Abstract
Platelets are necessary for lung leukocyte recruitment in a murine model of allergic inflammation, and platelet–leukocyte aggregates are formed in circulating blood of patients with asthma after allergen exposure. However, it is unknown how platelets induce pulmonary leukocyte recruitment in asthma. Here, we have investigated the importance of platelet adhesion molecule expression on pulmonary eosinophil and lymphocyte recruitment and on leukocyte CD11b and very late antigen (VLA)–4 expression in mice. Pulmonary leukocyte recruitment in platelet-depleted mice (sensitized and exposed to ovalbumin) transfused with fixed, unstimulated platelets (FUSPs) was abolished, whereas transfusion with platelets stimulated and fixed (FSPs), expressing P-selectin and P-selectin glycoprotein ligand-1 (PSGL-1), restored eosinophil and lymphocyte recruitment. Transfusion with platelets from P-selectin–deficient mice, or with FSPs stimulated in the presence of a blocking anti–P-selectin antibody, were unable to restore pulmonary leukocyte recruitment. Flow cytometric analysis revealed increased expression of CD11b and VLA-4 on leukocytes attached to platelets after allergen exposure, and CD11b expression on leukocytes was suppressed in thrombocytopenic mice but was restored with the transfusion of FSPs, but not FUSPs, a phenomenon concurrent with the formation of platelet–leukocyte complexes. P-selectin expression on the surfaces of platelets is a major requirement for pulmonary eosinophil and lymphocyte recruitment, allowing circulating platelets to bind to and stimulate leukocytes for endothelial attachment.
Introduction
Bronchial asthma has been recognized as a chronic inflammatory disease associated with leukocyte infiltration and airway epithelial damage. It is now clear that eosinophil, neutrophil, mast cell, and T-lymphocyte activation occurs in allergic asthma,1 whereas platelets appear to be important in murine models of chronic allergic inflammation.2 The presence of intravascular platelet aggregates within bronchial biopsy specimens in patients with asthma has also been reported.3 Substantial clinical evidence demonstrates intravascular platelet activation accompanying allergen-induced bronchoconstriction in patients with asthma, suggestive of participation of these blood elements in the pathophysiology of asthma,4-8 and the expression of P-selectin on platelets was found to be increased in patients with asthma.9 This is also apparent in other diseases with a substantial inflammatory component, including atherosclerosis,10 and in tumor metastasis, a disease process with many similarities to leukocyte recruitment,11,12 the implication being that platelet activation is a general feature of diseases in which leukocyte recruitment from the circulation to particular anatomic sites is required.
Using immune and nonimmune methods of platelet depletion to render mice severely thrombocytopenic, we recently demonstrated in a murine model of allergic inflammation that platelets are essential for eosinophil and lymphocyte recruitment to the lungs.8 This phenomenon was dependent on the presence of intact platelets rather than on the release of any soluble, platelet-released, proinflammatory mediators.8 Although our studies were conducted investigating eosinophil and lymphocyte recruitment, it can be envisaged that leukocyte recruitment from the circulation in general can be facilitated by a platelet-dependent mechanism and not restricted to the cells thus far studied given that the recruitment of other cell types is also dependent on platelets, as reported during atherosclerotic lesion formation.10
Interestingly, in our own studies, there was a significant increase in circulating platelet–leukocyte complexes upon allergen exposure in mice sensitized to allergen-allergen exposure. Leukocytes attached to platelets displayed a significant increase in the expression of the adhesion molecule CD11b, implying that platelets contribute to leukocyte activation and prime leukocytes for tissue recruitment. This finding was mirrored in patients with asthma undergoing allergen challenge.8
It is likely, therefore, that the requirement for platelets in inducing leukocyte recruitment to extravascular tissues during allergic lung inflammation occurs at the level of contact-dependent signaling to leukocytes, initiating the expression of adhesion molecules required for the attachment to activated endothelium. Indeed, P-selectin expression on platelets, but not on endothelial cells, has been shown to be responsible for leukocyte rolling along endothelium.13,14 Platelets roll on stimulated endothelium in vivo in a manner similar to that of leukocytes,15 suggesting that platelets may act as a bridge upon which leukocytes adhere to the endothelium from the circulation. Similarly, platelets have been shown to facilitate eosinophil–endothelial adherence when taken from allergic patients with asthma but not from healthy subjects.15 Although it is unknown at which point of the adhesion process platelets become involved in the murine model of allergic inflammation described,8 in other models the occurrence of platelet–leukocyte complexes is abolished by the administration of antibodies to P-selectin or to its counter ligand, P-selectin glycoprotein ligand-1 (PSGL-1).16-18 Mice made selectively deficient in L- or P-selectin exhibited virtually no leukocyte rolling,19-21 suggesting that platelets may “prime” leukocytes for efficient endothelial trafficking at the level of the circulation.
In the present study, we have investigated the importance of surface-expressed mediators on activated platelets for eosinophil and lymphocyte recruitment and platelet–leukocyte complex formation in a murine model of allergic inflammation, specifically the requirement for surface-expressed P-selectin on platelets. We have also recorded the increased occurrence of platelet–leukocyte complexes in the circulating blood of allergen-challenged mice and have linked this to an increased expression of very late antigen (VLA)–4 and CD11b on the surface of leukocytes.
Materials and methods
Sensitization of mice to ovalbumin
Male C57BL/6 mice (each weighing 20-25 g; Charles River) were immunized with chicken egg ovalbumin (OVA; 10 μg/0.4 mL intraperitoneally) on days 0 and 7, as previously described.8 Mice were subsequently exposed to aerosolized OVA (10 mg/mL) for 3 repeated 15-minute periods on days 15, 16, and 17 (model 104; Faset Aerosol Prisma; particle size 2-5 μm). Twenty-four hours after the last allergen challenge, mice were studied as outlined in this article. In some studies, blood was taken 24 hours after the start of challenge on day 15, the first day of challenge, for flow cytometric analysis. Local ethics committee approval was obtained from the University of Perugia.
