Abstract
Src homology 2 (SH2) domain-containing inositol-5-phosphatase 1 (SHIP1) plays important roles in negatively regulating the activation of immune cells primarily via the phosphoinositide 3-kinase (PI-3K) pathway by catalyzing the PI-3K product PtdIns-3,4,5P3 (phosphatidylinositol-3,4,5-triphosphate) into PtdIns-3,4P2. However, the role of SHIP1 in Toll-like receptor 4 (TLR4)-mediated lipopolysaccharide (LPS) response remains unclear. Here we demonstrate that SHIP1 negatively regulates LPS-induced inflammatory response via both phosphatase activity-dependent and -independent mechanisms in macrophages. SHIP1 becomes tyrosine phosphorylated and up-regulated upon LPS stimulation in RAW264.7 macrophages. SHIP1-specific RNA-interfering and SHIP1 overexpression experiments demonstrate that SHIP1 inhibits LPS-induced tumor necrosis factor α (TNF-α) and interleukin 6 (IL-6) production by negatively regulating the LPS-induced combination between TLR4 and myeloid differentiation factor 88 (MyD88); activation of Ras (p21ras protein), PI-3K, extracellular signal-regulated kinase 1/2 (ERK1/2), p38, and c-Jun NH2-terminal kinase (JNK); and degradation of IκB-α. SHIP1 also significantly inhibits LPS-induced mitogen-activated protein kinase (MAPK) activation in TLR4-reconstitited COS7 cells. Although SHIP1-mediated inhibition of PI-3K is dependent on its phosphatase activity, phosphatase activity-disrupted mutant SHIP1 remains inhibitory to LPS-induced TNF-α production. Neither disrupting phosphatase activity nor using the PI-3K pathway inhibitor LY294002 or wortmannin could significantly block SHIP1-mediated inhibition of LPS-induced ERK1/2, p38, and JNK activation and TNF-α production, demonstrating that SHIP1 inhibits LPS-induced activation of MAPKs and cytokine production primarily by a phosphatase activity- and PI-3K-independent mechanism. (Blood. 2005;105:4685-4692)
Introduction
Lipopolysaccharide (LPS; endotoxin) is a cell wall component of Gram-negative bacteria. LPS activates immune cells and triggers production of proinflammatory cytokines and other mediators, which up-regulate host immune defense systems and eliminate the bacterial infection.1 LPS hyporesponsive mice are susceptible to Gram-negative bacteria infection.2 On the other hand, excessive or prolonged production of LPS-induced mediators can result in septic shock, a life-threatening condition.1 However, a process, endotoxin tolerance, in which exposure to LPS renders immune cells tolerant to subsequent LPS stimulation, helps to keep responses to LPS under control.1,3 Endotoxin-tolerant macrophages, for instance, produce lower levels of the proinflammatory cytokines tumor necrosis factor α (TNF-α) and interleukin 6 (IL-6), both of which play important roles in septic shock.3 Little was known about the mechanism by which LPS interacts with immune cells until the Toll-like receptor (TLR) family was identified in mammalian cells.4,5 TLRs recognize conserved microbial components and function as critical sentinel receptors to initiate immune responses against microbial infections. TLR2, TLR4, and TLR9 recognize lipoteichoic acid, LPS, and the cytosine-phosphate-guanosine (CpG) motif of bacterial DNA, respectively. Given the important physiologic and pathologic relevance of LPS response, the mechanism of LPS-induced TLR4 signaling has been intensively studied but remains incompletely defined.4,5 Through recruitment of adaptor proteins such as myeloid differentiation factor 88 (MyD88) and TIR domain-containing adaptor inducing IFN-β (TRIF), TLR4 activates downstream mitogen-activated protein kinases (MAPKs), including extracellular signal-regulated kinase 1/2 (ERK1/2), p38, and c-Jun NH2-terminal kinase (JNK), and nuclear factor κ B (NF-κB). Activation of MAPKs and NF-κB represents the last events of cytoplasmic TLR4 signal transduction and is essential for LPS-induced production of proinflammatory cytokines.4,5 IL-1 receptor-associated kinase M (IRAK-M) and suppressor of cytokine signaling-1 function as negative regulators of TLR signal transduction and are considered as key molecules in the development of endotoxin tolerance.4-7 As such, these signaling molecules are targets for the modulation of LPS response. Identifying positive and negative regulators and the pathways of LPS signaling will provide insights into the mechanism of TLR signal transduction, rendering us the ability to finely orchestrate LPS- and other TLR agonist-induced responses so as to eliminate microbial infection while protecting against lethal host responses.
Src homology 2 (SH2) domain-containing inositol-5-phosphatase 1 (SHIP1) was initially identified as a 145-kDa protein that negatively regulated B-cell receptor signaling by catalyzing the phosphoinositide 3-kinase (PI-3K) product PtdIns-3,4,5P3 into PtdIns-3,4P2.8,9 SHIP1 also inhibits PI-3K activation induced by immunoglobulin E (IgE) and cytokines.10 In addition, SHIP1 can inhibit activation of ERK1/2, JNK, and NF-κB pathways.11-13 All of these pathways play important roles in LPS signaling4,5,14,15 ; however little is known about the role of SHIP1 as an important immune inhibitory molecule in LPS-induced inflammatory response.
We have investigated whether SHIP1 participates in LPS signaling in TLR4-reconstituted COS7 cells and the macrophage cell line RAW264.7. Unexpectedly, in addition to phosphatase activity-dependently inhibiting LPS-induced PI-3K activation, SHIP1 also phosphatase activity- and PI-3K-independently inhibits LPS-induced activation of MAPKs and the production of TNF-α. Our present study provides the first insight into the mechanism by which SHIP1 negatively regulates TLR4-mediated proinflammatory LPS response in a PI-3K-independent manner, suggesting that SHIP1 might be a potent candidate molecule for therapies aimed at manipulating LPS-induced inflammatory response.
Materials and methods
Reagents
LPS (0111:B4) was purchased from Sigma (St Louis, MO) and repurified as described previously.16 Antibodies specific to SHIP1, ERK1/2, p38, JNK, TLR4, MyD88, phospho-ERK1/2, phosphotyrosine, and horseradish peroxidase (HRP)-coupled secondary antibodies were obtained from Santa Cruz Biotechnology (Santa Cruz, CA). Antibodies specific to phospho-JNK and phospho-p38 were purchased from Promega (Madison, WI). LY294002, LY303511, wortmannin, and protease inhibitor cocktail were from Calbiochem (San Diego, CA).
