levels of phosphorylated p38 MAPK, whereas combined treatment had a pronounced effect. Together, these findings indicate that exposure of Bcr/Abl+ leukemia cells to the bortezomib/flavopiridol regimen results in diminished NF-κB/DNA binding and an increase in the net output of stress-related (eg, JNK and p38 MAPK) versus cytoprotective (eg, ERK1/2) MAP kinases.
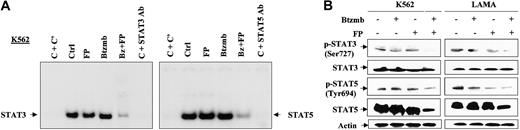
Bortezomib in combination with flavopiridol diminishes activity of STAT3 and STAT5
The STAT family of transcription factors has been implicated in transformation and antiapoptotic signaling stemming from constitutive activation of the Bcr/Abl kinase.39,40 To assess the effects of bortezomib and flavopiridol on STAT3 and STAT5 activation, EMSA analysis was used. Exposure to 200 nM flavopiridol or 8 nM bortezomib (24 hours each) individually exerted little or no effect on STAT3/DNA or STAT5/DNA binding (Figure 3A). In contrast, coadministration of bortezomib and flavopiridol induced a very pronounced reduction in STAT3/DNA and STAT5/DNA binding activity. Western analysis revealed that coadministration of flavopiridol and bortezomib in both K562 and LAMA84 cells resulted in diminished expression of STAT5 but not STAT3, and reduced phosphorylation of both STAT3 and STAT5 (Figure 3B). Together, these findings indicate that combined exposure of Bcr/Abl+ cells to bortezomib and flavopiridol results in a pronounced disabling of the STAT3 and STAT5 pathways, which play important roles in survival signaling downstream of the Bcr/Abl kinase.
Bortezomib/flavopiridol diminishes constitutive activation of STAT3 and STAT5 in CML cells. (A) K562 cells were incubated with 8 nM bortezomib (Btzmb or Bz) ± 200 nM flavopiridol (FP) for 24 hours, after which nuclear extracts were prepared and subjected to EMSA to monitor STAT3/DNA (left) and STAT5/DNA (right) binding activity as described in “Materials and methods.” For C + C′ (lane 1), 100-fold excess of unlabeled specific oligonucleotides was preincubated for 10 minutes with the nuclear extract of untreated cells prior to addition of 32P-labeled oligonucleotides. For lane 6, nuclear extracts of untreated cells were incubated with TransCruz gel supershift antibody against STAT3 and STAT5 for 30 minutes prior to addition of 32P-labeled oligonucleotides. Results are representative of 3 separate experiments. (B) K562 (left) and LAMA84 (right) cells were treated with Btzmb (K562: 8 nM; LAMA: 5 nM) ± FP (K562: 200 nM; LAMA: 150 nM) for 24 hours, after which Western blot analysis was performed to evaluate total level and phosphorylation status of STAT3 and STAT5. Each lane was loaded with 30 μg protein; blots were stripped and reprobed with antibodies to actin to ensure equal loading and transfer. An additional 2 studies yielded equivalent results.
Bortezomib/flavopiridol diminishes constitutive activation of STAT3 and STAT5 in CML cells. (A) K562 cells were incubated with 8 nM bortezomib (Btzmb or Bz) ± 200 nM flavopiridol (FP) for 24 hours, after which nuclear extracts were prepared and subjected to EMSA to monitor STAT3/DNA (left) and STAT5/DNA (right) binding activity as described in “Materials and methods.” For C + C′ (lane 1), 100-fold excess of unlabeled specific oligonucleotides was preincubated for 10 minutes with the nuclear extract of untreated cells prior to addition of 32P-labeled oligonucleotides. For lane 6, nuclear extracts of untreated cells were incubated with TransCruz gel supershift antibody against STAT3 and STAT5 for 30 minutes prior to addition of 32P-labeled oligonucleotides. Results are representative of 3 separate experiments. (B) K562 (left) and LAMA84 (right) cells were treated with Btzmb (K562: 8 nM; LAMA: 5 nM) ± FP (K562: 200 nM; LAMA: 150 nM) for 24 hours, after which Western blot analysis was performed to evaluate total level and phosphorylation status of STAT3 and STAT5. Each lane was loaded with 30 μg protein; blots were stripped and reprobed with antibodies to actin to ensure equal loading and transfer. An additional 2 studies yielded equivalent results.
