Abstract
CXC chemokine ligand 12 (CXCL12; stromal cell-derived factor-1 [SDF-1]/pre-B-cell growth-stimulating factor [PBSF]) and its receptor CXCR4 are essential for vascularization in the gastrointestinal tract as well as B lymphopoiesis and colonization of bone marrow by hematopoietic cells. However, the mechanism by which CXCL12/CXCR4 functions in blood vessel formation remains elusive. Here, we have found a novel mode of organ vascularization and determined the roles of CXCL12 in these processes. In the developing small intestine, many short interconnecting vessels form between larger superior mesenteric artery (SMA) and the neighboring primary capillary plexus surrounding the primitive gut, and they elongate and become the arteries supplying the small intestine. Mice lacking CXCL12 or CXCR4 lack the interconnecting vessels but have normal venous networks. The mutants lack filopodial extension and intussusception from endothelial cells of SMAs seen in wild-type embryos. CXCR4 is specifically expressed in arteries in the developing mesenteries and its expression is severely reduced in CXCL12–/– embryos. Mice in which CXCR4 is specifically deleted in the endothelium reveal vascular defects identical to those observed in the conventional CXCR4–/– embryos. Together, CXCL12 acts on arterial endothelial cells of SMA to up-regulate CXCR4 and mediate the connection between the larger artery and neighboring capillary plexus in an organ-specific manner.
Introduction
Vascularization of organs generally occurs during embryogenesis by remodeling of the preexisting vascular system to enable them to perform their specific functions. Early in development, embryos form a primary capillary plexus and major vessels, including the aorta and major veins, by a process referred to as vasculogenesis in which endothelial cells differentiate, proliferate, and aggregate.1-3 The vasculature of organs is thought be generated by 2 processes, sprouting or nonsprouting angiogenesis from the primary plexus or major vessels.1 Sprouting angiogenesis is a process in which capillaries sprout from preexisting vessels into avascular tissues and occurs most frequently late in organogenesis, for example in the brain and kidney.1,3 Nonsprouting angiogenesis is a process of splitting preexisting vessels by transcapillary intussusceptive pillars and has been reported to be predominant in the embryonic lung.4 Recent genetic approaches have provided a valuable starting point in probing the molecular mechanisms of vascular development. Mutant analysis of receptor tyrosine kinases and their ligands (such as Flk-1, Flt-1, VEGF-A, Tie1, Tie2, angiopoietin-1, EphB4, and ephrinB2) has indicated that these molecules are essential for early and general vascular development.1-3,5 However, most of these mutations result in early embryonic lethality, which hampers the analysis of the formation of most organ systems at later embryonic stages. Thus, despite years of investigation, the cellular and molecular mechanisms controlling organ vascularization remain poorly understood.
CXC chemokine ligand 12 (CXCL12; stromal cell–derived factor 1 [SDF-1]/pre-B-cell growth–stimulating factor [PBSF]) is the first cytokine that has been shown to be essential for organ vascularization.6 Chemokines are a large family of structurally related chemoattractive cytokines, which act via hepta helical transmembrane receptors coupled to heterotrimeric guanosine triphosphate (GTP)–binding proteins.7 CXCL12 was first characterized as a pre-B-cell growth–stimulating factor8,9 and its primary physiologic receptor is CXCR4, which also functions as an entry coreceptor for strains of HIV-1.6,10-15 The multiple essential functions of CXCL12 and CXCR4 in development have been demonstrated using mutant mice with targeted gene disruption.6,12,14,15 CXCL12 and CXCR4 are required for B-cell development, colonization of bone marrow by hematopoietic stem cells (HSCs) and myeloid lineage cells, colonization of the gonad by primordial germ cells (PGCs), cardiac ventricular septum formation, and cerebellar development.6,12,14-21 In addition to these, CXCL12–/– or CXCR4–/– embryos display defects in vascularization of the gastrointestinal tract but not in the yolk sac, brain, or heart, demonstrating the essential organ-specific functions of CXCL12 and CXCR4 in blood vessel formation.6 In vitro studies have revealed the activity of CXCL12 in blood vessel formation. CXCL12 induces migration of endothelial cells including human umbilical vein endothelial cells (HUVECs) and human aorta endothelial cells (HAECs).22-24 CXCL12 stimulates formation of capillary-like structures by HUVECs24 and human microvascular endothelial cells.25 CXCL12 induces neovascularization from cross sections of leukocyte-free rat aorta23 and an angiogenic activity in the model of the rabbit corneal pocket.25 Neutralized antibodies against CXCL12 inhibit growth factor–induced invasion by endothelial cells into subcutaneously injected matrigel.26 Despite these studies, the detailed functions of CXCL12 during blood vessel development in vivo remain unclear. Moreover, it is not clear why the essential functions of CXCL12 are organ-specific.
Here, we studied the processes of vascularization of the small intestine and the role of CXCL12 in these processes using CXCL12–/– and CXCR4–/– mice and mice in which CXCR4 was specifically deleted in the endothelium. Our results have demonstrated a novel mode of organ vascularization and revealed that CXCL12 acts on arterial endothelial cells to induce CXCR4 expression and direct the connection between the larger artery and neighboring intrinsic capillary plexus in an organ-specific manner.