Plasmid constructs
The expression vector pBK-CMV/150.8SHIP1 (SHIP1) was a kind gift from Dr L. R. Rohrschneider.8 A phosphatase activity-disrupted mutant SHIP1 (mu-SHIP1) construct was generated from pBK-CMV/150.8SHIP1 by converting P671A, D675A, and R676G using a Mutanbest Kit (TaKaRa, Dalian, China).17 Mutagenic primers are 5′-GTGCGCCGGAGTCCTCTGGA-3′ and 5′-CAGGACGCCAAGTTGTACTTCATCC-3′. The pBS-U6 (pBluescript-U6) plasmid was a gift from Dr Y. Shi.18 An RNA-interfering plasmid, pU6-SHIP1, containing a sequence matching SHIP1 cDNA (5′-GGAAGTCATCAGGACTCTGCA-3′) was constructed. The control vector pU6 contains a scrambled sequence (5′-TCAGTCACGTTAATGGTCGTT-3′) without known specificity. The expression vectors pEF-TLR4 and pEF-MD2 were kind gifts from Dr K. Miyake.19 CD14 cDNA was amplified from THP1 cells by reverse transcriptase-polymerase chain reaction and cloned into pcDNA3.1 expressing vector (Invitrogen, Carlsbad, CA). The primers used for CD14 amplification were 5′-ATCCGCTGTGTAGGAAAGAACGT-3′ and 5′-GGAATTCAGACAGGTCTAGGCTGGTAA-3′. The pGL3.5XκB-luciferase reporter plasmid was kindly provided by Seamus J. Martin.20 All constructs were confirmed by DNA sequencing.
Culture and transfection of RAW264.7 macrophages and COS7 cells
The murine macrophage cell line RAW 264.7 and monkey kidney cell line COS7 were obtained from the American Type Culture Collection (Manassas, VA) and cultured as described previously.21 For Western blotting, 2 × 106 cells, seeded into 60-mm dishes one day prior to transfection, were transfected with 5 μg DNA using Superfect Reagent (Qiagen, Hilden, Germany). For enzyme-linked immunosorbent assays (ELISAs), 2 × 105 cells were seeded into 24-well plates and incubated overnight before LPS stimulation. In some SHIP1 knockdown experiments the cells were cotransfected with a green fluorescence protein (GFP)-expressing plasmid (pGFP), and GFP-expressing cells were sorted with a FACSDiVa system (Becton Dickinson, San Jose, CA).22 SHIP1 stably transfected cells were selected with 300 μg/mL G418 (Invitrogen).
Detection of IL-6 and TNF-α
RAW264.7 macrophages were stimulated with 100 ng/mL LPS for indicated time periods. The concentrations of IL-6 and TNF-α in culture supernatants were measured using mouse IL-6 and mouse TNF-α ELISA Kits (R&D Systems, Minneapolis, MN) according to manufacturer's instructions.
Immunoprecipitation and Western blotting
Cells were lysed with M-PER Protein Extraction Reagent (Pierce, Rockford, IL) supplemented with protease inhibitor cocktail and protein concentrations of the extracts were measured by bicinchoninic acid (BCA) assay (Pierce). Forty micrograms of the protein was used either for immunoprecipitation or loaded per lane, subjected to sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE), transferred onto nitrocellulose membranes, then blotted as described previously.21
Assay of PI-3K activity
PI-3K activity was assayed with PI-3K ELISA kit (Echelon Biosciences, Salt Lake City, UT) according to manufacturer's instructions. In brief, cell lysates were prepared and PI-3K was immunoprecipitated with antibody against the p85 subunit and incubated with PI(4,5)P2 (phosphatidylinositol-4,5-diphosphate). The reaction products were incubated with a PI(3,4,5)P3 detector protein then added to a PI(3,4,5)P3-coated microplate for competitive binding. A peroxidase-linked secondary detection reagent and colorimetric detection were used to detect PI(3,4,5)P3 detector protein binding to the plate. The colorimetric signal was inversely proportional to the amount of PI(3,4,5)P3 produced by PI-3K activity.
Assay of Akt kinase activity
Akt (protein kinase B) activity was detected using Akt kinase Assay kit (Cell Signaling Technology, Beverly, MA) according to manufacturer's instructions. Briefly, cell lysates were prepared and immobilized Akt primary antibody was used to immunoprecipitate Akt from the extracts. Glycogen synthase kinase 3 (GSK-3) fusion protein (1 μg) was incubated with the precipitated protein in kinase buffer and then detected with phospho-glutathione-S-transferase 3 (phospho-GST-3)-specific antibody by Western blot. The phosphorylation level of GSK-3 fusion protein was proportional to Akt activity.
Ras activation assay
Ras activation was detected using Ras Activation Assay Kit (Upstate Biotechnology, Lake Placid, NY) according to the manufacturer's instructions. In brief, RAW264.7 cells were transfected and then stimulated with LPS as indicated. The cells were lysed with lysis buffer MLB, and protein concentrations of the extracts were measured using BCA Protein Assay kit (Pierce). Then 40 μg of lysate was incubated with GST fusion protein containing the Ras-binding domain of Raf (GST-Raf-RBD) for one hour at 4°C. Ras-guanosine triphosphate (Ras-GTP)-binding beads were pelleted by centrifuging at 14 000g for 3 minutes at 4°C. After 3 washes with MLB, the beads were boiled in SDS sample buffer for 5 minutes and separated on 15% SDS-PAGE. Ras-GTP was detected with anti-Ras antibody and HRP-conjugated secondary antibody and visualized with SuperSignal West Femto Maximum Sensitivity Substrate (Pierce).
Assay of luciferase reporter gene expression
RAW264.7 macrophages were cotransfected with the mixture of indicated pGL3-luciferase reporter plasmid, pRL-TK-Renilla-luciferase plasmid, and indicated amounts of SHIP1 expression construct. After 24 hours, the cells were left untreated or treated with LPS. Luciferase activities were measured using Dual-Luciferase Reporter Assay System (Promega) according to the manufacturer's instructions. Data are normalized for transfection efficiency by dividing Firefly luciferase activity with that of Renilla luciferase. The relative values are presented as fold increase over indicated control.
Densitometric analysis
Densitometric analysis was done with Labworks Image Acquisition and Analysis Software (UVP, Upland, CA). The background was subtracted, and the signals of the detected bands were normalized to the amount of loading control band. The relative values were presented as fold increase over control samples as indicated.
Statistical analysis
Statistical significance was determined by Student t test, with a value of P below .01 considered to be statistically significant.
Results
SHIP1 participates in LPS signaling and inhibits LPS-induced cytokine production in macrophages
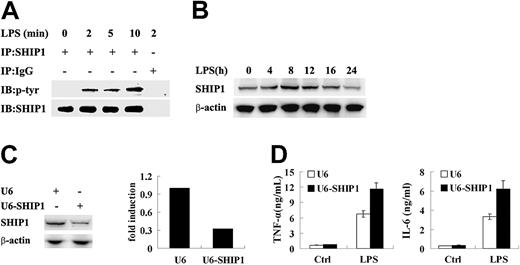
To study whether SHIP1 was involved in LPS signal transduction, we detected the phosphorylation of endogenous SHIP1 in RAW264.7 macrophages following LPS stimulation. As shown in Figure 1A, LPS stimulation prompted an increase in tyrosine phosphorylation of SHIP1 and the phosphorylation of SHIP1 was enhanced over time, suggesting SHIP1 might play a role in LPS signaling. In addition, the expression of SHIP1 was also upregulated, which increased at 4 hours and peaked at 8 to 12 hours after LPS stimulation (Figure 1B).