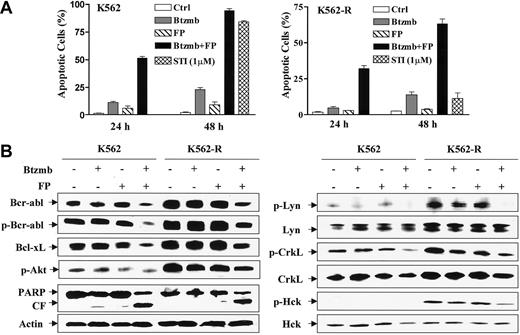
The bortezomib/flavopiridol regimen induces apoptosis in imatinib mesylate-resistant K562 cells displaying increased Bcr/Abl expression
Attempts were then made to determine the extent to which the bortezomib/flavopiridol regimen induced apoptosis in Bcr/Abl+ cells resistant to imatinib mesylate. To this end, the effects of these agents alone and in combination were examined in parental K562 and an imatinib mesylate-resistant subline (K562-R) exhibiting increased expression of Bcr/Abl. Treatment of parental cells with 200 nM bortezomib or 8 nM flavopiridol individually for 24 hours was minimally toxic, whereas combined exposure resulted in cell death in approximately 50% of cells (Figure 4A). Furthermore, more prolonged drug exposure (eg, 48 hours) triggered apoptosis in nearly 100% of cells. Continuous exposure (48 hours) to 1 μM imatinib mesylate was highly lethal to parental cells, but minimally toxic toward K562-R cells. While K562-R cells were somewhat less sensitive to the bortezomib/flavopiridol regimen than their parental counterparts, combined drug treatment resulted in a pronounced increase in lethality, particularly at 48 hours (eg, ∼ 70%).
Imatinib mesylate resistance conferred by increased Bcr/Abl expression fails to protect K562 cells from apoptosis induced by coadministration of bortezomib and flavopiridol. (A) K562 (left) and imatinib mesylate-resistant K562-R (right) cells were treated with 8 nM bortezomib (Btzmb) ± 200 nM flavopiridol (FP) for 24 hours and 48 hours, after which the percentage of cells exhibiting apoptotic morphology was determined by evaluating Wright Giemsa-stained cytospin preparations. In parallel, K562 and K562-R cells were exposed to 1 μM imatinib mesylate (STI) for 48 hours to document imatinib mesylate resistance. Results represent the means ± SDs for 3 separate experiments performed in triplicate. (B) K562 and K562-R cells were treated for 24 hours as described for panel A, after which cells were lysed and subjected to Western blot using the indicated antibodies. CF indicates cleavage fragment. Each lane was loaded with 30 μg protein; blots were stripped and reprobed with antibodies to actin to ensure equal loading and transfer. An additional 2 studies yielded equivalent results.
Imatinib mesylate resistance conferred by increased Bcr/Abl expression fails to protect K562 cells from apoptosis induced by coadministration of bortezomib and flavopiridol. (A) K562 (left) and imatinib mesylate-resistant K562-R (right) cells were treated with 8 nM bortezomib (Btzmb) ± 200 nM flavopiridol (FP) for 24 hours and 48 hours, after which the percentage of cells exhibiting apoptotic morphology was determined by evaluating Wright Giemsa-stained cytospin preparations. In parallel, K562 and K562-R cells were exposed to 1 μM imatinib mesylate (STI) for 48 hours to document imatinib mesylate resistance. Results represent the means ± SDs for 3 separate experiments performed in triplicate. (B) K562 and K562-R cells were treated for 24 hours as described for panel A, after which cells were lysed and subjected to Western blot using the indicated antibodies. CF indicates cleavage fragment. Each lane was loaded with 30 μg protein; blots were stripped and reprobed with antibodies to actin to ensure equal loading and transfer. An additional 2 studies yielded equivalent results.
K562-R cells exhibited a marked increase in Bcr/Abl expression compared with parental cells (Figure 4B, left panels). Moreover, levels of Bcl-xL were clearly elevated in the K562-R cells. However, coexposure to bortezomib/flavopiridol resulted in a decline in expression of Bcr/Abl and Bcl-xL in both the parental and imatinib mesylate-resistant lines. Expression of phospho-Akt was also markedly elevated in K562-R cells compared with parental cells but was modestly inhibited following exposure to bortezomib/flavopiridol. The extent of PARP cleavage induced by the combined treatment was comparable in the 2 cell lines. Thus, enhanced apoptosis in K562-R cells was associated with down-regulation of Bcr/Abl and Bcl-xL, as well as inactivation of Akt.