Materials and methods
Mice
Immunohistochemical staining
Embryos were dissected, fixed overnight in 4% paraformaldehyde at 4°C, and washed with phosphate-buffered saline (PBS) at 4°C. Then embryos were dehydrated through 50%, 75%, 90%, and 100% methanol (MeOH) and stored at –20°C prior to staining. For whole-mount immunofluorescent staining, embryos were rehydrated through 75%, 50%, and 25% MeOH for 15 minutes each at 4°C and blocked (5% goat serum in PBS plus 0.3% Triton X-100) for 30 minutes at 4°C. Then embryos were stained with anti–platelet-endothelial cell adhesion molecule 1 (PECAM-1) antibody (clone MEC13.3; BD Pharmingen, San Diego, CA; 1:250 dilution) and anti–smooth muscle α-actin antibody (clone 1A4; NeoMarkers, Fremont, CA; 1:400 dilution) followed by Alexa488- or Alexa546-conjugated secondary antibodies (Invitrogen, Carlsbad, CA; 1:500 dilution). Alternatively, to visualize anti–PECAM-1 staining with light microscopy, dehydrated embryos were bleached in 0.3% H2O2/MeOH for 30 minutes at 4°C, rinsed with 100% MeOH, and rehydrated. Embryos were blocked and stained with primary antibody (anti–PECAM-1 antibody) followed by horseradish peroxidase (HRP)–conjugated secondary antibody (Biosource, Camarillo, CA; 1:500 dilution). Then embryos were soaked in PBS plus Triton X (PBST) containing 0.025% diaminobenzidine (Dojindo, Kumamoto, Japan) and 0.08% NiCl2 for 30 minutes, and H2O2 was added to 0.01%. The enzymatic reaction was allowed to proceed until the desired color intensity was reached, and the tissues were rinsed with PBST.
For section staining, embryos were fixed in 4% paraformaldehyde, equilibrated in 30% sucrose/PBS, embedded in optimal cutting temperature (OCT) compound (Tissue-Tek, Sakura Finetechnical, Tokyo, Japan) and sectioned on a cryostat at 10 μm. Then sections were incubated with antibodies against PECAM-1 (1:100 dilution), followed by secondary antibodies conjugated to Alexa488 or Alexa546 (Invitrogen; 1:200 dilution). Samples were mounted with Slowfade Antifade kit (Invitrogen) and viewed using a confocal microscope (LSM 5 PASCAL; Carl Zeiss, Oberkochen, Germany) with Fluar 10 ×/0.50 or Plan Neofluar 40 ×/10.75 (Zeiss). The images were further processed using Adobe Photoshop 5.5.
Whole-mount in situ hybridization
Whole-mount in situ hybridization was performed using digoxigenin (DIG)–labeled riboprobes. Embryos were dissected, fixed, and stored in MeOH prior to staining. Upon rehydration, embryos were treated with 10 μg/mL proteinase K, washed in 2 mg/mL glycine, and refixed with 0.2% glutaraldehyde in 4% paraformaldehyde. Embryos went through a prehybridization incubation (50% formamide, 5 × [0.15 M NaCl, 0.015 M sodium citrate, ph 7.0] [SSC], 1% sodium dodecyl sulfate [SDS], 50 μg/mL yeast tRNA, 50 μg/mL heparin) at 70°C followed by an overnight hybridization at 70°C with DIG-labeled CXCR4 probe at 0.1 μg/mL. Embryos were washed twice in solution 1 (50% formamide, 5 × SSC, 1% SDS) and twice in solution 2 (50% formamide, 2 × SSC), all for 30 minutes at 70°C. Then embryos were washed with TBST (150 mM NaCl, 100 mM Tris-HCl, pH 7.5, 0.1% Tween-20), blocked with 1.5% blocking reagent (Roche Diagnostics, Mannheim, Germany), and incubated overnight at 4°C with alkaline phosphatase–conjugated anti-DIG antibody (Roche Diagnostics). Following several washes in TBST and NTMT (100 mM NaCl, 100 mM Tris-HCl, pH 9.5, 50 mM MgCl2, 0.1% Tween-20), color was developed in 4-nitroblue tetrazolium chloride/5-bromo-4-chloro-3-indonyl phosphate (NBT/BCIP). After in situ hybridization, embryos were embedded and sectioned with a cryostat.