SHIP1 is phosphorylated upon LPS stimulation and inhibits LPS-induced inflammatory cytokine production by macrophages. (A) SHIP1 becomes phosphorylated following LPS stimulation in macrophages. RAW264.7 macrophages were treated with 100 ng/mL LPS for the indicated time periods, lysed, then anti-SHIP1 antibody or control isotype IgG were used to immunoprecipitate (IP) SHIP1 from the extracts. Expression of phosphorylated and total SHIP1 was detected using specific antibodies to phosphotyrosine or SHIP1, respectively, by Western blotting.;65IB indicates immunoblot; and p-, phosphorylated. (B) SHIP1 expression is up-regulated after LPS stimulation in macrophages. RAW264.7 macrophages were treated with 100 ng/mL LPS for the indicated time periods. Expression of SHIP1 was detected by Western blotting. (C) SHIP1-specific interfering RNA inhibits SHIP1 expression in macrophages. RAW264.7 macrophages were transfected with pGFP together with SHIP1 interfering RNA plasmid pU6-SHIP1 or control plasmid pU6. After 48 hours, GPF-expressing cells were sorted and SHIP1 expression was detected by Western blot. Densitometrically analyzed and normalized over β-actin signal in the respective lane, the relative expression level of SHIP1 in the control cells was expressed as 1. (D) SHIP1 knockdown increases LPS-induced inflammatory cytokine production by macrophages. RAW264.7 macrophages were transfected with pU6-SHIP1 or control plasmid pU6 and cultured for 48 hours and then stimulated with 100 ng/mL LPS for 8 hours. Concentrations of TNF-α and IL-6 in the supernatants were measured by ELISA. Ctrl indicates control. Data are shown as mean ± SD (n = 3) of one representative experiment; similar results were observed in 3 separate experiments.
SHIP1 is phosphorylated upon LPS stimulation and inhibits LPS-induced inflammatory cytokine production by macrophages. (A) SHIP1 becomes phosphorylated following LPS stimulation in macrophages. RAW264.7 macrophages were treated with 100 ng/mL LPS for the indicated time periods, lysed, then anti-SHIP1 antibody or control isotype IgG were used to immunoprecipitate (IP) SHIP1 from the extracts. Expression of phosphorylated and total SHIP1 was detected using specific antibodies to phosphotyrosine or SHIP1, respectively, by Western blotting.;65IB indicates immunoblot; and p-, phosphorylated. (B) SHIP1 expression is up-regulated after LPS stimulation in macrophages. RAW264.7 macrophages were treated with 100 ng/mL LPS for the indicated time periods. Expression of SHIP1 was detected by Western blotting. (C) SHIP1-specific interfering RNA inhibits SHIP1 expression in macrophages. RAW264.7 macrophages were transfected with pGFP together with SHIP1 interfering RNA plasmid pU6-SHIP1 or control plasmid pU6. After 48 hours, GPF-expressing cells were sorted and SHIP1 expression was detected by Western blot. Densitometrically analyzed and normalized over β-actin signal in the respective lane, the relative expression level of SHIP1 in the control cells was expressed as 1. (D) SHIP1 knockdown increases LPS-induced inflammatory cytokine production by macrophages. RAW264.7 macrophages were transfected with pU6-SHIP1 or control plasmid pU6 and cultured for 48 hours and then stimulated with 100 ng/mL LPS for 8 hours. Concentrations of TNF-α and IL-6 in the supernatants were measured by ELISA. Ctrl indicates control. Data are shown as mean ± SD (n = 3) of one representative experiment; similar results were observed in 3 separate experiments.
The effects of SHIP1 knockdown on LPS-induced production of TNF-α and IL-6 in RAW264.7 cells were investigated. The cells were transfected with pGFP together with the SHIP1 RNA-interfering plasmid pU6-SHIP1 or control plasmid pU6. After they were cultured for 48 hours, GFP-expressing cells were sorted, and the expression level of SHIP1 in the cells was detected. As shown in Figure 1C, SHIP1 RNA interfering inhibited endogenous SHIP1 expression by approximately 65% in RAW264.7 macrophages. The pU6-SHIP1- or control plasmid pU6-transfected cells were stimulated with LPS, and production of TNF-α and IL-6 in the cells was detected. SHIP1 knockdown cells produced 1.7-fold TNF-α and 1.9-fold IL-6 of that produced by mock-transfected cells (P < .01 for U6 vs U6-SHIP1) upon LPS stimulation (Figure 1D), demonstrating that SHIP1 could inhibit LPS-induced inflammatory response in macrophages.
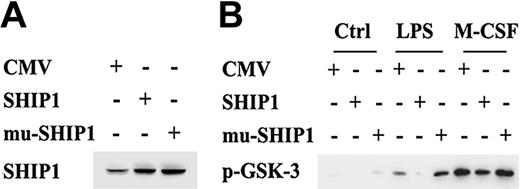
SHIP1 negatively regulates LPS-induced activations of the PI-3K pathway in a phosphatase activity-dependent manner in macrophages. (A) Wild-type SHIP1 and mutant SHIP1 were overexpressed in stably transfected RAW264.7 cells. RAW264.7 macrophages were stably transfected with empty pBK-CMV control plasmid, wild-type SHIP1, or phosphatase-inactive SHIP1 plasmid. Expressions of SHIP1 in the cells were detected with SHIP1 antibody. (B) Overexpression of wild-type SHIP1 and phosphatase-inactive SHIP1 differently affect Akt activity in macrophages. RAW264.7 macrophages were stably transfected with empty pBK-CMV control plasmid, wild-type SHIP1, or phosphatase-inactive SHIP1 plasmid. The cells were stimulated for 10 minutes with 100 ng/mL LPS, 100 ng/mL M-GSF, or left unstimulated and then cell extracts were prepared. Akt activity was assayed as described in “Materials and methods,” under “Assay of Akt kinase activity.” Similar results were observed in 3 separate experiments.
SHIP1 negatively regulates LPS-induced activations of the PI-3K pathway in a phosphatase activity-dependent manner in macrophages. (A) Wild-type SHIP1 and mutant SHIP1 were overexpressed in stably transfected RAW264.7 cells. RAW264.7 macrophages were stably transfected with empty pBK-CMV control plasmid, wild-type SHIP1, or phosphatase-inactive SHIP1 plasmid. Expressions of SHIP1 in the cells were detected with SHIP1 antibody. (B) Overexpression of wild-type SHIP1 and phosphatase-inactive SHIP1 differently affect Akt activity in macrophages. RAW264.7 macrophages were stably transfected with empty pBK-CMV control plasmid, wild-type SHIP1, or phosphatase-inactive SHIP1 plasmid. The cells were stimulated for 10 minutes with 100 ng/mL LPS, 100 ng/mL M-GSF, or left unstimulated and then cell extracts were prepared. Akt activity was assayed as described in “Materials and methods,” under “Assay of Akt kinase activity.” Similar results were observed in 3 separate experiments.