Effects of these agents were also examined in relation to expression/activation of the Bcr/Abl-related Src family kinases (eg, Lyn and Hck)41,42 as well as the adaptor protein CrkL43 (Figure 4B, right panels). Interestingly, K562-R cells displayed increased expression of both total and phosphorylated forms of the tyrosine kinase Lyn as well as the adaptor protein and Bcr/Abl substrate CrkL compared with parental K562 cells. In contrast, total levels of the tyrosine kinase Hck were equivalent in the 2 cell lines, whereas phospho-Hck was undetectable in parental cells but clearly increased in K562-R cells. In K562-R cells, bortezomib/flavopiridol abrogated phospho-Lyn expression, and reduced levels of phospho-CrkL and phospho-Hck, without inducing changes in levels of total Lyn, CrkL, and Hck. Thus, potentiation of apoptosis in imatinib mesylate-resistant Bcr/Abl kinase-overexpressing cells was associated with diminished phosphorylation/activation of Lyn, CrkL, and Hck, proteins whose activation status has been linked to Bcr/Abl actions.44-47
The bortezomib/flavopiridol regimen induces apoptosis in imatinib mesylate-resistant LAMA84 cells exhibiting diminished Bcr/Abl expression and increased Lyn expression/activation
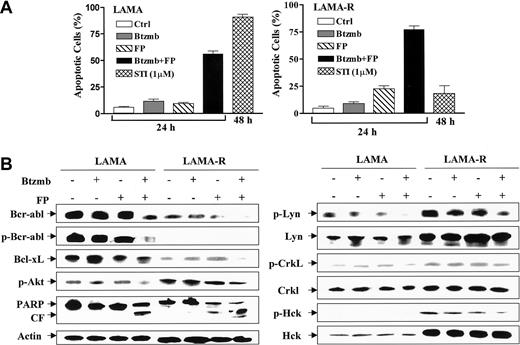
Parallel studies were performed in LAMA84 cells rendered resistant to imatinib mesylate (LAMA84-R) by continuous culture in imatinib mesylate-containing medium. As shown in Figure 5A, bortezomib and flavopiridol administered individually (24 hours each) were minimally toxic to parental LAMA84 cells as well as their imatinib mesylate-resistant counterparts. However combined exposure to bortezomib and flavopiridol resulted in a pronounced increase in apoptosis in parental cells; moreover, LAMA84-R cells were, if anything, more sensitive to the bortezomib/flavopiridol regimen than parental cells. As anticipated, LAMA84-R cells displayed significant resistance to 1 μM imatinib mesylate relative to parental LAMA84 cells (P < .001).
The bortezomib/flavopiridol regimen induces apoptosis in imatinib mesylate-resistant LAMA84 cells exhibiting Lyn overexpression and diminished expression of Bcr/Abl. (A) LAMA84 (left) and LAMA84-R (right) cells were incubated in the presence of 5 nM bortezomib (Btzmb) ± flavopiridol (FP: LAMA, 150 nM; LAMA-R, 100 nM) for 24 hours, or 1 μM imatinib mesylate for 48 hours, after which percentage of cells exhibiting apoptotic morphology was determined by evaluating Wright Giemsa-stained cytospin preparations. Results represent the means ± SDs for 3 separate experiments performed in triplicate. (B) Cells were treated as described for panel A, after which cells were lysed and subjected to Western blot using the indicated primary antibodies. CF indicates cleavage fragment. Each lane was loaded with 30 μg protein; blots were stripped and reprobed with antibodies to actin to ensure equal loading and transfer. An additional 2 studies yielded equivalent results.
The bortezomib/flavopiridol regimen induces apoptosis in imatinib mesylate-resistant LAMA84 cells exhibiting Lyn overexpression and diminished expression of Bcr/Abl. (A) LAMA84 (left) and LAMA84-R (right) cells were incubated in the presence of 5 nM bortezomib (Btzmb) ± flavopiridol (FP: LAMA, 150 nM; LAMA-R, 100 nM) for 24 hours, or 1 μM imatinib mesylate for 48 hours, after which percentage of cells exhibiting apoptotic morphology was determined by evaluating Wright Giemsa-stained cytospin preparations. Results represent the means ± SDs for 3 separate experiments performed in triplicate. (B) Cells were treated as described for panel A, after which cells were lysed and subjected to Western blot using the indicated primary antibodies. CF indicates cleavage fragment. Each lane was loaded with 30 μg protein; blots were stripped and reprobed with antibodies to actin to ensure equal loading and transfer. An additional 2 studies yielded equivalent results.
Western blot analysis was used to characterize the molecular basis of imatinib mesylate resistance in these cells. LAMA84-R cells displayed a marked reduction in Bcr/Abl expression and phosphorylation (Figure 5B, left panels), analogous to imatinib mesylate-resistant K562 cell lines described by other groups.15,16 They also exhibited diminished expression of Bcl-xL but increased levels of phospho-Akt. Combined exposure to bortezomib and flavopiridol reduced Bcr/Abl and Bcl-xL expression in LAMA84 cells, analogous to results in the K562 and K562-R lines. PARP degradation following bortezomib/flavopiridol exposure was roughly equivalent in LAMA84 and LAMA84-R cells.