Busulfan-induced platelet depletion
Busulfan (Sigma-Aldrich, Poole, United Kingdom), a bone marrow precursor cell–specific depressing agent, was used to deplete platelets, as previously described.8 Busulfan was prepared in polyethylene glycol 400 (25 mg/mL) and was heated at 65°C to 70°C until the mixture went into solution, before dilution (1:8) in warm saline for injection on days -4, -2, and 1 of the immunization protocol (20 mg/kg, 0.2 mL administered intraperitoneally).
Ex vivo manipulation of platelets and restoration of platelet population in thrombocytopenic mice
Citrated blood was taken from OVA-immunized mice and centrifuged for 20 seconds using an Eppifuge. The resultant platelet-rich plasma (PRP) was gel filtered with Sepharose 2B in Tyrode buffer. Gel-filtered platelets were diluted to 1 × 105 platelets per microliter and were stimulated for 4 minutes with 1 U/mL bovine thrombin (Sigma-Aldrich) in the presence of RGD peptide (1 mM) and CaCl2 (4 mM). The reaction was stopped with hirudin (10 U/mL). Platelet suspension was then fixed for 10 minutes with an equal volume of 2% paraformaldehyde (PFA) and was centrifuged at 1000 g. The pellet was resuspended in phosphate-buffered saline (PBS) supplemented with PGI2 (0.02 μM). These fixed stimulated platelets (FSPs) were then intravenously injected into mice made thrombocytopenic by busulfan treatment. In other experiments, washed platelets were fixed without previous stimulation with thrombin (fixed unstimulated platelets [FUSPs]). Thrombocytopenic mice received 2 transfusions of platelets, 20 minutes before allergen challenge, on the first 2 days of exposure. In some experiments, platelets were stimulated with thrombin in the presence of 100 μg monoclonal anti–P-selectin blocking antibody (RB40.34; Becton Dickinson, San Diego, CA) before reinjection. Typically, the injection volume of 0.2 mL contained 1.0 to 1.5 × 108 platelets, giving a cumulative dose of 2.0 to 3.0 × 108 platelets over the 2 injections. Preliminary studies were conducted with the administration of varying doses of antiplatelet antisera (APAS) into OVA-immunized mice,8 which produced different degrees of thrombocytopenia. This allowed us to determine the threshold concentration of circulating platelets that was expected to affect pulmonary leukocyte recruitment after reinfusion. After stimulation, the expression of P-selectin and PSGL-1 on the surfaces of platelets was quantified using flow cytometry, as explained below.
In studies using P-selectin–deficient mice, washed platelets from wild-type (C57Bl/6J) and P-selectin–deficient mice (C57Bl/6J/129Sw background; Jackson Laboratory, Bar Harbor, ME) were prepared as described. Platelets were injected intravenously into thrombocytopenic mice 20 minutes before allergen challenge on the first 2 days of exposure. Typically, the injection volume of 0.2 mL contained 2.5 to 3.0 × 108 platelets, giving a cumulative dose of 5.6 to 6.0 × 108 platelets over the 2 injections.
Bronchoalveolar lavage
Twenty-four hours after the last aerosol challenge on day 17, mice were anesthetized with sodium pentobarbital (0.1 mL 5% solution intraperitoneally), the trachea was exposed and cannulated, and 3 aliquots (0.5 mL each) of warm, sterile saline solution were injected into the lung; the resultant fluid was drawn out with a 1-mL syringe and put on ice. Total and differential cell counts were performed in a Burker chamber with a 25 × objective.
Platelet and leukocyte counts in blood and bone marrow
Blood (5 μL) was collected before challenge by tail bleed, using a pipette. The blood was added to 95 μL Stromatol solution (Mascia Brunelli srl, Milan, Italy) for platelet counting using a Burker chamber (Neuroprobe Inc, Gaithersburg, MD) under a 40 × objective. Total and differential blood cell counts were performed as previously described.8 Bone marrow was retrieved from both femurs taken from the hindlimbs of mice, and cytospins were prepared from leukocytes resuspended in 1 mL saline. Total and differential cell counts were then enumerated.
Lung histology
Some mice were killed 30 hours after the last allergen exposure; lungs were removed, processed with OCT compound (TissueTek, Redding, CA), and frozen at -80°C for immunofluorescence staining. Eosinophils were identified by morphologic characteristics and with a primary rat antimouse major basic protein (MBP) antibody (MT2-14.7.2; a kind gift from Dr J. Lee, Mayo Clinic, Scottsville, AZ) and an antirat immunoglobulin G–fluorescein isothiocyanate (IgG-FITC)–labeled secondary antibody. Platelets were identified with a primary goat anti-CD41 antibody (sc-6604; Santa Cruz Biotechnology, Santa Cruz, CA)2 and an antigoat IgG-cyanin 3 (Cy3)–labeled secondary antibody. Slides were observed under a 100 × objective using a fluorescence microscope.
Flow cytometry
Blood was obtained by means of cardiac puncture from anesthetized mice on citrate 24 hours after the first day of aerosol challenge and was analyzed for the presence of platelet–leukocyte aggregates and for CD11b and VLA-4 on leukocytes. Monoclonal antibodies, used in saturating concentrations, were FITC-labeled anti-CD41 (gpIα-IIβ no. 553848), phycoerythrin (PE)–labeled anti-CD11b (Mac-1 no. 557397), and streptavidin-labeled anti-CD49d (VLA-4 no. 557406, with second-step conjugation to streptavidin–PE conjugate no. 554061) (all from PharMingen, San Diego, CA) or control antibodies. After a 10-minute incubation at room temperature in the dark, 450 μL water was added to lyse red blood cells for a further 10 minutes before 500 μL paraformaldehyde (1% in PBS) was added. Samples were read within 4 to 6 hours on a FACScan flow cytometer (Coulter Epics XL-MCL Instrumentation, Milan, Italy). Live gating was performed on leukocyte-sized events to exclude single platelets; leukocytes were identified by their forward and side scatter characteristics. Events in this region, which were positive for CD41, were considered to represent platelet–leukocyte aggregates. CD11b- and VLA-4–positive events on platelet–leukocyte complexes were then identified from this region. CD11b- and VLA-4–positive events on leukocytes in general were identified by positive gating for PE fluorescence, and leukocytes not attached to platelets were identified as excluded from a gate ascertaining FITC-positive events.