Results
Organ-specific mechanisms of vascularization of the small intestine during ontogeny
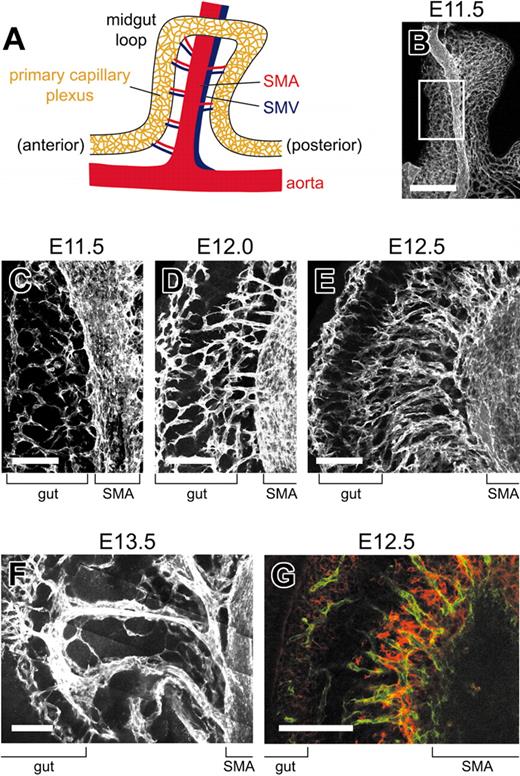
Little is known about the cellular mechanisms of vascularization of the small intestine. The small intestine begins to develop as a simple tube, called a midgut loop, during embryogenesis (Figure 1A). We previously found that in embryonic day 13.5 (E13.5) wild-type embryos, mesenteries connecting the proximal part and the distal part of the midgut loop contained many large branches arising from the superior mesenteric artery (SMA) or superior mesenteric vein (SMV; Figure 1A) but the mesenteries of E13.5 CXCL12–/– or CXCR4–/– embryos contained only smaller branches.6 To elucidate the mechanism responsible for the defects in these mutants, we first studied how these large vessels supplying the small intestine formed in wild-type embryos. Whole-mount antibody staining for PECAM-1 and confocal microscopic analysis were performed to visualize the vasculature. SMA and the primary capillary plexus surrounding the primitive gut were observed as early as E10.5 but the connection between SMA and the capillary plexus was not observed at this stage (data not shown). At E11.5, SMA ran along the proximal part of the midgut loop (Figure 1B) and many short interconnecting vessels between SMA and the neighboring primary capillary plexus surrounding the primitive gut were observed (Figure 1C). Subsequently, those interconnecting vessels had elongated concomitantly to the growth of the mesentery at E12.0, E12.5, and E13.5 (Figure 1D-F). The numbers of interconnecting vessels were reduced from E12.5 to E13.5 (Figure 1E-F). Each interconnecting vessel ran along another vessel connecting to the SMV (Figure 1F and data not shown), suggesting that the interconnecting vessels would become jugnal or ilenium arteries that supply the small intestine throughout adult life. We next examined blood vessel wall morphogenesis by whole-mount immunostaining for smooth muscle α-actin, a smooth muscle cell marker. At E11.5, the expression of smooth muscle α-actin was observed in the cells lining SMA. At E12.5, smooth muscle α-actin expression was seen along the SMA and at the base of interconnecting vessels between SMA and the primary capillary plexus surrounding the primitive gut, suggesting that arteriogenesis was initiated in these interconnecting vessels (Figure 1G).
Vascularization of the small intestine occurs through organ-specific mechanisms. (A) Schematic representation of the small intestine and its vasculature at E13.5. The small intestine develops as a simple tube, called the midgut loop, during ontogeny. (B-G) Whole-mount immunohistochemical analysis of midgut loops from wild-type embryos using pan-endothelial marker PECAM-1 (B-F) or PECAM-1 (green) and smooth muscle α-actin (red) (G). Images were collected by standard confocal microscopy (B-G) and used to build the 3-dimensional projection shown in B-F. (B) At E11.5, SMA runs along the primary capillary plexus surrounding the primitive gut. (C) Proximal part of mesentery and midgut loop boxed in B. Many short interconnecting vessels form between SMA and the neighboring capillary plexus. (D-G) Proximal parts of mesenteries and midgut loops at E12.0 (D), E12.5 (E, G), and E13.5 (F). The interconnecting vessels between SMA and the neighboring capillary plexus have elongated at E12.0, E12.5, and E13.5 (D-F). Each interconnecting vessel runs along the vein at E13.5 (F). (G) An optical slice is shown. Arteriogenesis has been initiated in the interconnecting vessels at E12.5. Bars: B, 500 μm; C-G, 100 μm.
Vascularization of the small intestine occurs through organ-specific mechanisms. (A) Schematic representation of the small intestine and its vasculature at E13.5. The small intestine develops as a simple tube, called the midgut loop, during ontogeny. (B-G) Whole-mount immunohistochemical analysis of midgut loops from wild-type embryos using pan-endothelial marker PECAM-1 (B-F) or PECAM-1 (green) and smooth muscle α-actin (red) (G). Images were collected by standard confocal microscopy (B-G) and used to build the 3-dimensional projection shown in B-F. (B) At E11.5, SMA runs along the primary capillary plexus surrounding the primitive gut. (C) Proximal part of mesentery and midgut loop boxed in B. Many short interconnecting vessels form between SMA and the neighboring capillary plexus. (D-G) Proximal parts of mesenteries and midgut loops at E12.0 (D), E12.5 (E, G), and E13.5 (F). The interconnecting vessels between SMA and the neighboring capillary plexus have elongated at E12.0, E12.5, and E13.5 (D-F). Each interconnecting vessel runs along the vein at E13.5 (F). (G) An optical slice is shown. Arteriogenesis has been initiated in the interconnecting vessels at E12.5. Bars: B, 500 μm; C-G, 100 μm.