SHIP1 negatively regulates LPS-induced activation of the PI-3K pathway in a phosphatase activity-dependent manner in macrophages
The PI-3K pathway, the main target of SHIP1 in a variety of cell responses, plays an important role in LPS signaling. To investigate the role of SHIP1 in LPS-induced PI-3K activation, we established wild-type and mu-SHIP1 stably transfected cell lines. The mu-SHIP1 was constructed by introducing mutations of P671A, D675A, and R676G in the catalytic domain of SHIP1, which disrupted SHIP1's phosphatase activity.17 Western blot results showed that SHIP1 was overexpressed in both wild-type and mutant plasmid-transfected cells (Figure 2A). As shown in Figure 2B, wild-type SHIP1 inhibited LPS-induced activation of Akt, a PI-3K downstream molecule that is activated upon binding to PI(3,4,5)P3. On the contrary, mu-SHIP1 enhanced LPS-induced Akt activation. SHIP1 negatively regulates macrophage colony-stimulating factor (M-CSF)-induced PI-3K-dependent Akt activation through its phosphatase activity.23,24 Consistent with previous studies, while overexpression of wild-type SHIP1 inhibited M-CSF-induced Akt activation, overexpression of mu-SHIP1 enhanced M-CSF-induced Akt activation (Figure 2B), providing further evidence that the mutations disrupted the phosphatase activity of SHIP1 in our study. Similar results were obtained in 3 independently established cell lines. These results demonstrate that SHIP1 negatively regulates the LPS-induced PI-3K pathway activation in macrophages in a phosphatase activity-dependent manner.
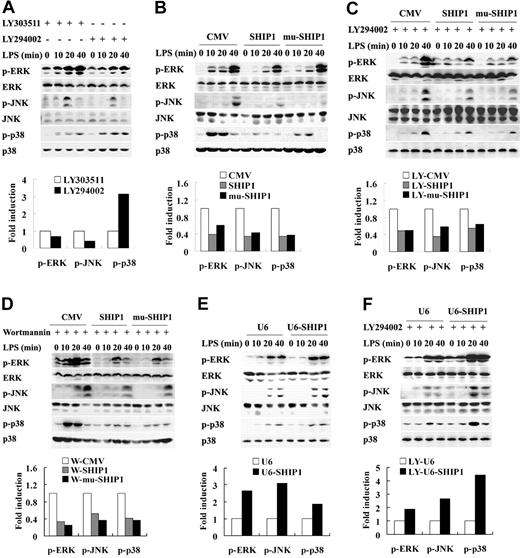
SHIP1 negatively regulates LPS-induced activation of MAPKs primarily via a phosphatase activity- and PI-3K-independent mechanism in macrophages
PI-3K promotes LPS-induced NF-κB activation in RAW264.7 macrophages.14 Our experiments demonstrate that this is also the case for LPS-induced ERK1/2 and JNK1/2 activation, which was strongly inhibited by the PI-3K-specific inhibitor LY294002 (Figure 3A). In contrast, LPS-induced p38 phosphorylation was enhanced by LY294002 treatment (Figure 3A), which was consistent with the previously reported inhibitory role of PI-3K in LPS-induced p38 activation in dendritic cells.15
We next investigated whether SHIP1 regulated LPS-induced activation of MAPKs through the PI-3K pathway. Unlike LY294002 treatment, SHIP1 overexpression not only inhibited LPS-induced ERK1/2 and JNK activation but also inhibited LPS-induced p38 MAPK activation (Figure 3B). The contrary effects of SHIP1 overexpression and LY294002 treatment on LPS-induced p38 activation suggested that SHIP1 might regulate LPS-induced p38 activation primarily via an alternative PI-3K-independent pathway. Consistently, phosphatase-inactive mu-SHIP1 could also inhibit LPS-induced ERK1/2, p38, and JNK activation, suggesting that SHIP1 regulates LPS-induced activation of MAPKs primarily via a phosphatase activity- and PI-3K-independent pathway. To confirm the conclusion, the PI-3K inhibitor LY294002 and wortmannin were used to inhibit PI-3K activation. As shown in Figure 3C-D, neither of them could efficiently diminish wild-type and mutant SHIP1-mediated inhibition of LPS-induced ERK1/2, p38, or JNK activation.
We further observed the effect of SHIP1 knockdown on LPS-induced activation of ERK1/2, p38, and JNK. Consistent with the above results, LPS-induced phosphorylation of ERK1/2, p38, and JNK was significantly enhanced in SHIP1 knockdown cells compared with that in control cells, in spite of the absence or presence of LY294002 (Figure 3E-F), demonstrating that SHIP1 regulates LPS-induced activation of MAPKs primarily by a PI-3K-independent mechanism in macrophages.
SHIP1 inhibits LPS-induced activation of MAPKs primarily via a phosphatase activity- and PI-3K-independent mechanism in macrophages. (A) LY294002 affects LPS-induced activation of MAPKs in macrophages. RAW264.7 macrophages were pretreated with 30 μM LY303511 or 30 μM LY294002 for 40 minutes and then stimulated with 100 ng/mL LPS for the indicated time periods. The phosphorylation of ERK1/2, p38, and JNK were detected by Western blot. Phosphorylation levels of the proteins at the time point of 20 minutes after LPS stimulation were quantitated by measuring band intensities. The values were normalized to the total ERK, p38, or JNK signal, respectively. Relative phosphorylation levels of the proteins in the control cells were expressed as 1. (B) Overexpression of wild-type SHIP1 or phosphatase activity-disrupted mutant SHIP1 inhibits LPS-induced activation of MAPKs in macrophages. RAW264.7 macrophages were transiently transfected with control plasmid, wild-type SHIP1, or mutant SHIP1 and cultured for 24 hours. The cells were stimulated with 100 ng/mL LPS for the indicated time periods. The phosphorylation of ERK1/2, p38, and JNK were detected and shown as described in panel A. (C-D) Overexpression of wild-type SHIP1 or phosphatase activity-disrupted mutant SHIP1 inhibits LPS-induced activation of MAPKs in the presence of PI-3K inhibitor in macrophages. Control plasmid, wild-type SHIP1, or phosphatase-inactive mutant SHIP1-transfected RAW264.7 macrophages were pretreated with (C) 30 μM LY294002 (LY) or (D) 100 nM wortmannin (W) for 40 minutes and then stimulated with 100 ng/mL LPS for the indicated time periods. The phosphorylation of ERK1/2, p38, and JNK was detected and shown as described in panel A. (E) SHIP1 RNA interfering enhances LPS-induced activation of MAPKs in macrophages. RAW264.7 macrophages were transfected with pU6-SHIP1 or control plasmid and cultured for 48 hours. The cells were stimulated with 100 ng/mL LPS for the indicated time periods. The phosphorylation of ERK1/2, p38, and JNK were detected and shown as described in panel A. (F) SHIP1 RNA interfering enhances LPS-induced activations of MAPKs in the presence of LY294002 in macrophages. RAW264.7 macrophages were transfected and cultured as described in panel E. All of the cells were pretreated with 30 μM LY294002 for 40 minutes and then stimulated with 100 ng/mL LPS for the indicated time periods. The phosphorylation of ERK1/2, p38, and JNK were detected by Western blotting, densitometrically analyzed, and presented as described in panel A. Similar results were observed in 3 separate experiments.