In some experiments, the percentage of platelets positive for P-selectin and PSGL-1 expression was obtained from washed platelet samples that were then reinfused into platelet-depleted animals. Platelets were positively identified by the CD41-FITC or the CD61-PE (integrin β3 chain no. 553347) antigen, and the surface expression of P-selectin and PSGL-1 was identified using antibodies against CD62P-FITC (P-selectin no. 553744) or CD154-PE (PSGL-1 no. 555306).
Statistical analysis of data
Data are expressed as mean ± SEM. Bronchoalveolar (BAL) fluid leukocyte numbers, blood leukocyte and platelet numbers, and FACScan data were analyzed using one-way analysis of variance (ANOVA), followed by Bonferroni multiple-comparisons test. Nonlinear regression (1-site competition) was performed for data studying the effects of APAS on eosinophil recruitment for calculation of the coefficient of correlation (r2). All analyses were conducted using the GraphPad Prism statistical package (version 4.0; Graph Pad, San Diego, CA). P less than .05 was considered significant.
Results
Effects of activated platelet surface mediator expression on pulmonary eosinophil and lymphocyte recruitment
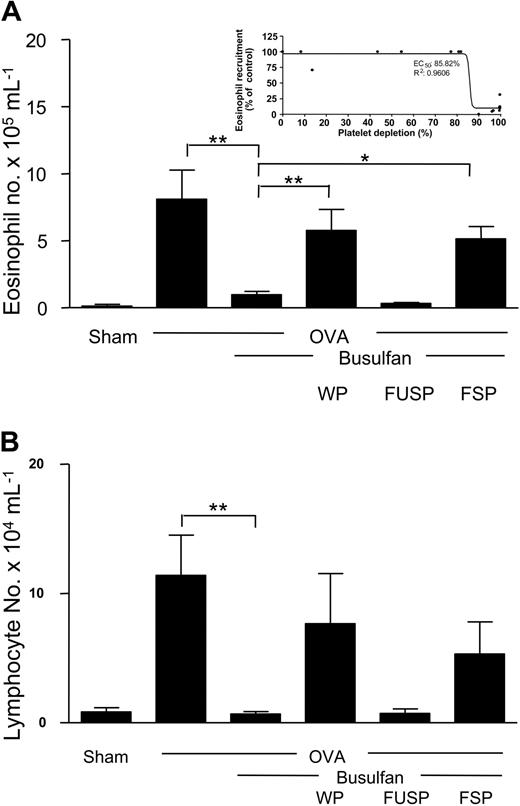
Allergen sensitization and subsequent allergen exposure by aerosol resulted in a significant recruitment of eosinophils to the lungs 24 hours after the last allergen challenge compared with sham-sensitized animals (8.1 ± 2.2 × 105 cells/mL vs 0.1 ± 0.1 × 105 cells/mL; P < .001). Mice rendered severely thrombocytopenic with busulfan (0.1 ± 0.1 × 109 cells/mL vs 1.1 ± 0.1 × 109 cells/mL; 91% depletion; P < .001) before the start of allergen exposure showed significantly reduced recruitment of eosinophils to the lungs 24 hours after the last allergen challenge (1.0 ± 0.3 × 105 cells/mL; P < .01) (Figure 1A). This phenomenon was also observed at an earlier time, 8 hours after allergen challenge (OVA control, 1.7 ± 0.4 × 105 cells/mL; OVA + busulfan, 0.3 ± 0.1 × 105 cells/mL; P < .01). Busulfan treatment only marginally affected total circulating leukocytes (1.1 ± 0.1 × 107 cells/mL vs 0.83 ± 0.01 × 107 cells/mL, 24% depletion; P < .05), but it did not significantly reduce circulating blood eosinophil levels (OVA controls, 3.8 ± 0.8 × 105 cells/mL; OVA + busulfan, 3.9 ± 0.9 × 105 cells/mL) or eosinophil levels in the bone marrow (OVA controls, 2.3 ± 0.6 × 106 cells/mouse; OVA + busulfan, 2.2 ± 0.2 × 106 cells/mouse). Furthermore, the infusion of gel-filtered platelets (containing no leukocytes) from donor animals into thrombocytopenic mice significantly restored pulmonary eosinophil recruitment into the lung, as measured in BAL fluid, compared with busulfan-treated controls (5.8 ± 1.6 × 105 cells/mL vs 1.0 ± 0.03 × 105 cells/mL; P < .01) to a level not significantly different than that of OVA controls (Figure 1A).
Infusion of stimulated platelets restores pulmonary eosinophil and lymphocyte recruitment in sensitized mice depleted of platelets. Sham- and OVA-sensitized mice were exposed to allergen, and BAL fluid was obtained 24 hours after the third day of challenge and analyzed for eosinophil (A) and lymphocyte (B) numbers. In some groups, mice were rendered thrombocytopenic with the administration of busulfan. Selected groups of thrombocytopenic mice were intravenously administered WPs, FUSPs, or FSPs. (A, inset) Dose-response curve of platelet depletion compared with eosinophil recruitment. n = 4-6 animals per group. Data are expressed as mean ± SEM. *P < .05; **P < .01.
Infusion of stimulated platelets restores pulmonary eosinophil and lymphocyte recruitment in sensitized mice depleted of platelets. Sham- and OVA-sensitized mice were exposed to allergen, and BAL fluid was obtained 24 hours after the third day of challenge and analyzed for eosinophil (A) and lymphocyte (B) numbers. In some groups, mice were rendered thrombocytopenic with the administration of busulfan. Selected groups of thrombocytopenic mice were intravenously administered WPs, FUSPs, or FSPs. (A, inset) Dose-response curve of platelet depletion compared with eosinophil recruitment. n = 4-6 animals per group. Data are expressed as mean ± SEM. *P < .05; **P < .01.
Inhibition of eosinophil recruitment in mice administered APAS occurred when platelet depletion exceeded 83% compared with the normal value (dose-response curve; 50% effect (EC50) = 85.8%; r2 = 0.9606; n = 19) (Figure 1A, inset). For this reason, mice depleted of platelets by more than 90% were used in this study, and subsequent procedures investigating the effect of platelet reconstitution on lung leukocyte recruitment were conducted with a dose of platelets that increased circulating numbers to at least 25% to 40% of original values.