CXCL12 and CXCR4 are essential specifically for the formation of short interconnecting vessels between SMA and the neighboring primary capillary plexus surrounding the primitive gut
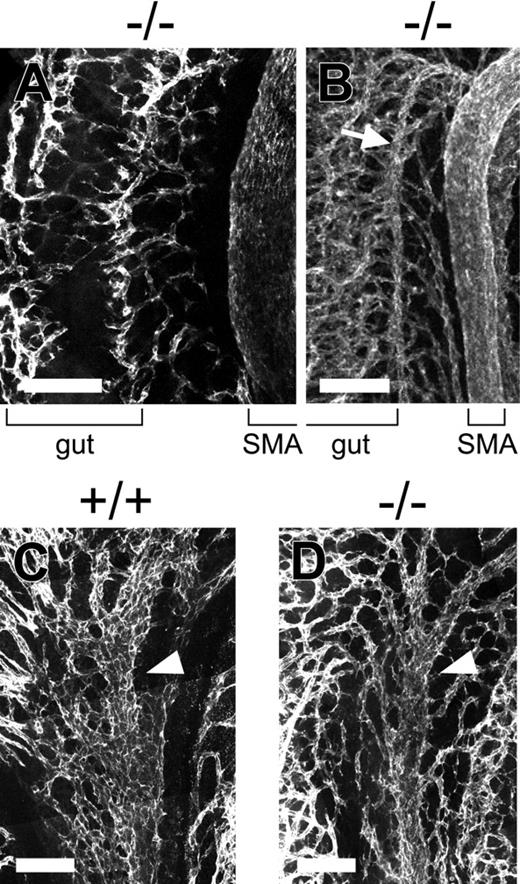
We next examined the vascularization of the small intestine in CXCL12–/– or CXCR4–/– embryos by whole-mount fluorescence and confocal microscopic analysis. In the CXCL12–/– or CXCR4–/– embryos, the formation of SMA and the primary capillary plexus surrounding the primitive gut appeared normal at E10.5, E11.5, and E12.5. However, the interconnecting vessels between SMA and the capillary plexus surrounding the primitive gut were almost absent in CXCL12–/– or CXCR4–/– embryos compared with wild-type embryos from E11.5 onward (Figure 1E, Figure 2A, and data not shown). In these mutants, a collateral vessel that arises from SMA around the apex of the midgut loop and that might supply the mutant gut was found (Figure 2B). In contrast, SMV and the venous network connecting to SMV appeared normal in the E12.5 mutants (Figure 2C-D). To confirm this result, we used antibodies against mucosal addressin cell adhesion molecule 1, which has been shown to be expressed specifically in venous endothelial cells in mesenteries during embryogenesis.28 There was no significant difference in the venous network pattern in mesenteries between wild-type and mutant embryos at E12.5 (data not shown). Immunostaining for PECAM-1 and smooth muscle α-actin revealed that cells expressing smooth muscle α-actin were not observed along SMV and the venous network and that wild-type mice and mutant mice were indistinguishable with the location and distribution of smooth muscle cells surrounding SMAs (data not shown). Thus, these results demonstrated that CXCL12 and CXCR4 are essential specifically for the formation of the interconnecting vessels between SMA and the neighboring capillary plexus surrounding the primitive gut.
CXCL12 is essential for the formation of interconnecting vessels between SMA and the primary capillary plexus surrounding the primitive gut but not the venous network. Whole-mount immunohistochemical analysis of midgut loops from wild-type or CXCL12–/– embryos using pan-endothelial marker PECAM-1. Images were collected by standard confocal microscopy and used to build the 3-dimensional projection shown here. (A) The interconnecting vessels between SMA and the primary capillary plexus surrounding the primitive gut are almost absent in E12.5 CXCL12–/– embryos. (B) A collateral (arrow) arises from SMA around the apex of the midgut loop in the mutants. (C, D) There is no significant difference in SMV (arrowheads) and the venous network arising from SMV between E12.5 wild-type (C) and CXCL12–/– (D) embryos. Bars, 100 μm.
CXCL12 is essential for the formation of interconnecting vessels between SMA and the primary capillary plexus surrounding the primitive gut but not the venous network. Whole-mount immunohistochemical analysis of midgut loops from wild-type or CXCL12–/– embryos using pan-endothelial marker PECAM-1. Images were collected by standard confocal microscopy and used to build the 3-dimensional projection shown here. (A) The interconnecting vessels between SMA and the primary capillary plexus surrounding the primitive gut are almost absent in E12.5 CXCL12–/– embryos. (B) A collateral (arrow) arises from SMA around the apex of the midgut loop in the mutants. (C, D) There is no significant difference in SMV (arrowheads) and the venous network arising from SMV between E12.5 wild-type (C) and CXCL12–/– (D) embryos. Bars, 100 μm.
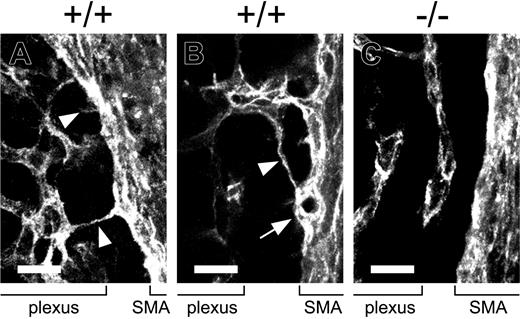
Filopodial extension and intussusception from endothelial cells of SMA seen in wild-type embryos are absent in CXCL12–/– or CXCR4–/– embryos
Next, to determine the mechanism regulating the formation of interconnecting vessels between SMA and the neighboring primary capillary plexus surrounding the primitive gut, detailed analysis of the endothelial cells of SMA from E11.5 wild-type, CXCL12–/–, or CXCR4–/– embryos was done by immunohistostaining and confocal microscopy. Higher magnification of PECAM-1–stained wild-type embryos demonstrated filopodial extension (Figure 3A-B) and intussusception (Figure 3B), which is a hallmark of nonsprouting angiogenesis, from endothelial cells of SMA. The filopodial processes connected to the adjacent primary capillary plexus surrounding the primitive gut, and we did not find the sprout tips of vessel branches from SMA, suggesting that the filopodial processes immediately after sprouting from SMA made contact with the neighboring capillary plexus (Figure 3A-B). In contrast, in CXCL12–/– or CXCR4–/– embryos, filopodial extension, and intussusception from endothelial cells of SMA were barely detectable (Figure 3C and data not shown).