In accord with the results of Donato et al,15 LAMA84-R cells exhibited increased expression of total and phosphorylated forms of Lyn and Hck (Figure 5B, right panels). Combined treatment with bortezomib and flavopiridol had little effect on total levels of these proteins. Bortezomib/flavopiridol did, however, result in diminished phosphorylation/activation of Lyn and reduced levels of phospho-Hck in LAMA84-R cells. As in the case of K562 cells, phospho-Hck was undetectable in wild-type LAMA84 cells. Collectively, these findings indicate that the bortezomib/flavopiridol regimen effectively induces apoptosis in CML cells displaying a novel form of imatinib mesylate resistance characterized by diminished Bcr/Abl expression and increased expression/activation of the Lyn kinase. They also demonstrate that this phenomenon is characterized by down-regulation of Bcr/Abl and Bcl-xL proteins, and diminished phosphorylation/activation of the Src kinases Lyn and Hck.
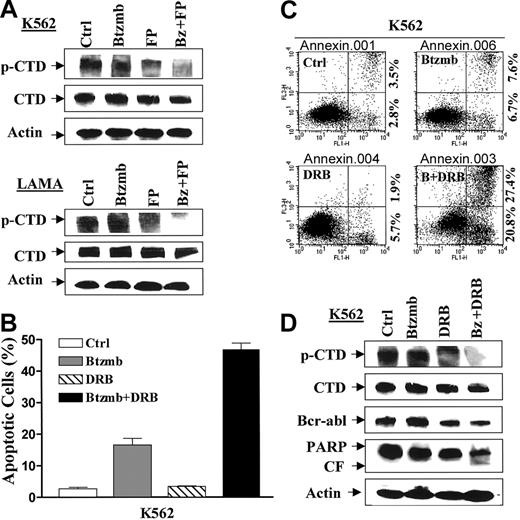
Flavopiridol/bortezomib inhibits CTD phosphorylation of RNA polymerase II, an action mimicked by the P-TEFb inhibitor DRB
Previous studies have shown that flavopiridol acts, at least in part, by blocking phosphorylation of the carboxy terminal domain (CTD) of RNA polymerase II through inhibition of the P-TEFb CDK9/cyclin T complex.20 To assess the possible contribution of this phenomenon to bortezomib/flavopiridol lethality in Bcr/Abl+ cells, 5,6-dichloro-1-β-D-ribofuranosylbenzimidazole (DRB), a P-TEFb inhibitor,48 was used. Consistent with previous reports,49 flavopiridol decreased expression of phospho-CTD in both K562 and LAMA84 cells (Figure 6A). However, coadministration of bortezomib, which by itself had little effect, led to a pronounced reduction in CTD phosphorylation. In addition, DRB, which by itself was nontoxic, significantly increased the percentage of morphologically apoptotic (Figure 6B) and Annexin V/PI+ cells (Figure 6C) following bortezomib exposure. Interestingly, DRB alone diminished CTD phosphorylation and resulted in Bcr/Abl down-regulation in K562 cells (Figure 6D). Coadministration of bortezomib with DRB led to a very modest further reduction in Bcr/Abl expression but a substantial increase in PARP cleavage and abrogation of CTD phosphorylation. Together, these findings support the notion that inhibition of P-TEFb contributes to the enhanced lethality of the bortezomib/flavopiridol regimen in Bcr/Abl+ leukemia cells.
Bortezomib/flavopiridol inhibits phosphorylation of the C-terminal domain (CTD) of RNA polymerase II, an action mimicked by the P-TEFb inhibitor DRB. (A) K562 (top) and LAMA84 (bottom) cells were incubated in the presence of flavopiridol (FP, K562: 200 nM; LAMA: 150 nM) ± bortezomib (Btzmb or Bz, K562: 8 nM; LAMA: 5 nM) for 24 hours, after which Western blot analysis was performed to monitor phosphorylation of CTD. (B) K562 cells were exposed to 8 nM bortezomib (Btzmb) ± 30 μM DRB for 48 hours, after which percentage of cells exhibiting apoptotic morphology was determined by evaluating Wright Giemsa-stained cytospin preparations. Results represent the means ± SDs for 3 separate experiments performed in triplicate. (C) Alternatively, K562 cells were treated as described for panel B, and apoptosis was assessed by Annexin V-FITC staining and flow cytometry as described for Figure 1A. Results are representative of 3 separate experiments. (D) K562 cells were treated as described for panel B, after which cells were lysed and subjected to Western blot using the indicated primary antibodies. CF indicates cleavage fragment. For panels A and D, each lane was loaded with 30 μg protein; blots were stripped and reprobed with antibodies to actin to ensure equal loading and transfer. An additional 2 studies yielded equivalent results.
