Abstract
The objective of this study was to investigate whether the immunostimulatory properties of human monocyte-derived dendritic cells (DCs) could be enhanced by triggering OX40/OX40L signaling. Since monocyte-derived DCs possess only low-cell surface levels of OX40L in the absence of CD40 signaling, OX40L was expressed by transfection of DCs with the corresponding mRNA. We show that OX40L mRNA transfection effectively enhanced the immunostimulatory function of DCs at multiple levels: OX40L mRNA transfection augmented allogeneic and HLA class II epitope-specific CD4+ T-cell responses, improved the stimulation of antigen-specific cytotoxic T lymphocytes (CTLs) in vitro without interfering with the prostaglandin E2 (PGE2)–mediated migratory function of the DCs, and facilitated interleukin 12 p70 (IL-12p70)–independent T helper type 1 (Th1) polarization of naive CD4+ T-helper cells. Furthermore, vaccination of tumor-bearing mice using OX40L mRNA–cotransfected DCs resulted in significant enhancement of therapeutic antitumor immunity due to in vivo priming of Th1-type T-cell responses. Our data suggest that transfection of DCs with OX40L mRNA may represent a promising strategy that could be applied in clinical immunotherapy protocols, while circumventing the current unavailability of reagents facilitating OX40 ligation.
Introduction
We have previously shown that vaccination with RNA-transfected dendritic cells (DCs) induced therapeutic antitumor immunity in murine tumor models1,2 and stimulated antigen-specific T-cell responses in patients with renal3 or prostate malignancies.4 However, one drawback of using RNA for antigen delivery is that endogenously expressed antigens will be preferentially channeled into the major histocompatibility complex (MHC) class I presentation pathway, thus stimulating primarily CD8+ cytotoxic T lymphocyte (CTL) responses. While CTLs represent an important effector arm in the antitumor response, it has become evident that the concomitant stimulation of antigen-specific CD4+ T-helper cells is a prerequisite for the induction of effective and persistent antitumor immunity.5,6 Therefore, to improve the efficacy of DC vaccines, it will be necessary to develop strategies that enhance the CD4+ T-cell arm of the immune response.
One of the most commonly used protocols for generating mature human DCs involves the differentiation of DCs from CD14+ monocytes, followed by culture in media supplemented with the proinflammatory cytokines tumor necrosis factor α (TNF-α, interleukin 6 (IL-6), IL-1β, and prostaglandin E2 (PGE2) to induce their maturation.7 Studies have shown that the presence of the inflammatory mediator PGE2 during maturation of DCs is a prerequisite for the acquisition of chemotactic responsiveness to lymph node–derived chemokines, such as CC chemokine ligand 19 (CCL19) and CCL21.8,9 Thus, the capacity of DCs to migrate from the periphery to the draining lymph nodes, the site at which priming of T lymphocytes occurs, is dependent on PGE2. Unfortunately, PGE2 impairs the ability of DCs to produce bioactive IL-12p70, a cytokine essential to facilitate naive CD4+ T-cell differentiation toward T helper type 1 (Th1).8,9 Also, it was shown that maturation of monocyte-derived DCs in the presence of PGE2 renders these cells insusceptible to subsequent modulation by immunostimulatory cytokines and also inhibits responsiveness to CD40 ligand (CD40L)–mediated signaling encountered at the lymph node.10
To overcome these obstacles, we tested whether triggering a “downstream” event, namely costimulation of CD4+ T cells via OX40 signaling, could circumvent the PGE2-mediated attenuation of DC function and augment the immunostimulatory efficacy of antigen-presenting DCs matured in the presence of PGE2. The approach that we have taken to facilitate OX40L expression in the absence of CD40L signaling was to transfect DCs with the corresponding mRNA. We hypothesized that costimulation of CD4+ T cells via the OX40/OX40L signaling pathway may enhance the stimulation of antigen-specific CD4+ T cells, thereby augmenting a concomitant CD8+ T-cell response.
We show that OX40L mRNA transfection effectively augmented the immunostimulatory function of monocyte-derived and ex vivo–matured DCs at multiple levels: OX40L signaling facilitated the enhancement of an antigen-specific CD4+ T-cell response, induced Th1-polarizing activity, and improved the induction of antigen-specific CTL responses in vitro without interfering with the PGE2-mediated migratory function of DCs. In addition, vaccination with OX40L mRNA–transfected DCs in mice carrying preestablished B16 melanomas resulted in a significant enhancement of therapeutic antitumor activity due to in vivo priming of Th1-type CD4+ T-cell responses. To our knowledge, this is the first report demonstrating that DC function can be significantly improved by transfection with RNA encoding a costimulatory molecule.
Materials and methods
Cloning of human OX40L cDNA and in vitro transcription of RNA
Total RNA was extracted from DCs using the RNeasy Maxi kit (Qiagen, Valencia, CA) and reverse-transcribed using SuperScript II reverse transcriptase (Invitrogen, Carlsbad, CA). cDNA was amplified by polymerase chain reaction (PCR) using the primers OX40Lsense TATATATCTAGAGCCACCATGGAAAGGGTCCAACCC and OX40Lantisense TATATAGAGCTCCCCCTCAAAGGACACAGAATTCAC (Integrated DNA Technologies, Coralville, IA). The full-length OX40L sequence was then cloned into the pGEM4Z-A64 vector, containing a synthetic poly-A tail, as shown previously.1 OX40L mRNA was generated by in vitro transcription using the mMESSAGEmMACHINE T7 kit (Ambion, Austin, TX).