CXCL12 is essential for filopodial extension and intussusception from endothelial cells of SMA. Whole-mount immunohistochemical analysis of midgut loops from wild-type (A, B) or CXCL12–/– (C) embryos. Images were collected by standard confocal microscopy and used to build the 3-dimensional projection shown here. (A, B) Higher magnification of PECAM-1–stained E11.5 wild-type embryos demonstrates filopodial extension (A-B, arrowheads) and intussusception (B, arrow) from endothelial cells of SMA. The filopodial processes that arise from the endothelial cells of SMA connect to the primary capillary plexus surrounding the primitive gut. (C) Higher magnification of PECAM-1–stained E11.5 CXCL12–/– embryos reveals that filopodial extension and intussusception from endothelial cells of SMA are undetectable in CXCL12–/– embryos. Bars, 20 μm.
CXCL12 is essential for filopodial extension and intussusception from endothelial cells of SMA. Whole-mount immunohistochemical analysis of midgut loops from wild-type (A, B) or CXCL12–/– (C) embryos. Images were collected by standard confocal microscopy and used to build the 3-dimensional projection shown here. (A, B) Higher magnification of PECAM-1–stained E11.5 wild-type embryos demonstrates filopodial extension (A-B, arrowheads) and intussusception (B, arrow) from endothelial cells of SMA. The filopodial processes that arise from the endothelial cells of SMA connect to the primary capillary plexus surrounding the primitive gut. (C) Higher magnification of PECAM-1–stained E11.5 CXCL12–/– embryos reveals that filopodial extension and intussusception from endothelial cells of SMA are undetectable in CXCL12–/– embryos. Bars, 20 μm.
CXCR4 is specifically expressed in arteries and this expression requires CXCL12 in the developing mesenteries
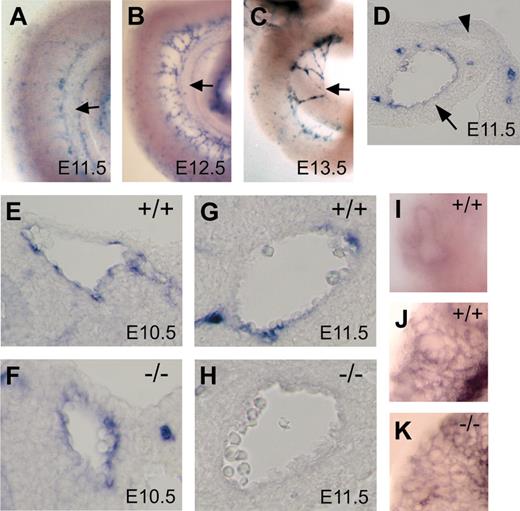
The result that the defects in blood vessel formation in CXCL12–/– or CXCR4–/– mice were specific to arteries prompted us to compare the expression of CXCR4 in arteries with that in veins. Whole-mount in situ hybridization analysis revealed that CXCR4 expression was observed predominantly in SMA but not in the capillary plexus surrounding the primitive gut at E10.5 (data not shown) and E11.5 (Figure 4A). At E12.5, CXCR4 was expressed only in SMA and newly formed branches arising from SMA (Figure 4B). At E13.5, CXCR4 was expressed in large branches arising from SMA but not in SMA, per se (Figure 4C). Analysis of the transverse sections of the E11.5 and E12.5 midgut loop revealed that CXCR4 was detected in endothelial cells of SMA and branches arising from SMA but not in SMV (Figure 4D,G and data not shown). Thus, these results revealed that CXCR4 was expressed predominantly in arteries in developing mesenteries.
Characteristic expression of CXCR4 in developing mesenteries. (A-I) Whole-mount in situ hybridization analysis of CXCR4. Whole-mount view of the midgut loops from wild-type embryos at E11.5 (A), E12.5 (B), and E13.5 (C). CXCR4 expression is observed predominantly in SMA (A, B) and newly formed branches arising from SMA (B, C) but not in the primary capillary plexus surrounding the primitive gut (A-C). Arrows indicate SMA (A-C). (D) Analysis of the transverse sections of E11.5 midgut loop. CXCR4 is detected in endothelial cells of SMA (arrow) but not in those of SMV (arrowhead). (E-H) Analysis of the transverse sections of the midgut loop from wild-type and CXCL12–/– embryos at E10.5 (E, F) and E11.5 (G, H). (E, F) CXCR4 expression is observed in SMA from wild-type and CXCL12–/– embryos at E10.5. (G, H) Note the severe reduction of CXCR4 expression in CXCL12–/– embryos at E11.5. (I) Whole-mount view of the lung from wild-type embryos at E12.5. (J, K) Whole-mount immunohistochemical analysis of the lungs from wild-type (J) and CXCL12–/– (K) embryos at E12.5 using pan-endoth elial marker PECAM-1. CXCR4 expression is not observed in blood vessels of the lung (I, J) and vascular defects are not observed in the mutant lung (K).