Bortezomib/flavopiridol inhibits phosphorylation of the C-terminal domain (CTD) of RNA polymerase II, an action mimicked by the P-TEFb inhibitor DRB. (A) K562 (top) and LAMA84 (bottom) cells were incubated in the presence of flavopiridol (FP, K562: 200 nM; LAMA: 150 nM) ± bortezomib (Btzmb or Bz, K562: 8 nM; LAMA: 5 nM) for 24 hours, after which Western blot analysis was performed to monitor phosphorylation of CTD. (B) K562 cells were exposed to 8 nM bortezomib (Btzmb) ± 30 μM DRB for 48 hours, after which percentage of cells exhibiting apoptotic morphology was determined by evaluating Wright Giemsa-stained cytospin preparations. Results represent the means ± SDs for 3 separate experiments performed in triplicate. (C) Alternatively, K562 cells were treated as described for panel B, and apoptosis was assessed by Annexin V-FITC staining and flow cytometry as described for Figure 1A. Results are representative of 3 separate experiments. (D) K562 cells were treated as described for panel B, after which cells were lysed and subjected to Western blot using the indicated primary antibodies. CF indicates cleavage fragment. For panels A and D, each lane was loaded with 30 μg protein; blots were stripped and reprobed with antibodies to actin to ensure equal loading and transfer. An additional 2 studies yielded equivalent results.
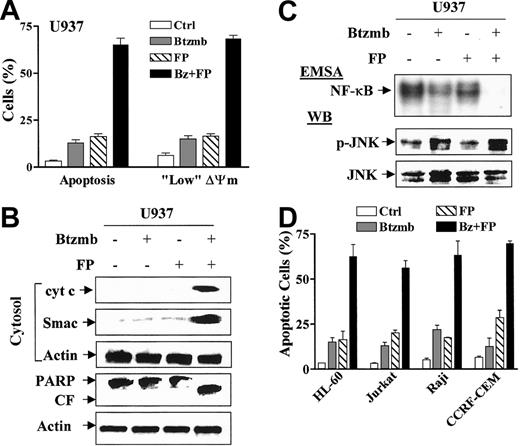
The bortezomib/flavopiridol regimen synergistically induces mitochondrial dysfunction and apoptosis in Bcr/Abl- human leukemia cells
To determine whether synergistic interactions between flavopiridol and bortezomib were restricted to Bcr/Abl+ cells, parallel studies were carried out in a variety of Bcr/Abl- human leukemic cell types. As shown in Figure 7A, exposure of U937 cells to 5 nM bortezomib or 100 nM flavopiridol for 24 hours individually had little effect on loss of Δψm or apoptosis, whereas combined treatment was associated with pronounced increases in these events. Consistent with these findings, combined exposure of cells to these agents resulted in marked increases in cytosolic release of cytochrome c and Smac/DIABLO accompanied by PARP degradation (Figure 7B). Analogous to results obtained in Bcr/Abl+ cells, flavopiridol marginally and bortezomib modestly reduced NF-κB/DNA binding, whereas combined treatment essentially abrogated NF-κB activity (Figure 7C). Similarly, combined exposure of cells to these agents resulted in a marked increase in JNK activation in U937 cells (Figure 7C). Finally, coexposure to flavopiridol and bortezomib resulted in greater than additive effects on apoptosis in a variety of other human myeloid (HL-60) and lymphoid (Jurkat, Raji, CCRF-CEM) leukemia cell lines (Figure 7D).
Cotreatment with bortezomib/flavopiridol synergistically induces apoptosis in multiple Bcr/Abl-human leukemia cells, accompanied by abrogation of NF-κB/DNA binding activity and activation of JNK. (A) U937 cells were exposed to 5 nM bortezomib (Btzmb or Bz) ± 100 nM flavopiridol (FP) for 24 hours, after which the percentage of cells exhibiting apoptotic morphology and reduced Δψm was determined by evaluating Wright Giemsa-stained cytospin preparations and monitoring DiOC6 uptake, respectively. Results represent the means ± SDs for 3 separate experiments performed in triplicate. (B) Alternatively, cytosolic (S-100) fractions and whole-cell lysates were prepared, and expression of cytochrome c and Smac/DIABLO in cytosol (upper panels) and PARP cleavage (lower panels) was monitored by Western blot. CF indicates cleavage fragment. Each lane was loaded with 30 μg protein; blots were stripped and reprobed with antiactin antibodies to ensure equal loading and transfer of protein. An additional 2 studies yielded equivalent results. (C) U937 cells were treated as described for panel A, after which nuclear extracts and cell lysates were prepared and subjected to electrophoretic mobility shift assay (EMSA, top blot) and Western blot analysis (WB, lower blots), respectively. Results are representative of 3 separate experiments. (D) Multiple human leukemia cells were exposed to bortezomib (Btzmb or Bz, HL-60, 3 nM; Jurkat, 7.5 nM; Raji and CCRF-CEM, 5 nM) ± flavopiridol (FP, 100 nM) for 24 hours, after which the percentage of cells exhibiting apoptotic morphology was determined by evaluating Wright Giemsa-stained cytospin preparations. Results represent the means ± SDs for at least 3 separate experiments performed in triplicate.