SHIP1 inhibits LPS-induced activation of MAPKs primarily via a phosphatase activity- and PI-3K-independent mechanism in macrophages. (A) LY294002 affects LPS-induced activation of MAPKs in macrophages. RAW264.7 macrophages were pretreated with 30 μM LY303511 or 30 μM LY294002 for 40 minutes and then stimulated with 100 ng/mL LPS for the indicated time periods. The phosphorylation of ERK1/2, p38, and JNK were detected by Western blot. Phosphorylation levels of the proteins at the time point of 20 minutes after LPS stimulation were quantitated by measuring band intensities. The values were normalized to the total ERK, p38, or JNK signal, respectively. Relative phosphorylation levels of the proteins in the control cells were expressed as 1. (B) Overexpression of wild-type SHIP1 or phosphatase activity-disrupted mutant SHIP1 inhibits LPS-induced activation of MAPKs in macrophages. RAW264.7 macrophages were transiently transfected with control plasmid, wild-type SHIP1, or mutant SHIP1 and cultured for 24 hours. The cells were stimulated with 100 ng/mL LPS for the indicated time periods. The phosphorylation of ERK1/2, p38, and JNK were detected and shown as described in panel A. (C-D) Overexpression of wild-type SHIP1 or phosphatase activity-disrupted mutant SHIP1 inhibits LPS-induced activation of MAPKs in the presence of PI-3K inhibitor in macrophages. Control plasmid, wild-type SHIP1, or phosphatase-inactive mutant SHIP1-transfected RAW264.7 macrophages were pretreated with (C) 30 μM LY294002 (LY) or (D) 100 nM wortmannin (W) for 40 minutes and then stimulated with 100 ng/mL LPS for the indicated time periods. The phosphorylation of ERK1/2, p38, and JNK was detected and shown as described in panel A. (E) SHIP1 RNA interfering enhances LPS-induced activation of MAPKs in macrophages. RAW264.7 macrophages were transfected with pU6-SHIP1 or control plasmid and cultured for 48 hours. The cells were stimulated with 100 ng/mL LPS for the indicated time periods. The phosphorylation of ERK1/2, p38, and JNK were detected and shown as described in panel A. (F) SHIP1 RNA interfering enhances LPS-induced activations of MAPKs in the presence of LY294002 in macrophages. RAW264.7 macrophages were transfected and cultured as described in panel E. All of the cells were pretreated with 30 μM LY294002 for 40 minutes and then stimulated with 100 ng/mL LPS for the indicated time periods. The phosphorylation of ERK1/2, p38, and JNK were detected by Western blotting, densitometrically analyzed, and presented as described in panel A. Similar results were observed in 3 separate experiments.
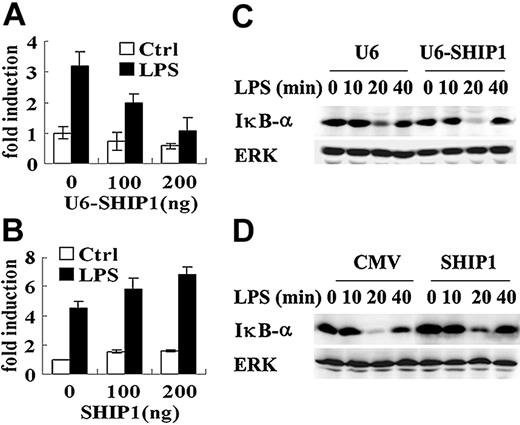
SHIP1 inhibits LPS-induced IκB-α degradation but enhances NF-κB activation in macrophages
The NF-κB pathway plays an important role in TLR4 signal transduction. We investigated the role of SHIP1 in NF-κB activation by detecting NF-κB luciferase reporter gene expression. Unexpectedly, SHIP1 knockdown dose-dependently inhibited LPS-induced NF-κB activation (Figure 4A). Consistently, SHIP1 overexpression dose-dependently enhanced LPS-induced NF-κB activation (Figure 4B). We also detected LPS-induced NF-κB luciferase activity in SHIP1 or control vector stably transfected RAW264.7 macrophages. SHIP1 stable overexpression also increased LPS-induced NF-κB luciferase activity (data not shown). We further observed the effect of SHIP1 knockdown on LPS-induced IκB-α degradation. While SHIP1 knockdown enhanced LPS-induced IκB-α degradation (Figure 4C), SHIP1 overexpression inhibited LPS-induced IκB-α degradation (Figure 4D). These results suggest that SHIP1 positively regulates LPS-induced NF-κB activation through an IκB-α-independent mechanism.
SHIP1 inhibits LPS-induced IκB-α degradation but enhances NF-κB activation in macrophages. (A-B) SHIP1 increases LPS-induced NF-κB reporter gene expression. RAW264.7 macrophages in 24-well plates were transiently cotransfected with 100 ng of pGL3.5XκB-luciferase, 10 ng of pTK-Renilla-luciferase, and 0, 100, and 200 ng of pU6-SHIP1 (A) or SHIP1 (B). Total amounts of plasmid DNA were equalized using corresponding control vector. After 48 hours (A) or 24 hours (B) of culture, the cells were stimulated with 100 ng/mL LPS for 6 hours. NF-κB luciferase activity was measured using theDual-Luciferase Reporter Assay System, normalized by Renilla luciferase activity, expressed as fold induction relative to the activity in unstimulated cells transfected with control vector. Data are shown as mean ± SD (n = 3) of one typical experiment. (C-D) SHIP1 inhibits LPS-induced IκB-α degradation in macrophages. RAW264.7 macrophages were transfected with pU6-SHIP1 or control pU6 plasmid and cultured for 48 hours (C) or transfected with SHIP1 or control pBK-CMV plasmid and cultured for 24 hours (D). The cells were stimulation with 100 ng/mL LPS for the indicated time periods. The degradation of IκB-α was detected by Western blotting. Similar results were observed in 3 separate experiments.
SHIP1 inhibits LPS-induced IκB-α degradation but enhances NF-κB activation in macrophages. (A-B) SHIP1 increases LPS-induced NF-κB reporter gene expression. RAW264.7 macrophages in 24-well plates were transiently cotransfected with 100 ng of pGL3.5XκB-luciferase, 10 ng of pTK-Renilla-luciferase, and 0, 100, and 200 ng of pU6-SHIP1 (A) or SHIP1 (B). Total amounts of plasmid DNA were equalized using corresponding control vector. After 48 hours (A) or 24 hours (B) of culture, the cells were stimulated with 100 ng/mL LPS for 6 hours. NF-κB luciferase activity was measured using theDual-Luciferase Reporter Assay System, normalized by Renilla luciferase activity, expressed as fold induction relative to the activity in unstimulated cells transfected with control vector. Data are shown as mean ± SD (n = 3) of one typical experiment. (C-D) SHIP1 inhibits LPS-induced IκB-α degradation in macrophages. RAW264.7 macrophages were transfected with pU6-SHIP1 or control pU6 plasmid and cultured for 48 hours (C) or transfected with SHIP1 or control pBK-CMV plasmid and cultured for 24 hours (D). The cells were stimulation with 100 ng/mL LPS for the indicated time periods. The degradation of IκB-α was detected by Western blotting. Similar results were observed in 3 separate experiments.