Characteristic expression of CXCR4 in developing mesenteries. (A-I) Whole-mount in situ hybridization analysis of CXCR4. Whole-mount view of the midgut loops from wild-type embryos at E11.5 (A), E12.5 (B), and E13.5 (C). CXCR4 expression is observed predominantly in SMA (A, B) and newly formed branches arising from SMA (B, C) but not in the primary capillary plexus surrounding the primitive gut (A-C). Arrows indicate SMA (A-C). (D) Analysis of the transverse sections of E11.5 midgut loop. CXCR4 is detected in endothelial cells of SMA (arrow) but not in those of SMV (arrowhead). (E-H) Analysis of the transverse sections of the midgut loop from wild-type and CXCL12–/– embryos at E10.5 (E, F) and E11.5 (G, H). (E, F) CXCR4 expression is observed in SMA from wild-type and CXCL12–/– embryos at E10.5. (G, H) Note the severe reduction of CXCR4 expression in CXCL12–/– embryos at E11.5. (I) Whole-mount view of the lung from wild-type embryos at E12.5. (J, K) Whole-mount immunohistochemical analysis of the lungs from wild-type (J) and CXCL12–/– (K) embryos at E12.5 using pan-endoth elial marker PECAM-1. CXCR4 expression is not observed in blood vessels of the lung (I, J) and vascular defects are not observed in the mutant lung (K).
Next, to unravel the mechanisms controlling the expression of CXCR4, we examined CXCR4 expression in CXCL12–/– embryos by in situ hybridization analysis. CXCR4 expression was seen in SMA from both wild-type and CXCL12–/– embryos at E10.5 (Figure 4E-F). However, CXCR4 expression was severely diminished in the absence of CXCL12 at E11.5 and E12.5, suggesting that CXCL12 plays a critical role in maintaining CXCR4 expression in endothelial cells of SMA (Figure 4G-H and data not shown).
In situ hybridization analysis demonstrated that CXCR4 was not expressed in blood vessels of the organs including lung or brain at E12.5 or E13.5 (Figure 4I-J and data not shown). Immunostaining for PECAM-1 revealed that vascular defects were not observed in these organs in CXCL12–/– or CXCR4–/– embryos (Figure 4K and data not shown). Thus, the expression of CXCR4 may contribute to the specificity of the defects in vasculature in the mutants.
CXCL12-expressing cells are located in the vicinity of endothelial cells of SMA and along their sprouts in the developing mesenteries
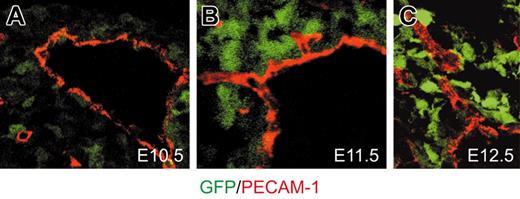
Expression of CXCL12 in developing mesenteries was analyzed using mice in which GFP was knocked into the CXCL12 locus (CXCL12/GFP knock-in mice) at E10.5 and E11.5 (Figure 5A-B). At E11.5, the cells expressing high-level GFP appeared in the vicinity of endothelial cells of SMA at the roots of sprouts from SMA and along the sprouts (Figure 5B-C). The cells expressing CXCL12 did not express smooth muscle α-actin (data not shown), indicating that CXCL12-expressing cells are different from smooth muscle cells. The CXCL12 expression was unaltered in CXCR4–/– embryos (data not shown). Thus, it is likely that CXCL12 produced by CXCL12-expressing cells acts on adjacent endothelial cells of SMA to up-regulate the CXCR4 expression and induce the formation of interconnecting vessels between SMA and the neighboring primary capillary plexus surrounding the primitive gut. Next, we examined the expression of VEGF-A in the CXCL12-expressing cells in the mesenteries. VEGF-A is a cytokine that is well known to be crucial for embryonic vascular formation.29,30 Immunohistochemical staining using CXCL12/GFP knock-in mice revealed that almost all of CXCL12-expressing cells expressed VEGF-A (data not shown). However, many VEGF-A–expressing cells did not express CXCL12 (data not shown).
Location of CXCL12-expressing cells in developing mesenteries. Sections of E10.5 (A), E11.5 (B), and E12.5 (C) midgut loops from CXCL12/GFP knock-in mice were stained with antibodies against PECAM-1 (red). Images were collected by standard confocal microscopy and optical slices are shown. (B, C) Cells expressing high-level CXCL12/GFP (green) are observed to accumulate in patches adjacent to endothelial cells of SMA (B) and along the sprouts from SMA (C).
Location of CXCL12-expressing cells in developing mesenteries. Sections of E10.5 (A), E11.5 (B), and E12.5 (C) midgut loops from CXCL12/GFP knock-in mice were stained with antibodies against PECAM-1 (red). Images were collected by standard confocal microscopy and optical slices are shown. (B, C) Cells expressing high-level CXCL12/GFP (green) are observed to accumulate in patches adjacent to endothelial cells of SMA (B) and along the sprouts from SMA (C).