In contrast, eosinophil recruitment was not restored in thrombocytopenic mice transfused with gel-filtered resting platelets that were fixed with 1% PFA before transfusion (FUSPs) (0.3 ± 0.1 × 105 cells/mL vs 1.0 ± 0.03 × 105 cells/mL in thrombocytopenic control mice) (Figure 1A). However, the infusion of gel-filtered platelets that had been stimulated with thrombin and then fixed with 1% PFA (FSPs) significantly restored eosinophilia (5.2 ± 0.9 × 105 cells/mL; P < .05) to levels comparable to those observed in the BAL fluid of OVA-sensitized mice with normal platelet counts (8.1 ± 2.2 × 105 cells/mL) (Figure 1A). Interestingly, there was a significant difference in the percentage of platelets expressing the adhesion molecules P-selectin and PSGL-1 on the surface of FSPs compared with FUSPs, as measured by flow cytometry (P-selectin: FSP, 55.6% ± 11.5%; FUSP, 25.9% ± 7.6%; P < 0.05) (PSGL-1: FSP, 24.8% ± 4.7%; FUSP, 7.8% ± 1.8%; P < .01). Levels of P-selectin and PSGL-1 on FUSPs were found to be equivalent to levels found on washed platelets (WPs) (P-selectin: 20.3% ± 4.8%; PSGL-1: 6.7% ± 3.0%).
Similarly, platelet depletion significantly reduced pulmonary lymphocyte recruitment compared with OVA-sensitized controls (P < .05) (Figure 1B), and the transfusion of WPs and FSPs restored lymphocyte recruitment in platelet-depleted mice whereas the transfusion of FUSPs did not (Figure 1B). Busulfan administration did not significantly reduce lymphocyte levels in femur bone marrow compared with OVA-sensitized control mice (4.1 ± 0.6 × 106 cells/mouse vs 3.3 ± 0.7 × 106 cells/mouse).
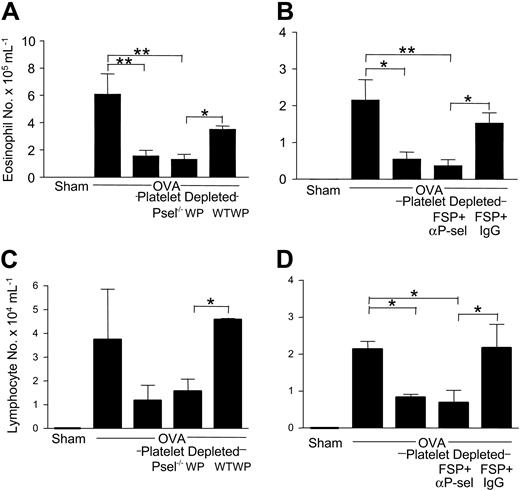
Further studies were conducted to specifically investigate the role of platelet P-selectin on pulmonary eosinophil recruitment with the use of washed platelets taken from P-selectin–deficient mice, cross-transfused into OVA-sensitized thrombocytopenic mice. Eosinophil recruitment remained suppressed in thrombocytopenic mice receiving washed platelets deficient in P-selectin (1.3 ± 0.4 × 105 cells/mL) compared with thrombocytopenic control mice (1.6 ± 0.4 × 105 cells/mL) (Figure 2A). On the contrary, the transfusion of washed platelets taken from normal C57BL/6 mice restored eosinophil recruitment. This was significantly different than in mice receiving P-selectin–deficient platelets (3.5 ± 0.3 × 105 cells/mL vs 1.3 ± 0.4 × 105 cells/mL; P < .05) but was not significantly different than in OVA-immunized controls (6.1 ± 1.5 × 105 cells/mL) (Figure 2A). Additionally, in this set of experiments, busulfan administration to OVA-sensitized mice significantly suppressed circulating blood platelet numbers compared with OVA-sensitized control mice (0.06 ± 0.01 × 109 cells/mL vs 0.84 ± 0.01 × 109 cells/mL; 93% depletion; P < .001), but it did not significantly affect leukocyte numbers (0.78 ± 0.1 × 107 cells/mL vs 0.85 ± 0.1 × 107 cells/mL; 8% depletion; P = NS).
Platelet P-selectin is required for pulmonary eosinophil and lymphocyte recruitment in allergen-sensitized mice previously depleted of platelets. Sham- and OVA-sensitized mice were exposed to allergen, and BAL fluid was obtained 24 hours after the third day of challenge and analyzed for eosinophil and lymphocyte numbers. In some groups, mice were rendered thrombocytopenic with the administration of busulfan. Selected groups of thrombocytopenic mice were administered (A,C) washed platelets from P-selectin–deficient (P-sel-/-WP) or normal mice (WTWP) or (B,D) stimulated platelets coincubated with a P-selectin blocking antibody (FSP + αP-sel) or control IgG (FSP + IgG). n = 3-4 animals per group. Data are expressed as mean ± SEM. *P < .05; **P < .01.
Platelet P-selectin is required for pulmonary eosinophil and lymphocyte recruitment in allergen-sensitized mice previously depleted of platelets. Sham- and OVA-sensitized mice were exposed to allergen, and BAL fluid was obtained 24 hours after the third day of challenge and analyzed for eosinophil and lymphocyte numbers. In some groups, mice were rendered thrombocytopenic with the administration of busulfan. Selected groups of thrombocytopenic mice were administered (A,C) washed platelets from P-selectin–deficient (P-sel-/-WP) or normal mice (WTWP) or (B,D) stimulated platelets coincubated with a P-selectin blocking antibody (FSP + αP-sel) or control IgG (FSP + IgG). n = 3-4 animals per group. Data are expressed as mean ± SEM. *P < .05; **P < .01.