Cotreatment with bortezomib/flavopiridol synergistically induces apoptosis in multiple Bcr/Abl-human leukemia cells, accompanied by abrogation of NF-κB/DNA binding activity and activation of JNK. (A) U937 cells were exposed to 5 nM bortezomib (Btzmb or Bz) ± 100 nM flavopiridol (FP) for 24 hours, after which the percentage of cells exhibiting apoptotic morphology and reduced Δψm was determined by evaluating Wright Giemsa-stained cytospin preparations and monitoring DiOC6 uptake, respectively. Results represent the means ± SDs for 3 separate experiments performed in triplicate. (B) Alternatively, cytosolic (S-100) fractions and whole-cell lysates were prepared, and expression of cytochrome c and Smac/DIABLO in cytosol (upper panels) and PARP cleavage (lower panels) was monitored by Western blot. CF indicates cleavage fragment. Each lane was loaded with 30 μg protein; blots were stripped and reprobed with antiactin antibodies to ensure equal loading and transfer of protein. An additional 2 studies yielded equivalent results. (C) U937 cells were treated as described for panel A, after which nuclear extracts and cell lysates were prepared and subjected to electrophoretic mobility shift assay (EMSA, top blot) and Western blot analysis (WB, lower blots), respectively. Results are representative of 3 separate experiments. (D) Multiple human leukemia cells were exposed to bortezomib (Btzmb or Bz, HL-60, 3 nM; Jurkat, 7.5 nM; Raji and CCRF-CEM, 5 nM) ± flavopiridol (FP, 100 nM) for 24 hours, after which the percentage of cells exhibiting apoptotic morphology was determined by evaluating Wright Giemsa-stained cytospin preparations. Results represent the means ± SDs for at least 3 separate experiments performed in triplicate.
Discussion
Recent studies have demonstrated that neoplastic cells of hematopoietic origin are particularly susceptible to a strategy in which cell cycle and survival signaling pathways are simultaneously interrupted. For example, coadministration of the checkpoint abrogator UCN-01 with pharmacologic inhibitors of the cytoprotective MEK/ERK pathway (eg, PD184352) leads to a dramatic increase in apoptosis in a variety of human leukemia and myeloma cells.17,35 Analogously, flavopiridol, a pan-CDK inhibitor, and proteasome inhibitors such as MG-132 have recently been shown to interact in a highly synergistic manner to trigger apoptosis in various human leukemia cell types.32 Because constitutive activation of the Bcr/Abl kinase leads to multiple perturbations (eg, up-regulation of Bcl-xL and activation of NF-κB)4,5 that oppose apoptosis, Bcr/Abl+ cells are traditionally resistant to conventional cytotoxic agents.7-9 However, a regimen combining flavopiridol, which potently induces apoptosis in human leukemia cells at nanomolar concentrations,21 with bortezomib, an agent that has shown remarkable activity against multiple myeloma cells50 and, more recently, CML cells,29 proved highly effective in engaging the cell death pathway in otherwise apoptosis-resistant Bcr/Abl+ leukemic cells.
It is noteworthy that synergistic induction of apoptosis by the flavopiridol/bortezomib regimen occurred in conjunction with Bcr/Abl down-regulation. In this regard, several novel agents, including the heat shock protein 90 (Hsp90) antagonist 17-AAG16 and several histone deacetylase (HDAC) inhibitors (eg, suberoylanilide hydroxamic acid [SAHA] and LAQ824),51,52 have been shown to promote apoptosis in such cells in association with Bcr/Abl down-regulation. Moreover, coadministration of agents including HDAC inhibitors33,51 or flavopiridol23 with imatinib mesylate also induced a pronounced reduction in Bcr/Abl expression. Consequently, it appears plausible that the reduction in Bcr/Abl expression by the flavopiridol/bortezomib regimen contributes, at least in part, to the antileukemic synergism of this combination.