Endothelial CXCR4 is required for vascularization of the gastrointestinal tracts
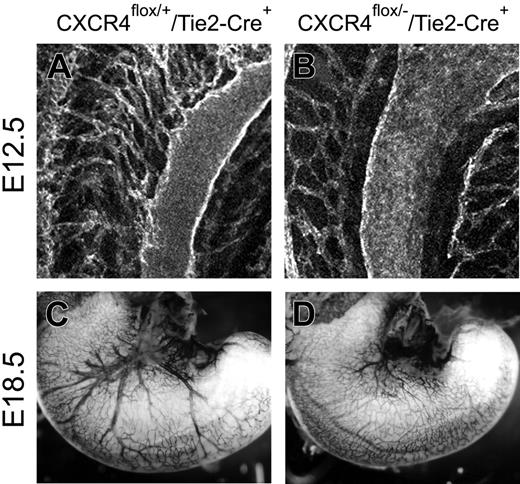
To confirm the idea that CXCR4 expression in endothelial cells is essential for vascularization of the gastrointestinal tract, we generated conditional CXCR4-deficient mice in which CXCR4 was specifically deleted in the endothelium. Conditional deletion of the CXCR4 flox allele was achieved with transgenic mice with the Tie2 kinase promoter/enhancer expression cassette, which gave uniform expression of Cre recombinase (Cre) in all endothelial cells both in the adult and embryo.27,31 The Tie2-Cre transgenic mice were crossed to CXCR4flox/flox mice and the resultant progeny were crossed to CXCR4+/– mice. Whole-mount immunostaining for PECAM-1 revealed that CXCR4flox/–/Tie2-Cre embryos had defects in vascularization of the small intestine and stomach that were identical to those seen in the conventional CXCR4–/– embryos (Figure 6A-D). Like CXCL12–/– and CXCR4–/– embryos, the numbers of interconnecting vessels between SMA and the neighboring primary capillary plexus surrounding the primitive gut were severely reduced (Figure 6A-B), and filopodial extension and intussusception from endothelial cells of SMA were almost absent in the CXCR4flox/–/Tie2-Cre embryos as compared with CXCR4flox/+/Tie2-Cre embryos (data not shown). These results suggest that CXCR4 is required specifically in endothelial cells for the formation of the interconnecting vessels between SMA and the neighboring primary capillary plexus surrounding the primitive gut.
CXCR4 expressed in endothelial cells is required for vascularization of the gastrointestinal tracts. Whole-mount PECAM-1 staining of E12.5 midgut loops (A, B) and E18.5 stomachs (C, D). (A, B) Images were collected by standard confocal microscopy and used to build the 3-dimensional projection shown here. The interconnecting vessels between SMA and the primary capillary plexus surrounding the primitive gut seen in CXCR4flox/+/Tie2-Cre embryos (A) are absent in CXCR4flox/–/Tie2-Cre embryos (B). (C, D) Whole-mount view of the stomach. The large vessels distributed to the surface of the stomach seen in CXCR4flox/+/Tie2-Cre embryos (C) are absent in CXCR4flox/–/Tie2-Cre embryos (D).
CXCR4 expressed in endothelial cells is required for vascularization of the gastrointestinal tracts. Whole-mount PECAM-1 staining of E12.5 midgut loops (A, B) and E18.5 stomachs (C, D). (A, B) Images were collected by standard confocal microscopy and used to build the 3-dimensional projection shown here. The interconnecting vessels between SMA and the primary capillary plexus surrounding the primitive gut seen in CXCR4flox/+/Tie2-Cre embryos (A) are absent in CXCR4flox/–/Tie2-Cre embryos (B). (C, D) Whole-mount view of the stomach. The large vessels distributed to the surface of the stomach seen in CXCR4flox/+/Tie2-Cre embryos (C) are absent in CXCR4flox/–/Tie2-Cre embryos (D).
Discussion
In this study, we have unraveled the organ-specific mechanisms of vascularization of the small intestine at the cellular and molecular levels. Previous studies using quail/chick interspecies transplants have revealed that the gut is vascularized by vasculogenesis and contains intrinsic endothelial cells.4 We have shown that the major artery designated SMA runs along the intrinsic primary capillary plexus surrounding the gut and many short interconnecting vessels form between SMA and the neighboring plexus. Because the tips of sprouts from SMA were not observed, the endothelial processes immediately after extension from SMA and the capillary plexus might coalesce. Subsequently, those interconnecting vessels elongate and some of these vessels would become jugnal or ilenium arteries, which supply the small intestine throughout adult life. It has been thought previously that, in vascularization of many organs, sprouts from preexisting larger arteries or capillary plexus extend into avascular tissues.3,32 However, our results demonstrate a novel organ-specific mechanism of vascularization. In addition, we have shown that formation of interconnecting vessels between SMA and the neighboring primary capillary plexus surrounding the primitive gut depends on a chemokine CXCL12 and its receptor CXCR4. Detailed analysis of the endothelial cells of SMA from CXCL12–/– and CXCR4–/– embryos raises the possibility that CXCL12 plays an essential role in filopodial extension and intussusception from endothelial cells of SMA. This is consistent with the previous in vitro studies that have shown that CXCL12 induces the formation of cell-surface projections in small-cell lung cancer cells33 and axon elongation in cultured cerebellar granule neurons.34 Intersomitic vessels are well characterized and have contributed a model system in which to study the mechanisms of vascular patterning with vessels that sprout from the larger artery. Analysis using CXCL12–/– and CXCR4–/– embryos has revealed that CXCL12 and CXCR4 are dispensable for the formation of intersomitic arteries (data not shown). In intersomitic vessel formation, the sprouts from the dorsal aorta extend into avascular tissues.32,35 Thus, we hypothesize that blood vessel formation in which larger arteries and the capillary plexus coalesce depends on CXCL12 and CXCR4 and this may be an explanation for the organ-specific role of CXCL12 and CXCR4 in blood vessel formation.