In another set of experiments, after coincubating platelets with a blocking antimouse P-selectin antibody or with an aspecific IgG, we investigated the effects of transfusing fixed, thrombin-stimulated platelets into thrombocytopenic mice on eosinophil recruitment. Platelets incubated with a control IgG before thrombin stimulation displayed a significant increase in P-selectin expression compared with nonstimulated platelets, as measured by flow cytometry (17.0% ± 2.2% vs 5.9% ± 0.2%; P < .05) Incubation with the blocking anti–P-selectin antibody suppressed the percentage of platelets positive for P-selectin fluorescence (7.9% ± 2.8%). The infusion of fixed platelets prestimulated in the presence of an anti–P-selectin antibody did not restore recruitment of eosinophils to the lungs compared with control thrombocytopenic mice (0.4% ± 0.2% × 105 cells/mL vs 0.5% ± 0.2% × 105 cells/mL). However, in thrombocytopenic mice transfused with platelets stimulated in the presence of control IgG, pulmonary eosinophil recruitment was significantly restored (1.5 ± 0.3 × 105 cells/mL; P < .05 compared with mice transfused with FSP + anti–P-selectin) and was not significantly different from OVA-immunized control mice (2.2 ± 0.6 × 105 cells/mL) (Figure 2B).
To exclude enhanced platelet clearance as a cause of the lack of effect of ex vivo anti–P-selectin–treated platelets in restoring eosinophil lung recruitment, control experiments were performed. Platelet numbers increased 1 hour after reinfusion (platelet dose, 1.6 × 108 cells per mouse) of FSPs (0 hour, 1.7 ± 0.2 × 108 cells/mL; 1 hour, 2.9 ± 0.1 × 108 cells/mL); of fixed platelets incubated with a control IgG antibody (FSP + IgG) (0 hour, 1.6 ± 0.3 × 108 cells/mL; 1 hour, 2.7 ± 0.3 × 108 cells/mL); of fixed platelets incubated with an antimouse CD41 antibody (FSP + anti-CD41) (0 hour, 1.7 ± 0.1 × 108 cells/mL; 1 hour, 3.4 ± 0.7 × 108 cells/mL); and of fixed platelets incubated with an anti–P-selectin antibody (FSP + anti–P-selectin) (0 hour, 1.8 ± 0.1 × 108 cells/mL; 1 hour, 3.7 ± 1.0 × 108 cells/mL). Similarly, 3 hours after transfusion, platelet numbers remained elevated in all groups and were not statistically different (FSP, 2.9 ± 0.1 × 108 cells/mL; FSP + IgG, 3.3 ± 0.1 × 108 cells/mL; FSP + anti-CD41, 3.0 ± 0.1 × 108 cells/mL; FSP + anti–P-selectin, 3.2 ± 1.1 × 108 cells/mL), whereas 20 hours after reinfusion, platelet numbers had returned to baseline values in all treatment groups (FSP: 1.9 ± 0.3 × 108 cells/mL; FSP + IgG: 1.2 ± 0.3 × 108 cells/mL; FSP + anti-CD41: 1.4 ± 0.6 × 108 cells/mL; FSP + anti–P-selectin: 1.9 ± 0.4 × 108 cells/mL).
Similar observations on the effects of platelet P-selectin on eosinophil recruitment were documented in relation to pulmonary lymphocyte recruitment (Figure 2C-D). In particular, the requirement for platelets in inducing pulmonary lymphocyte recruitment was dependent on platelet P-selectin because the transfusion of platelets from P-selectin–deficient mice (Figure 2C) and platelets stimulated in the presence of an anti–P-selectin antibody (Figure 2D) did not restore lymphocyte recruitment, whereas wild-type platelets and fixed platelets stimulated in the presence of control IgG did restore lymphocyte recruitment (Figure 2C-D).
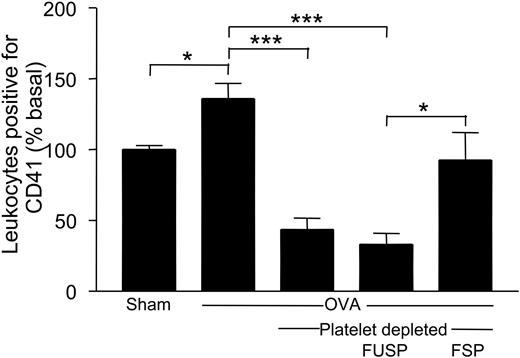
Effects of allergen exposure and platelet stimulation on the formation of platelet–leukocyte complexes in circulating blood
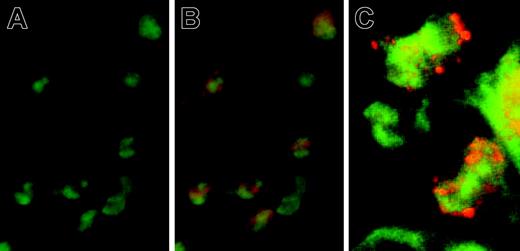
Histologic analysis of lung tissue, after the first day of allergen exposure, revealed the presence of platelets (red, positive for CD41) attached to eosinophils (green, positive for MBP) and multilobed nuclei migrating to lung tissue (Figure 3A-C). Studies were thus performed to examine the presence of platelet–leukocyte complexes in circulating blood 24 hours after the initial day of allergen exposure. This time was chosen because preliminary studies have shown it to be optimal for blood eosinophilia after allergen exposure. Flow cytometric analysis of whole blood revealed a significant increase in the percentage of leukocytes positive for the platelet-specific marker CD41 in blood taken from OVA-sensitized mice compared with sham-sensitized controls (measured in relation to basal: 136.1% ± 2.9% vs 100.0% ± 2.9%; P < .05). Although platelet depletion obviously led to a significant decrease in the percentage of leukocytes attached to platelets after allergen exposure compared with that in OVA-sensitized controls (43.6% ± 8.1%; P < .001), thrombocytopenic mice transfused with FSPs displayed a significant increase in the percentage of leukocytes complexed to platelets than did mice receiving FUSPs (measured in relation to basal, 92.6% ± 19.5% vs 33.1% ± 7.8%; P < .05) (Figure 4), demonstrating the ability of FSPs to attach to circulating leukocytes after reinfusion in thrombocytopenic mice, in correlation to the increased expression of the adhesion molecules P-selectin (P < .05) and PSGL-1 (P < .05) on the surface of FSPs (P-selectin, 54.4% ± 8.2%; PSGL-1, 35.8% ± 8.1%) compared with the surface of FUSPs (P-selectin, 18.8% ± 7.4%; PSGL-1, 10.5% ± 0.6%). In this set of experiments, busulfan administration to OVA-sensitized mice significantly suppressed circulating blood platelet numbers compared with those in control mice (0.07 ± 0.01 × 109 cells/mL vs 1.05 ± 0.06 × 109 cells/mL; 93% depletion; P < .001).