SHIP1 inhibits LPS-induced TNF-α production by both phosphatase activity-dependent and -independent mechanisms in macrophages
To confirm the roles of SHIP1's phosphatase activity and the PI-3K pathway in SHIP1-mediated inhibition of LPS-induced inflammatory response, we compared the effects of wild-type SHIP1 and phosphatase-inactive mu-SHIP1 expression on LPS-induced TNF-α production. RAW264.7 macrophages stably transfected with SHIP1, mu-SHIP1 plasmid, or control vector were stimulated with LPS. As shown in Figure 5A, both wild-type SHIP1 and mu-SHIP1 expression inhibited LPS-induced TNF-α production. However, disruption of SHIP1's phosphatase activity partially blocked the decrease in TNF-α production. Similar results were obtained in 3 independently established cell lines. These results provided further evidences that SHIP1 inhibited LPS-induced proinflammatory response by both phosphatase activity-dependent and -independent mechanisms.
We also observed whether the PI-3K inhibitor LY294002 or wortmannin could affect SHIP1-mediated inhibition of LPS-induced TNF-α production. SHIP1 or mock-transfected RAW264.7 macrophages were stimulated with LPS in the presence of dimethyl sulfoxide (DMSO), LY303511, LY294002, or wortmannin, and TNF-α production in the supernatants was quantified (Figure 5B). Consistent with previous studies, LY294002 could partially inhibit LPS-induced TNF-α production, but wortmannin did not inhibit TNF-α production.14 However, neither of them could significantly diminish SHIP-mediated inhibition of TNF-α production. PI-3K activity assay showed that LY294002 and wortmannin used in the experiments were effective in blocking PI-3K activation (Figure 5C). These results suggest that the PI-3K-independent pathway functions in SHIP1-mediated inhibition of LPS-induced inflammatory response.
SHIP1 inhibits LPS-induced TNF-α production primarily via a phosphatase activity- and PI-3K-independent mechanism in macrophages. (A) Overexpression of wild-type SHIP1 and phosphatase activity-disrupted mutant SHIP1 inhibits LPS-induced TNF-α production in macrophages. RAW264.7 macrophages (2 × 105) stably transfected with control vector, SHIP1 plasmid, or mutant SHIP1 were stimulated with 100 ng/mL LPS for 8 hours or left unstimulated; concentrations of TNF-α in the supernatants were measured by ELISA. (B) SHIP1 inhibits LPS-induced TNF-α production in the presence of PI-3K inhibitors in macrophages. RAW264.7 macrophages (2 × 105) stably transfected with control vector or SHIP1 plasmid were stimulated with 100 ng/mL LPS in the presence of DMSO, 100 ng/mL wortmannin, 30 μM LY303511, or 30 μM LY294002 for 8 hours, then concentrations of TNF-α in the supernatants were measured by ELISA. (C) LY294002 and wortmannin sufficiently inhibit PI-3K activity in macrophages. RAW264.7 macrophages were pretreated with 30 μM LY294002 (also included in the enzyme reaction), 100 nM wortmannin for 40 minutes, or left untreated. Then the cells were stimulated with 1 μg/mL LPS for 10 minutes. PI-3K activity in the cells was assayed as described in “Materials and methods,” under “Assay of PI-3K activity.” For LY294002-treated cells, LY294002 was also added to the reaction mixture. The amount of PI(3,4,5)P3 produced in the reactions was proportional to PI-3K activity. Data are shown as mean ± SD (n = 3) of one typical experiment. Similar results were observed in 3 separate experiments.
SHIP1 inhibits LPS-induced TNF-α production primarily via a phosphatase activity- and PI-3K-independent mechanism in macrophages. (A) Overexpression of wild-type SHIP1 and phosphatase activity-disrupted mutant SHIP1 inhibits LPS-induced TNF-α production in macrophages. RAW264.7 macrophages (2 × 105) stably transfected with control vector, SHIP1 plasmid, or mutant SHIP1 were stimulated with 100 ng/mL LPS for 8 hours or left unstimulated; concentrations of TNF-α in the supernatants were measured by ELISA. (B) SHIP1 inhibits LPS-induced TNF-α production in the presence of PI-3K inhibitors in macrophages. RAW264.7 macrophages (2 × 105) stably transfected with control vector or SHIP1 plasmid were stimulated with 100 ng/mL LPS in the presence of DMSO, 100 ng/mL wortmannin, 30 μM LY303511, or 30 μM LY294002 for 8 hours, then concentrations of TNF-α in the supernatants were measured by ELISA. (C) LY294002 and wortmannin sufficiently inhibit PI-3K activity in macrophages. RAW264.7 macrophages were pretreated with 30 μM LY294002 (also included in the enzyme reaction), 100 nM wortmannin for 40 minutes, or left untreated. Then the cells were stimulated with 1 μg/mL LPS for 10 minutes. PI-3K activity in the cells was assayed as described in “Materials and methods,” under “Assay of PI-3K activity.” For LY294002-treated cells, LY294002 was also added to the reaction mixture. The amount of PI(3,4,5)P3 produced in the reactions was proportional to PI-3K activity. Data are shown as mean ± SD (n = 3) of one typical experiment. Similar results were observed in 3 separate experiments.
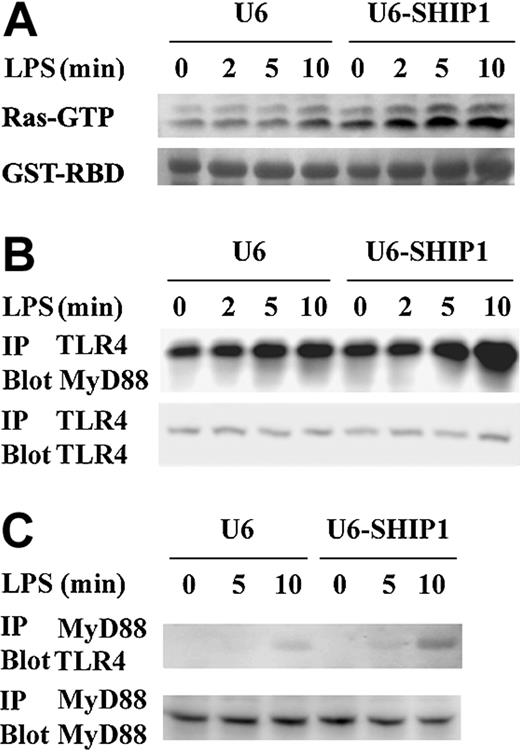
SHIP1 inhibits LPS-induced Ras activation and TLR4-MyD88 complex formation
Ras is an important signal intermediator in the activation of immune cells and can be inhibited by SHIP1 in a PI-3K-independent manner.10 To further illuminate the mechanisms by which SHIP1 negatively regulates LPS response, LPS-induced Ras activation was detected in SHIP1 knockdown cells. As shown in Figure 6A, LPS treatment activated Ras over time. Compared with mock transfection, SHIP1 RNA interfering significantly enhanced LPS-induced Ras activation.
