Comment on Mauser-Bunschoten et al, page 2654
This article offers an innovative technique—embolization—for stopping joint hemorrhages in hemophilia patients who do not respond to factor replacement.
Joint bleeding has been the major cause of morbidity for hemophilia patients, frequently requiring surgical intervention for correction and requiring large amounts of replacement therapy with significant financial implications. Profuse bleeding frequently occurs either spontaneously or after joint surgery and may respond poorly to factor replacement.
Mauser-Bunschoten and colleagues present a novel approach to this type of bleeding in 18 patients with 23 major point bleeds. Using angiography and embolization, the results were particularly salutary and controlled bleeding in two thirds of cases with 1 procedure. Bleeding recurred in one third of cases, requiring a second treatment, and 1 case needed 3 such procedures.
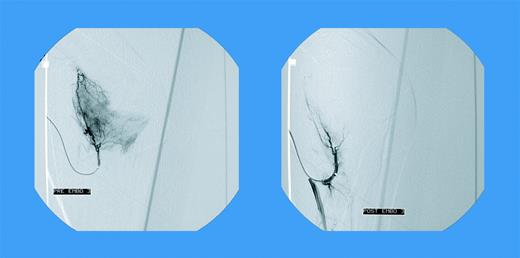
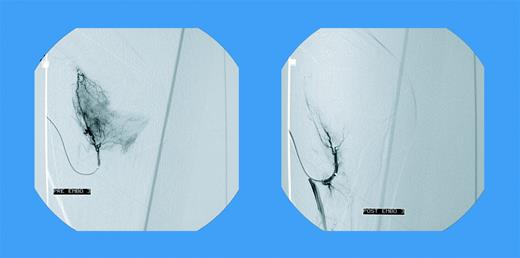
These patients had either factor VIII or factor IX deficiency, with or without inhibitors. Almost twice as many cases were seen after joint replacement (within 6 months) and the remainder were spontaneous. None of these bleeding episodes responded to high-dose factor replacement.FIG1
Blush in a patient with elbow bleeding. See the complete article by Mauser-Bunschoten et al, beginning on page 2654.
Blush in a patient with elbow bleeding. See the complete article by Mauser-Bunschoten et al, beginning on page 2654.
Selective catheterizations of the popliteal and/or the supragenual and infragenual arteries were carried out and angiograms were done with embolization performed with microcoils. Figure 1A-B dramatically demonstrates the effect of these embolizations. This holds true for either spontaneous or post–joint replacement bleeding.
The authors describe the relatively few complications from this procedure. Arterial spasm and a small thrombus were seen. Joint pain was an accompanying symptom after this therapy. As one would anticipate, one of the inhibitor patients had a significant femoral bleed from the puncture site. Although the authors attribute this to early immobilization, femoral punctures are particularly hazardous in this setting.
Although there have been anecdotal reports of using this technique, this large series is of great interest. It is particularly of note that these types of bleeds occurred both spontaneously and in the post–joint replacement surgical setting. Much energy has been spent on trying to prevent the kind of arthropathy leading to such hemorrhage, using varied prophylactic regimens. Despite these efforts, large numbers of young as well as adult patients remain with substantial joint damage vulnerable to such events. This technology, which the authors appropriately caution should be undertaken only by experienced technologists, offers hemostasis where high-cost, large-volume replacement therapy is ineffective.
As factor concentrates opened the door to rehabilitative surgical intervention for hemophilia arthropathy, this technology offers a way to put the proverbial “finger in the dike.” ▪