Identification of platelet–eosinophil complexes in lungs taken from allergen-sensitized mice after allergen exposure. Lungs were taken and processed for immunofluorescence examination 30 hours after the start of allergen exposure. Sections were stained for an eosinophil-specific protein (rat anti-MBP; green fluorescence) and for a platelet-specific protein (goat anti-CD41; red fluorescence). (A) Image with filter for only green fluorescence (MBP+) (objective lens ×40). (B) Image with filters for both green and red (CD41+) fluorescence; tissue eosinophils were observed complexed to platelets (objective lens ×40). (C) Individual platelets can be seen attached to eosinophils. Sections were analyzed using a 100 × objective lens. Sections were analyzed, with immersion oil, using a light fluorescence microscope (AxioSkop 2 Plus; Carl Zeiss, Oberkochen, Germany). Images were analyzed with Lucia Core System 1.0 (Prague, Czech Republic). The Zeiss Achroplan ×100 objective has a numerical aperture (NA) of 1.25 (Figure 3C). Figures 3A and 3B were viewed with a Zeiss Achroplan ×40 objective, and this has an NA of 0.75.
Identification of platelet–eosinophil complexes in lungs taken from allergen-sensitized mice after allergen exposure. Lungs were taken and processed for immunofluorescence examination 30 hours after the start of allergen exposure. Sections were stained for an eosinophil-specific protein (rat anti-MBP; green fluorescence) and for a platelet-specific protein (goat anti-CD41; red fluorescence). (A) Image with filter for only green fluorescence (MBP+) (objective lens ×40). (B) Image with filters for both green and red (CD41+) fluorescence; tissue eosinophils were observed complexed to platelets (objective lens ×40). (C) Individual platelets can be seen attached to eosinophils. Sections were analyzed using a 100 × objective lens. Sections were analyzed, with immersion oil, using a light fluorescence microscope (AxioSkop 2 Plus; Carl Zeiss, Oberkochen, Germany). Images were analyzed with Lucia Core System 1.0 (Prague, Czech Republic). The Zeiss Achroplan ×100 objective has a numerical aperture (NA) of 1.25 (Figure 3C). Figures 3A and 3B were viewed with a Zeiss Achroplan ×40 objective, and this has an NA of 0.75.
Circulating platelet–leukocyte complexes are increased in allergen-sensitized mice after allergen exposure. Sham- and OVA-sensitized mice were exposed to allergen, and circulating blood was obtained by cardiac puncture 24 hours after 1 day of allergen exposure. In some groups, mice were rendered thrombocytopenic by the administration of busulfan. Selected groups of thrombocytopenic mice were intravenously administered WPs, FUSPs, or FSPs. Leukocytes (detected by their forward and side scatter characteristics) attached to platelets were identified by anti–CD41-FITC fluorescence. n = 5-9 animals per group. Data are expressed as mean ± SEM. *P < .05; ***P < .001.
Circulating platelet–leukocyte complexes are increased in allergen-sensitized mice after allergen exposure. Sham- and OVA-sensitized mice were exposed to allergen, and circulating blood was obtained by cardiac puncture 24 hours after 1 day of allergen exposure. In some groups, mice were rendered thrombocytopenic by the administration of busulfan. Selected groups of thrombocytopenic mice were intravenously administered WPs, FUSPs, or FSPs. Leukocytes (detected by their forward and side scatter characteristics) attached to platelets were identified by anti–CD41-FITC fluorescence. n = 5-9 animals per group. Data are expressed as mean ± SEM. *P < .05; ***P < .001.
Effects of platelets on the expression of adhesion molecules on the surface of circulating leukocytes
VLA-4 expression on circulating leukocytes was not different between sham and OVA-sensitized mice after allergen exposure (Figure 5A), though in mice depleted of platelets there was a tendency to an increase of VLA-4 on circulating leukocytes (Figure 5A) that was not significant. However, an analysis of leukocytes attached to platelets revealed a significant increase in the percentage of leukocytes expressing VLA-4 in OVA-sensitized mice compared with sham-sensitized controls when measured as a percentage of basal expression (+165.3% ± 35.4% vs +100.3% ± 13.7%; P < .05). There was a tendency to an increase of leukocytes expressing VLA-4 in platelet–leukocyte complexes in thrombocytopenic mice after reinfusion of FSPs (265.7% ± 109.7%) compared with that in mice reinfused with FUSPs (84.7% ± 22.1%) (Figure 5B). Further analysis revealed no difference in the percentages of non–platelet-bound leukocytes expressing VLA-4 between sham- and OVA-sensitized mice or in OVA-sensitized thrombocytopenic mice (Figure 5C). Thus, the tendency for an increase in the percentage of circulating leukocytes displaying VLA-4 in thrombocytopenic mice (Figure 5A) was not a result of platelet depletion.
VLA-4 expression on circulating leukocytes complexed to platelets after allergen exposure is increased. Sham- and OVA-sensitized mice were exposed to allergen, and circulating blood was obtained by cardiac puncture 24 hours after 1 day of allergen exposure. In some groups, mice were rendered thrombocytopenic with the administration of busulfan. Leukocytes were identified by forward and side scatter characteristics. Selected groups of thrombocytopenic mice were intravenously administered FUSPs or FSPs. Platelet–leukocyte complexes were identified with positive fluorescence gating for anti–CD41-FITC, and VLA-4 expression was then identified using anti–CD49d-streptavidin-PE conjugate. (A) VLA-4 expression on circulating leukocytes. (B) VLA-4 expression on platelet–leukocyte complexes. (C) VLA-4 expression on non–platelet-bound leukocytes. n = 5-9 animals per group. Data are expressed as mean ± SEM. *P < .05.