Recruitment of MyD88 to TLR4 is required for LPS signaling. We investigated the effect of SHIP1 knockdown on the LPS-induced TLR4-MyD88 combination by immunoprecipitation. As shown in Figure 6B-C, LPS treatment promoted the TLR4-MyD88 combination. Compared with mock transfection, SHIP1 RNA interfering significantly enhanced the LPS-induced TLR4-MyD88 combination.
SHIP1 inhibits LPS-induced Ras activation and the TLR4-MyD88 combination in macrophages. (A) SHIP1 knockdown enhances LPS-induced Ras activation in macrophages. RAW264.7 macrophages were transfected with pU6-SHIP1 or control pU6 plasmid and cultured for 48 hours. The cells were treated with 100 ng/mL LPS for the indicated time periods; Ras activation was assayed as described in “Materials and methods.” The gel was stained with Coomassie blue to show equal protein loading (GST-RBD). Similar results were observed in 3 separate experiments. (B-C) SHIP1 knockdown enhances the LPS-induced TLR4-MyD88 combination in macrophages. RAW264.7 macrophages were transfected with pU6-SHIP1 or control pU6 plasmid and cultured for 48 hours. The cells were stimulated with 100 ng/mL LPS for the indicated time periods; the TLR4-MyD88 complex was precipitated with antibody against to TLR4 (C) or MyD88 (D) and detected as described in “Materials and methods.” Similar results were observed in 3 separate experiments.
SHIP1 inhibits LPS-induced Ras activation and the TLR4-MyD88 combination in macrophages. (A) SHIP1 knockdown enhances LPS-induced Ras activation in macrophages. RAW264.7 macrophages were transfected with pU6-SHIP1 or control pU6 plasmid and cultured for 48 hours. The cells were treated with 100 ng/mL LPS for the indicated time periods; Ras activation was assayed as described in “Materials and methods.” The gel was stained with Coomassie blue to show equal protein loading (GST-RBD). Similar results were observed in 3 separate experiments. (B-C) SHIP1 knockdown enhances the LPS-induced TLR4-MyD88 combination in macrophages. RAW264.7 macrophages were transfected with pU6-SHIP1 or control pU6 plasmid and cultured for 48 hours. The cells were stimulated with 100 ng/mL LPS for the indicated time periods; the TLR4-MyD88 complex was precipitated with antibody against to TLR4 (C) or MyD88 (D) and detected as described in “Materials and methods.” Similar results were observed in 3 separate experiments.
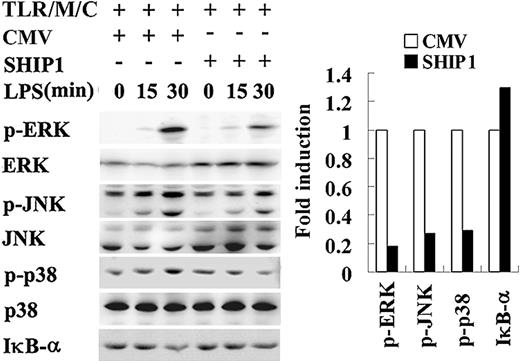
SHIP1 inhibits LPS-induced MAPKs activation in TLR4-reconstituted COS7 cells
As repurified LPS activates macrophages exclusively through TLR4,25 the aforementioned results suggest that SHIP1 might be an inhibitory regulator of TLR4-mediated LPS response. We used TLR4-reconstituted COS7 cells to confirm that SHIP1 targeted to TLR4 signaling. LPS could not induce detectable phosphorylation of MAPKs in COS7 cells (data not shown), which was consistent with a previous report that COS7 cells did not express TLR4 and were irresponsive to LPS stimulation.26 We established TLR4-reconstituted COS7 cells by transfecting the cells with constructs expressing TLR4, MD2, and CD14, all of which were required for TLR4-mediated LPS signaling, together with wild-type SHIP1 plasmid or control empty vector. As shown in Figure 7, LPS-induced phosphorylation of ERK1/2, p38, and JNK was significantly inhibited in the cells transfected with SHIP1 compared with the cells transfected with control empty vector, further demonstrating that SHIP1 negatively regulates TLR4-mediated LPS signaling.
Discussion
In this study, we demonstrated that SHIP1 was phosphorylated and then up-regulated upon LPS stimulation and could inhibit LPS-induced activation of MAPKs and production of proinflammatory cytokines in macrophages. Kinetic studies demonstrated that the up-regulation of SHIP1 was much later compared with the phosphorylation of SHIP1, suggesting that the phosphorylation of SHIP1 could not be attributed to the up-regulation of SHIP1 expression. Recent studies suggested that SHIP1's 5-phosphatase activity appears not to change following extracellular stimulation and subsequent tyrosine phosphorylation.27 LPS-induced phosphorylation might not influence the phosphatase activity of SHIP1. However, the change in the phosphorylation level of SHIP1 suggested that SHIP1 was involved in LPS signaling and might function as a negative regulator of LPS-induced inflammatory response in RAW264.7 macrophages.
SHIP1 overexpression inhibited Akt activity not only in resting cells but also in LPS-stimulated cells and the inhibition was dependent on the integrality of SHIP1's phosphatase catalytic domain, suggesting that SHIP1 negatively regulates LPS-induced activation of the PI-3K pathway through its phosphatase activity. However, disruption of the phosphatase activity of SHIP1 did not reverse its inhibitory regulation of MAPK activation and TNF-α production. Consistently, both LY294002 and wortmannin, which sufficiently inhibited LPS-induced PI-3K activity, could not significantly diminish SHIP1-mediated inhibition of LPS-induced MAPK activation and cytokine production, indicating that phosphatase activity of SHIP1 and the inhibition of PI-3K activation do not play predominant roles in SHIP1-mediated inhibition of LPS-induced inflammatory response in RAW264.7 macrophages.
SHIP1 inhibits LPS-induced MAPKs activation in TLR4-reconstituted COS7 cells. COS7 cells were cotransfected with 1 μg TLR4, 1 μg MD2, and 1 μg CD14 plasmids (TLR/M/C) to establish TLR4-reconstituted cells. Together with TLR/M/C plasmids, the cells were also transfected with 2 μg pBK-CMV/150.8SHIP1 (SHIP1) or its control empty vector pBK-CMV (CMV) and cultured for 48 hours. The cells were stimulated with 100 ng/mL LPS for the indicated time periods. The phosphorylation of ERK1/2, p38, JNK, and degradation of IκB-α were detected by Western blotting. Similar results were observed in 3 separate experiments.
SHIP1 inhibits LPS-induced MAPKs activation in TLR4-reconstituted COS7 cells. COS7 cells were cotransfected with 1 μg TLR4, 1 μg MD2, and 1 μg CD14 plasmids (TLR/M/C) to establish TLR4-reconstituted cells. Together with TLR/M/C plasmids, the cells were also transfected with 2 μg pBK-CMV/150.8SHIP1 (SHIP1) or its control empty vector pBK-CMV (CMV) and cultured for 48 hours. The cells were stimulated with 100 ng/mL LPS for the indicated time periods. The phosphorylation of ERK1/2, p38, JNK, and degradation of IκB-α were detected by Western blotting. Similar results were observed in 3 separate experiments.