Several lines of evidence suggest that interference with the cytoprotective NF-κB pathway plays an important role in bortezomib/flavopiridol synergism in Bcr/Abl+ cells. For example, the functional relationship between NF-κB survival signaling with activation of the Bcr/Abl kinase has been documented in multiple studies.53-55 Moreover, the lethal effects of proteasome inhibitors, including bortezomib, have been related to inactivation of the NF-κB cascade,56 presumably a consequence of sparing of IκBα from proteasomal degradation, allowing it to sequester NF-κB in the cytoplasm.26 Thus, Bcr/Abl+ leukemic cells, which, like multiple myeloma cells, are also dependent upon NF-κB survival signals,57 may also be susceptible to proteasome inhibitor-mediated lethality.29,30 Finally, recent studies suggest that the Akt58 and NF-κB pathways59 may play particularly important roles in protecting human leukemia cells from the lethal effects of CDK inhibition (ie, by agents such as flavopiridol).
The finding that bortezomib/flavopiridol-induced lethality in Bcr/Abl+ cells was associated with JNK activation is compatible with results of earlier investigations of the proteasome inhibitor/flavopiridol regimen in Bcr/Abl- human leukemia cells,32 as well as with recent evidence of JNK activation in Bcr/Abl+ cells undergoing apoptosis in response to bortezomib and HDAC inhibitors.31 There is abundant evidence linking activation of the stress-related JNK pathway to cell death,60 including that occurring in Bcr/Abl+ cells.61 An association between JNK activation and disruption of the cytoprotective NF-κB pathway has also been described.62 Such findings raise the possibility that bortezomib/flavopiridol-mediated interruption of NF-κB signaling may enhance JNK activation, thereby potentiating the lethal response.
Activation of STAT3 and STAT5 has been implicated in survival signaling downstream of Bcr/Abl63,64 ; moreover, inhibition of STAT5 by Bcr/Abl kinase inhibitors (eg, PD180970) has been shown to induce apoptosis in Bcr/Abl+ cells.65 Furthermore, the imatinib mesylate lethality in Bcr/Abl+ cells has been related, at least in part, to interruption of STAT signaling.66 The downstream targets of STAT3 and STAT5 responsible for enhanced survival of Bcr/Abl+ cells are not known with certainty, but may involve myeloid cell leukemia 1 (Mcl-1), survivin, or Bcl-xL.67-69 In view of these considerations, it is noteworthy that combined (but not individual) exposure of cells to flavopiridol and bortezomib resulted in diminished STAT3 and STAT5 phosphorylation and a very pronounced reduction in STAT3/DNA and STAT5/DNA binding activity. Collectively, these findings suggest that interference with STAT signaling in Bcr/Abl+ cells plays a significant role in bortezomib/flavopiridol lethality. Interestingly, synergistic effects of flavopiridol and imatinib mesylate in Bcr/Abl+ cells were not associated with major changes in STAT5 phosphorylation status,23 suggesting that interactions between flavopiridol and bortezomib versus imatinib mesylate proceed through separate mechanisms, at least as far as STAT signaling is concerned.
Combined treatment with bortezomib and flavopiridol also resulted in down-regulation of Bcl-xL and modest inactivation of Akt, proteins known to lie downstream of Bcr/Abl and which are thought to contribute to enhanced survival of Bcr/Abl+ cells.6,9 The mechanism by which the bortezomib/flavopiridol regimen diminished Bcl-xL and phospho-Akt remains to be determined, but the possibility that diminished Bcr/Abl protein levels and/or inhibition of STAT5 contribute to this phenomenon seems plausible.5,6
Notably, the bortezomib/flavopiridol regimen potently triggered apoptosis in imatinib mesylate-resistant cells exhibiting increased Bcr/Abl protein. Furthermore, this occurred in association with diminished Bcr/Abl protein expression and phosphorylation. In conjunction with recent findings involving the flavopiridol/imatinib mesylate combination,23 the possibility arises that down-regulation of Bcr/Abl by bortezomib/flavopiridol may mimic the effects of direct inhibition of Bcr/Abl by imatinib mesylate, thus contributing to enhanced cell death. It is noteworthy that increased Bcr/Abl protein expression in imatinib mesylate-resistant K562-R cells was associated with enhanced activation/phosphorylation of the Src tyrosine kinases Lyn and Hck as well as the adaptor protein CrkL, all of which have been associated with constitutive activation of the Bcr/Abl kinase.44-47 Significantly, combined exposure to the bortezomib/flavopiridol regimen diminished expression of phosphorylated forms of these proteins. While the functional contribution of these events to synergistic interactions between bortezomib and flavopiridol remains to be established, given evidence linking these kinases to Bcr/Abl survival functions,41,42,47,70 it is tempting to speculate that they may play a significant role.