VLA-4 expression on circulating leukocytes complexed to platelets after allergen exposure is increased. Sham- and OVA-sensitized mice were exposed to allergen, and circulating blood was obtained by cardiac puncture 24 hours after 1 day of allergen exposure. In some groups, mice were rendered thrombocytopenic with the administration of busulfan. Leukocytes were identified by forward and side scatter characteristics. Selected groups of thrombocytopenic mice were intravenously administered FUSPs or FSPs. Platelet–leukocyte complexes were identified with positive fluorescence gating for anti–CD41-FITC, and VLA-4 expression was then identified using anti–CD49d-streptavidin-PE conjugate. (A) VLA-4 expression on circulating leukocytes. (B) VLA-4 expression on platelet–leukocyte complexes. (C) VLA-4 expression on non–platelet-bound leukocytes. n = 5-9 animals per group. Data are expressed as mean ± SEM. *P < .05.
In contrast to VLA-4 expression on leukocytes, there was a significant increase in the percentage of leukocytes expressing CD11b after allergen exposure between OVA- and sham-sensitized mice (139.0% ± 12.3% vs 100.0% ± 6.8%; P < .05). In mice depleted of platelets, the percentage of leukocytes expressing CD11b was significantly suppressed compared with the percentage in OVA-sensitized control mice (59.5% ± 13.0%; P < .001) (Figure 6A). The reinfusion of FUSPs had no effect on the percentage of leukocytes expressing CD11b (39.5% ± 11.6%; P < .001), though there was a significant increase in the percentage of leukocytes expressing CD11b in mice administered FSPs (93.2% ± 33.4%; P < .05) (Figure 6A).
CD11b expression on circulating leukocytes is suppressed in mice depleted of platelets but is restored with the infusion of FSPs forming complexes with leukocytes. Sham- and OVA-sensitized mice were exposed to allergen, and circulating blood was obtained by cardiac puncture 24 hours after 1 day of allergen exposure. In some groups, mice were rendered thrombocytopenic with the administration of busulfan. Selected groups of thrombocytopenic mice were intravenously administered FUSPs or FSPs. Leukocytes were identified by forward- and side-scatter characteristics. Platelet–leukocyte complexes were identified with positive fluorescence gating for anti–CD41-FITC, and CD11b expression was then identified using anti–CD11b-PE fluorescence. (A) CD11b expression on circulating leukocytes. (B) CD11b expression on platelet–leukocyte complexes. (C) CD11b expression on non–platelet-bound leukocytes. n = 5-9 animals per group. Data are expressed as mean ± SEM. *P < .05; ***P < .001.
CD11b expression on circulating leukocytes is suppressed in mice depleted of platelets but is restored with the infusion of FSPs forming complexes with leukocytes. Sham- and OVA-sensitized mice were exposed to allergen, and circulating blood was obtained by cardiac puncture 24 hours after 1 day of allergen exposure. In some groups, mice were rendered thrombocytopenic with the administration of busulfan. Selected groups of thrombocytopenic mice were intravenously administered FUSPs or FSPs. Leukocytes were identified by forward- and side-scatter characteristics. Platelet–leukocyte complexes were identified with positive fluorescence gating for anti–CD41-FITC, and CD11b expression was then identified using anti–CD11b-PE fluorescence. (A) CD11b expression on circulating leukocytes. (B) CD11b expression on platelet–leukocyte complexes. (C) CD11b expression on non–platelet-bound leukocytes. n = 5-9 animals per group. Data are expressed as mean ± SEM. *P < .05; ***P < .001.
An analysis of leukocytes attached to platelets also revealed a significant increase in the percentage of leukocytes expressing CD11b in OVA-sensitized mice compared with sham-sensitized controls (145.2% ± 19.0% vs 102.8% ± 10.6%; P < .05) (Figure 6B). Furthermore, the reinfusion of FSPs into thrombocytopenic mice increased the percentage of leukocytes complexed to platelets expressing CD11b (64.1% ± 22.9%) compared with mice receiving FUSPs (15.6% ± 4.9%; P < .05). On the contrary, there was no difference in the percentage of non–platelet-bound leukocytes expressing CD11b between sham- and OVA-sensitized mice, and this percentage remained unaffected in thrombocytopenic mice (Figure 6C).
Discussion
We have recently demonstrated, in a murine model of allergic inflammation using immune (antiplatelet antisera) and nonimmune (busulfan) platelet depletion, that platelets are essential for eosinophil and lymphocyte recruitment to the lungs.8 This phenomenon depends on the presence of intact platelets rather than on the release of any soluble, proinflammatory mediators from platelets during periods of allergen exposure.8 In the present study, we provide evidence that pulmonary eosinophil and lymphocyte recruitment in a murine model of allergic inflammation is dependent on leukocyte contact with activated platelets expressing adhesion molecules on their surface and that platelet P-selectin is of major importance in these events. Thus, platelet attachment to leukocytes by platelet P-selectin or its ligand, PSGL-1, increases the expression of adhesion molecules on the surface of leukocytes, priming them for diapedesis through vessel walls.
Primarily, pulmonary eosinophil and lymphocyte recruitment, which was significantly suppressed in mice depleted of platelets, was restored by the transfusion of ex vivo thrombin–stimulated and then fixed platelets (FSPs). This did not occur in mice receiving unstimulated fixed platelets (FUSPs). FSPs were found to display increased levels of the adhesion molecules P-selectin and PSGL-1 on their surface compared with FUSPs; levels in the latter did not differ from those of resting washed platelets. The expression of P-selectin and PSGL-1 on FUSPs, though still higher than levels found normally on platelets circulating in blood, is higher than the expression found on FSPs. The lack of eosinophil-recruiting activity of FUSPs may, therefore, reflect a threshold effect by which a critical amount of adhesive molecules must be expressed on the platelet surface before leukocyte activation is affected. The threshold value of platelet depletion required to suppress eosinophil recruitment in sensitized animals supports this conclusion. A role for platelet P-selectin in eosinophil and lymphocyte recruitment was demonstrated because gel-filtered platelets obtained from P-selectin–deficient mice and transfused into thrombocytopenic mice did not restore pulmonary eosinophil and lymphocyte recruitment. This evidence suggests that platelet-derived P-selectin is important for eosinophil and lymphocyte recruitment, whereas endothelial-derived P-selectin plays a secondary role in leukocyte recruitment because the thrombocytopenic recipient mice were not deficient in P-selectin. The role of platelet-expressed P-selectin was confirmed in experiments performed with FSPs stimulated in the presence of an antimouse P-selectin monoclonal antibody.