LPS-induced Ras activation can be inhibited by SHIP1. In addition to functioning as a phosphatase, SHIP1 also competes with growth factor receptor-bound protein 2 (Grb2) for src homologous and collagen gene (Shc) and thereby PI-3K-independently inhibits Ras activation.10 The inhibition of Ras activation might be a possible PI-3K-independent pathway that SHIP1 employs to negatively regulate LPS response. However, LPS did not induce a detectable Shc-SHIP1 combination in our immunoprecipitation experiments to explore the upstream events that lead to the inhibition of Ras. Instead, SHIP1 knockdown enhanced the LPS-induced TLR4-MyD88 combination, a proximate signal event in LPS signaling. Upon LPS stimulation, TLR4 and MyD88 translocate into lipid rafts.28,29 SHIP1 also translocates into lipid rafts following LPS treatment.30 It is intriguing to suspect whether SHIP1 could inhibit the translocation of TLR4 and MyD88 into a lipid raft or whether SHIP1 could inhibit the combination between TLR4 and MyD88 in a lipid raft by a competitive mechanism. We sought to identify the association between endogenous SHIP1 and the intermediates involved in TLR4 signal transduction following LPS stimulation. However, we failed to detect the known intermediates including MyD88, IRAK1, and tumor necrosis factor receptor-associated factor 6 (TRAF6) in immunocoprecipitation experiments using a SHIP1-specific antibody (data not shown). Translocation to membrane was reported to be essential for the regulatory activity of SHIP1.31,32 In this case, identification of specific and direct interactions between SHIP1 and the intermediates might be difficult.32
In TLR4 signal transduction, PI-3K is activated downstream of MyD88.14 SHIP1 might PI-3K-independently block LPS signaling through inhibiting the TLR4-MyD88 combination. In IL-1β signal transduction, Ras is activated downstream of MyD88 and IRAK1.33 Our previous study showed that Ras activation promotes IRAK1-TRAF6 complex formation and thereby enhances TLR9 signal transduction in RAW264.7 macrophages.21 However, it remains unclear whether Ras activation is dependent on the TLR4-MyD88 combination in TLR signaling. Further study will determine whether the activation of Ras is MyD88 dependent in TLR4 and TLR9 signal transduction.
During the review of the manuscript, 2 groups reported that SHIP1 could regulate LPS-induced inflammatory response.30,34 Sly et al34 reported that LPS-induced ERK1/2 and Akt phosphorylation as well as cytokine production was enhanced in SHIP1-/- BMmφ cells. Inconsistent with our results observed in RAW264.7 macrophages, the enhancement in TNF-α production could be efficiently blocked by LY294002 and wortmannin in SHIP1-/- BMmφ cells.34 The discrepancy might be due to the fact that the pharmacologic functions of LY294002 and wortmannin are different in the cells used in the 2 studies. Ly294002 and wortmannin completely blocked LPS-induced TNF-α production in SHIP1-/- BMmφ cells rather than diminished SHIP1 deficiency-mediated enhancement of TNF-α production.34 However, Ly294002 can only partially inhibit LPS-induced TNF-α production, and wortmannin cannot affect LPS-induced TNF-α production in RAW264.7 cells, as shown in our experiments and by another group.14
In another study, Fang et al30 reported that SHIP1 up-regulated LPS-induced inflammatory response by showing that LPS-induced NF-κB-dependent gene transcription was up-regulated in SHIP1-overexpressing RAW264.7 cells, and LPS-induced ERK1/2 and Akt phosphorylation as well as TNF-α production was inhibited in SHIP1-/- BMmφ cells. The controversial results concerning the activation of ERK1/2 and Akt and the production of TNF-α might be due to the fact that differently prepared LPSs were used in these studies and that contaminant agonists of other TLRs in commercially obtained LPS might lead to different results. In fact, we found that SHIP1 could positively regulate the signal transduction induced by some other TLR agonists in our experiments (data not shown). However, consistent with data by Fang et al,30 we also observed that SHIP1 did not inhibit LPS-induced NF-κB activation in macrophages as revealed by increased luciferase reporter gene expression. In TLR signaling, MAPKs and IκB-α pathways lie downstream of the MyD88-IRAK1-TRAF6 cascade. The activation of the MyD88-IRAK1-TRAF6 cascade leads to MAPK activation and IκB-α degradation. In resting cells, IκB-α binds to the NF-κB p65 subunit and blocks its nuclear translocation. Upon activation, IκB-α is degraded and the NF-κB p65 subunit is released. As an NF-κB target gene itself, IκB-α is rapidly resynthesized and functions as a fast feedback down-regulator of NF-κB activation. We further investigated the effect of SHIP1 expression on LPS-induced IκB-α degradation. IκB-α was degraded within 20 minutes and significantly resynthesized within 40 minutes after LPS stimulation, as observed previously by another group in RAW264.7 macrophages.35 Interestingly, SHIP1 expression inhibited LPS-induced IκB-α degradation in the cells, suggesting that SHIP1 enhances LPS-induced NF-κB activity by an alternative mechanism rather than IκB-α degradation. In addition to IκB-α degradation, several other pathways can regulate the activation of NF-κB. For example, the phosphorylation of the NF-κB subunit contributes to trans-activation of NF-κB.36 A recent study demonstrated that proteasome-mediated NF-κB degradation IκB-α-independently regulates NF-κB activity.37 Whether SHIP1 enhances LPS-induced NF-κB activation by affecting NF-κB phosphorylation or proteasome activity remains unclear. Our future study will illuminate whether SHIP1 enhances LPS-induced NF-κB phosphorylation or inhibits proteasome-mediated NF-κB degradation.
In conclusion, we provided the first evidence that SHIP1 can inhibit LPS-induced inflammatory response through a phosphatase activity- and PI-3K-independent mechanism. In addition to inhibiting LPS-induced PI-3K activation, SHIP1 inhibits the LPS-induced TLR4-MyD88 combination and Ras activation and subsequently inhibits LPS-induced activation of MAPKs, which is primarily in a phosphatase activity- and PI-3K-independent manner. These results suggest that RNA interfering and ectopic expression targeting SHIP1 might provide novel therapeutic strategies to modulate LPS response.
Prepublished online as Blood First Edition Paper, February 8, 2005; DOI 10.1182/blood-2005-01-0191.
Supported by grants from the National Natural Science Foundation of China (30300187, 30200145, 30121002, 30490240), Tsinghua Yuyuan Foundation (202400.005-02), and the National Key Basic Research Program of China (2001CB510002).
H.A. and H.X. contributed equally to this work.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank Dr J. Rayner for critically reading this manuscript. Xuetao Cao and Huazhang An designed the research; Huazhang An, Hongmei Xu, Minghui Zhang, Jun Zhou, Tao Feng, Cheng Qian and Runzi Qi performed it; and Xuetao Cao, Huazhang An and Hongmei Xu analyzed data and wrote the paper.