Our results have shown that CXCR4 is expressed in arteries but not in veins in developing mesenteries. Consistent with this, the formation of arterial branches but not a venous network was affected in the mesenteries from CXCL12–/– or CXCR4–/– embryos. In addition, CXCR4 was not expressed in vasculature of the organs, including lung or brain at E12.5 or E13.5. Vascular defects were not observed in these organs. These results indicate that CXCL12 is the factor specific to arterial endothelial cells during ontogeny and raise the possibility that the expression of CXCR4 contributes to the specificity of the CXCL12/CXCR4 functions in blood vessel formation. Why was CXCR4 expression detected only in endothelial cells of developing SMA and newly formed branches of SMA? It is possible that factors that up-regulate the CXCR4 expression are produced by the primary gut, including endothelial cells of the capillary plexus located along SMA. Since the expression of CXCR4 in SMA was unaffected at E10.5 but severely diminished in the absence of CXCL12 at E11.5 and E12.5, CXCR4 expression in the artery became dependent on CXCL12 at E11.5. It has been previously reported that hypoxia induces CXCR4 expression through activation of the transcription factor hypoxia-inducible factor-136 or inactivation of von Hippel-Lindau tumor suppressor protein (pVHL)37,38 in endothelial cells or tumor cells, respectively. In addition, prostaglandin E2 has been shown to augment CXCR4 expression on human microvascular endothelial cells.39 Thus, our results demonstrated a novel mechanism for CXCR4 up-regulation in endothelial cells.
The analysis using CXCL12/GFP knock-in mice revealed that the cells expressing high-level GFP appeared in the vicinity of endothelial cells in SMA at the roots of sprouts at E11.5 when these sprouts begin to form. Thus, there is the possibility that CXCL12 guides the initial positioning of filopodial extension and intussusception from endothelial cells of SMA. It will be interesting to unravel the regulatory mechanisms for CXCL12-expressing cell behavior in developing mesenteries.
We have shown that mice in which lineage-specific deletion of CXCR4 was accomplished by the use of Tie2 kinase promoter/enhancer reveal defects identical to those observed in the conventional CXCR4–/– mesenteries. This supports the notion that CXCL12 acts on endothelial cells to regulate vascularization of the gastrointestinal tract. We cannot, however, exclude the possibility that the defects of the blood vessel formation in the mutants might be due to defects in the function of hematopoietic cells,40 since Tie2 is also expressed in a small population of hematopoietic cells including HSCs41 as well as vascular endothelial cells. However, some CXCR4flox/–/Tie2-Cre embryos in which hematopoiesis was largely normal by flow cytometric analysis also displayed deficits in blood vessel formation in the gastrointestinal tract, phenocopying the vascular phenotype of conventional CXCR4-deficient embryos (data not shown), supporting the idea that the defects in blood vessel formation in the CXCR4flox/–/Tie2-Cre embryos were due to the deficits in endothelial cells.
VEGF-A is a cytokine that is crucial for embryonic vascular formation.29,30 VEGF-A has been thought to be important for vascular sprouting during angiogenesis as well as vasculogenesis. For example, it has been reported that VEGF-A is essential for the outgrowth of intersomitic vessels, which sprout from the aorta,29,42 and that heparin-binding VEGF-A is required for lateral extensions of filopodia at the tips of microvessel sprouts from perineural vascular plexus in hindbrain.43 VEGF-A was ubiquitously expressed in developing mesenteries (data not shown). In addition, Flk-1, a receptor for VEGF-A, was expressed in all endothelial cells of SMA as well as SMV (data not shown). Thus, VEGF-A is likely to act in concert with CXCL12. In this case, vascularization of organs would require VEGF-A as well as organ-specific factors such as CXCL12. Further studies will be required to reveal the role of VEGF-A in vascularization of the small intestine during ontogeny.
We have demonstrated the role of CXCL12 and CXCR4 in the formation of arteries that supply the small intestine. Factors involved in embryonic blood vessel formation are thought to regulate adult angiogenesis in pathologic conditions.2 In particular, tumor vessels grow by various mechanisms.44 Therefore there is the possibility that in some tumors pathologic angiogenesis occurs through this CXCL12-mediated mechanism, in which the larger artery and the neighboring capillary plexus coalesce. Thus, this study provides insights into the cellular and molecular mechanisms of organ-specific blood vessel formation.
Prepublished online as Blood First Edition Paper, December 30, 2004; DOI 10.1182/blood-2004-07-2563.
Supported by a Research for the Future Program grant of The Japanese Society for the Promotion of Science, Sports and Culture of Japan and by Establishment of International COE for Integration of Transplantation Therapy and Regenerative Medicine (COE program of the Ministry of Education, Culture, Sports, Science and Technology, Japan).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank T. Egawa, J. Yoshida, K. Matsumoto, E. Yoshimura, and M. Satoh for technical assistance.