The relevance of P-selectin in eosinophil and lymphocyte diapedesis and, therefore, in allergic inflammation has been previously demonstrated in a murine model similar to ours.22 However, the role of platelet P-selectin was not investigated, though it has since been reported that platelet P-selectin, but not endothelial P-selectin, is critical for neutrophil recruitment into the outer and inner medulla of the kidneys in a murine model of acute postischemic renal failure23 and in atherosclerotic lesion development.24 Furthermore, the recent demonstration that circulating leukocyte/monocyte aggregates promote the formation of atherosclerotic lesions suggests that circulating activated platelets are a necessary facet of the inflammatory response, perhaps through the platelet P-selectin–mediated delivery of platelet-derived proinflammatory factors to leukocytes and the vessel wall.25 Interestingly, platelets have been shown to facilitate eosinophil–endothelial adherence when taken from patients with asthma but not from healthy subjects,16 and this depended on activated platelets expressing P-selectin.
Previous studies using in vivo models of inflammatory reactions in the skin26 and the peritoneal cavity27 have demonstrated that P-selectin may play an important role in allergic inflammation earlier (3-12 hours) rather than later (20-24 hours) after allergen challenge. We observed the suppression of leukocyte recruitment to the lungs by platelet depletion at both early (8 hours) and late time points (24 hours) after allergen challenge and, therefore, do not confirm such a time-dependent phenomenon in our model. Indeed, others studying allergic inflammation in the lung also demonstrated the importance of P-selectin at later time points (24 hours) after allergen challenge.22,28
In this study, we have attempted to investigate the mechanism through which stimulated, circulating platelets activate leukocytes and prime them for the subsequent steps of initial vessel wall trafficking through the up-regulation of adhesion molecules. Here, we found that the formation of circulating platelet–leukocyte complexes is significantly increased in allergen-sensitized mice compared with sham-sensitized controls after allergen exposure and that the percentage of leukocytes attached to platelets expressing both CD11b and VLA-4 is increased. This phenomenon was not seen with circulating FUSPs, whereas the formation of circulating platelet–leukocyte complexes expressing CD11b and VLA-4 was restored with the infusion of FSPs. The percentage of leukocytes not attached to platelets and expressing VLA-4 or CD11b did not differ between sham- and allergen-sensitized mice, implying that platelet–leukocyte complexes are further required for efficient leukocyte attachment to the endothelium. In our study, the administration of busulfan was found not to affect the percentage of non–platelet-bound leukocytes expressing VLA-4 or CD11b, confirming that the method of platelet depletion was not toxic to leukocytes.
Rheologic evidence also suggests that leukocyte activation and subsequent integrin expression, after tethering to platelets, is a plausible mechanistic explanation by which platelets are a requisite factor in leukocyte recruitment because platelet–leukocyte collisions occur with greater frequency than leukocyte–endothelium collisions in conditions of laminar flow.29 Physiologic flow includes a redistribution of blood elements by which the density of platelets and leukocytes rapidly increases around the vessel periphery.29-31 This zone “traps” leukocytes into an environment rich in platelets, thus greatly enhancing the possibility of collisions between platelets and leukocytes. This may lead to the tethering of platelets to leukocytes to form rosettes through P-selectin–recognition steps, to up-regulate integrin expression, and to accelerate the action of firm adhesion to endothelium as platelet-bound leukocytes enter the capillary network.
Direct observation of membrane tethering between neutrophils and platelets has been demonstrated under physiologic flow conditions,32 and activated platelets have been shown to bind monocytes, polymorphonuclear (PMN) cells, eosinophils, basophils, and T cells,33,34 in a process involving a P-selectin–dependent recognition step.35 The stimulation of platelets with thrombin has been shown to induce the formation of rosettes around eosinophils in eosinophil–platelet suspensions, an action that was prevented by the inclusion of P-selectin monoclonal antibody.19 The P-selectin released from α granules and exported to the surfaces of platelets is the likely effector of the interaction with eosinophils because soluble P-selectin in plasma is predominantly monomeric and has a lower binding affinity for the P-selectin counter-ligand PSGL-1.36 This cellular interaction may result in the increased expression of integrins on leukocytes,35 and it produces platelet–leukocyte complexes that become the most adhesive cells (respective to their type) in the circulation.37
Recent observations, obtained from studies using whole blood exposed to hydrodynamic shear, comparable to that of the venous circulation, have confirmed that platelet adherence to PMN cells by P-selectin binding resulted in MAC-1–dependent platelet–PMN cell aggregation.38 Two previous reports have also shown the requirement of an intermediate activating signal from platelets themselves for the integrin to become functionally competent in binding to the counterreceptor, either with the platelets immobilized to a surface15 or activated in suspension.35 Thus, platelets are implicated in delivering an activating signal to leukocytes between rolling movement, tethering to endothelium, and firm attachment. Evidence supports a direct role for P-selectin in this scenario because purified P-selectin stimulated MAC-1–dependent platelet adhesion to human PMN cells39 and LFA-1 MAC-1–dependent adhesion of murine PMNs to intercellular adhesion molecule-1 (ICAM-1).40
In addition, P-selectin on activated platelets has been shown to be necessary for the presentation of inflammatory mediators (for example, RANTES) to monocytes, allowing RANTES-dependent monocyte recruitment to atheromatous lesions24,41 in a process that requires the formation of circulating platelet–monocyte aggregates.
In conclusion, the present study has demonstrated the requirement for factors expressed on the surfaces of activated platelets in the pulmonary recruitment of eosinophils and lymphocytes in a murine model of asthma, among which P-selectin plays a crucial role. It is, therefore, conceivable that the mechanism by which platelets induce the efficient attachment of eosinophils and lymphocytes to the endothelium, the first step in their transmigration to the inflamed tissue, is through P-selectin–dependent contact in the circulation, inducing the up-regulation of adhesion molecules on leukocytes.
Prepublished online as Blood First Edition Paper, November 4, 2004; DOI 10.1182/blood-2004-06-2282.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.