Resistance to imatinib mesylate in Bcr/Abl+ cells in culture as well as in patient-derived cells has been attributed to bcr/abl gene amplification, increased levels of the Bcr/Abl protein, or mutations in the imatinib mesylate binding site (eg, Thr315Ile) of the Bcr/Abl kinase.71,72 In addition, mutations distant to the kinase domain that cause allosteric changes incompatible with imatinib mesylate binding have been described.73 Recently, however, several groups have described a putatively Bcr/Abl-independent form of imatinib mesylate resistance characterized by diminished Bcr/Abl expression and an increase in expression of the Lyn and Hck kinases.15,16 The characteristics of LAMA84-R cells (ie, reduced expression of Bcr/Abl and increased levels of total and phosphorylated Lyn and Hck) are very similar to those of the K562 cell lines described by Donato et al.15 The observation that LAMA84-R cells displayed diminished Bcl-xL expression in all likelihood reflects down-regulation of Bcr/Abl, and in addition suggests that this protein does not contribute to imatinib mesylate resistance, at least in this imatinib mesylate-resistant cell line. As noted in K562-R cells, combined treatment with flavopiridol/bortezomib induced clear decreases in levels of phosphorylated Lyn and Hck. Based upon the present and previous studies,15,41 it appears plausible that enhanced activation of Lyn and Hck, both of which can act through Bcr/Abl downstream targets (eg, STAT5 and ERK),42,74-76 may subsume some of the survival functions of Bcr/Abl. Furthermore, such events may also attenuate apoptosis induced by imatinib mesylate and other agents acting more proximally in the survival cascade. As a corollary, the bortezomib/flavopiridol regimen, by virtue of its capacity to inactivate the downstream targets Lyn and Hck, may potentially circumvent certain Bcr/Abl-independent forms of imatinib mesylate resistance. The clinical relevance of this form of drug resistance in patients who have progressed on imatinib mesylate is currently the subject of intense interest.15
In view of the pleiotropic actions of flavopiridol,18 it is difficult to identify with certainty the primary mechanism by which this agent interacts synergistically with bortezomib to trigger cell death in Bcr/Abl+ cells. Notably, flavopiridol alone, and particularly in combination with bortezomib, blocked phosphorylation of the carboxy-terminal domain (CTD) of RNA polymerase II. These findings are consistent with previous studies emphasizing that flavopiridol, by inhibiting the cyclinT/CDK9 complex (PTEFb),20,77 acts as a transcriptional repressor.78 It is important to note that potentiation of bortezomib lethality by flavopiridol was mimicked by DRB, an inhibitor of CTD phosphorylation.48,49 Collectively, these observations suggest that transcriptional repression by flavopiridol lowers the threshold for bortezomib-mediated lethality in Bcr/Abl+ leukemia cells. On the other hand, the possibility that the actions of flavopiridol as a pan-CDK inhibitor contribute to a diminished apoptotic threshold cannot be completely excluded.
While imatinib mesylate has had a major impact on the treatment of CML, the emergence or pre-existence of drug resistance (ie, through Bcr/Abl amplification or the development of Bcr/Abl kinase mutations) remains a continuing problem.13,71-73 This has prompted the search for new agents potentially active in such settings. Recent studies suggest that flavopiridol enhances imatinib mesylate lethality in leukemic cells exhibiting certain forms of imatinib mesylate resistance23 and indicate that bortezomib exhibits in vitro toxicity toward Bcr/Abl+ leukemia cells.29 Alternative approaches include the development of agents (eg, Hsp90 antagonists and histone deacetylase inhibitors) capable of down-regulating Bcr/Abl expression16,51,52 or inhibiting mutant Bcr/Abl kinase (eg, PD180970 and PD166326),65,79,80 as well as compounds capable of inactivating Src tyrosine kinases independent of Bcr/Abl (eg, CGP76030 and SKI-606).81,82 Such approaches may be particularly appropriate in the case of Bcr/Abl-independent forms of imatinib mesylate resistance associated with Lyn and Hck activation.15 For similar reasons, the ability of the bortezomib/flavopiridol regimen to (a) down-regulate Bcr/Abl expression and (b) inactivate Lyn and Hck kinases makes it an attractive candidate for further examination in CML and related Bcr/Abl+ hematologic malignancies, including those that have developed resistance to imatinib mesylate through established as well as more novel mechanisms.
Prepublished online as Blood First Edition Paper, March 23, 2004; DOI 10.1182/blood-2003-12-4121.
Supported by awards CA63753-05, CA83705, CA93738, and CA 100866 from the National Cancer Institute, National Institutes of Health (NIH); award 6045-03 from the Leukemia and Lymphoma Society of America; and award DAMD-17-03-1-0209 from the Department of Defense.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.