Generation and electroporation of dendritic cells with RNA
DCs were generated from peripheral blood mononuclear cells (PBMCs) in the presence of IL-4 and granulocyte-macrophage colony-stimulating factor (GM-CSF) and transfected with RNA via electroporation, as described previously.11 After transfection, cells were centrifuged, resuspended in X-VIVO 15 medium (Cambrex Bioscience, Walkersville, MD), and matured for 18 hours in the presence of 10 ng/mL TNF-α, 10 ng/mL IL-1 β, 150 ng/mL IL-6 (R&D Systems, Minneapolis, MN), and 1 μg/mL PGE2 (Cayman Chemicals, Ann Arbor, MI).
Antibodies and reagents
The cytokines and the antibody pairs used for interferon-γ, IL-4, IL-5, and IL-12p70 enzyme-linked immunosorbent assays (ELISAs) were purchased from R&D Systems. Anti–OX40L antibody was obtained from Santa Cruz Biotechnology, Santa Cruz, CA, and Five NH2-terminally deleted epitope-tagged (FLAG)–tagged recombinant OX40L protein was provided by Alexis Biochemicals, San Diego, CA.
Immunologic analysis
CD4+ T cells were isolated from PBMCs by negative depletion (Miltenyi Biotec, Auburn, CA), and cytokine secretion was analyzed by interferon-γ and IL-4 enzyme-linked immunospot (ELISPOT) after short-term stimulation.3 Cytolytic assays were performed by coculturing RNA-transfected DCs with autologous PBMCs at a 1:10 ratio. Cells were restimulated once, and IL-2 (10 U/mL) was added after 5 days and every other day thereafter. After 20 days of culture, effector cells were harvested and analyzed in cytolytic assays. Target cells were labeled with 100 μCi (3.7 MBq) Na2[51CrO4] (NEN, Boston, MA) in 200 μL complete RPMI 1640 for 1 hour at 37°C in 5% CO2, and 51Cr-labeled target cells were incubated in complete RPMI 1640 medium with effector cells for 4 hours at 37°C. Then, 50 μL supernatant was harvested, and release of 51Cr was measured with a γ-counter. Results from triplicate wells were averaged, and the percentage of specific lysis was calculated.
To analyze antigen-specific secretion of Th1/Th2-type cytokines by T cells, the interferon-γ and IL-4 secretion assay detection kits (Miltenyi, Bergisch-Gladbach, Germany) were used according to the protocol provided by the manufacturer. Cytometric bead arrays were performed using the human Th1/Th2 cytokine cytometric bead array kit according to the manufacturer's protocol (BD Biosciences Pharmingen, San Diego, CA). For intracellular staining, 10 μg/mL Brefeldin A (Sigma, St Louis, MO) was added during the last 4 hours of an 8-hour culture period. After stimulation, cells were stained with antibodies against cell surface markers, fixed with 0.5% paraformaldehyde, and permeabilized with 0.5% saponin.
For proliferation assays, negative selection of CD4+ T lymphocytes was performed by magnetic bead separation (Miltenyi). Purified cells were seeded into 96-well round-bottomed microplates (105 cells/well) in the presence of indicated numbers of mRNA-transfected DCs. The final volume of each well was adjusted to 200 μL with complete RPMI 1640 medium. Triplicate wells of T cells alone were used as a background control. After 5 days of culture, 1 μCi (0.037 MBq) [methyl-3H] thymidine (NEN) was added to each well, and incubation was continued for an additional 16 hours. Cells were collected onto glass fiber filters (Wallac, Turku, Finland) with a cell harvester, and uptake of thymidine was determined using a liquid scintillation counter. Stimulation indexes were calculated using the ratio of mean counts-per-minute of DC-induced T-cell proliferation and the mean counts-per-minute of T-cell proliferation in the absence of DCs.
Polarization of CD4+CD45RA+ T cells
Naive CD4+CD45RA+ T cells were isolated by magnetic bead separation (Miltenyi Biotec) and stimulated with allogeneic DCs at a stimulator-to-responder ratio of 1:10. After 5 days, T cells were stimulated with 50 ng/mL phorbol 12-myristate 13-acetate (PMA) and 1 μg/mL ionomycin (Sigma) and analyzed after 6 hours by cytokine secretion assay. For polarization of antigen-specific naive cells, naive CD4+CD45RA+ T cells from a HLA-DR11.5–positive donor were stimulated using autologous DCs loaded with tetanus toxoid (1 FU/mL). After 7 days, cells were restimulated with autologous DCs pulsed with the HLA-DR11.5–restricted helper epitope p30947-967 FNNFTVSFWLRVPKVSASHLE, (EMC Microcollections, Tubingen, Germany) and analyzed in ELISPOT assays.
Migration assays for mRNA-transfected DCs
DCs (1 × 106) were plated into the upper chambers of 6-well transwell plates (8-μm pore size; Costar, Corning, NY). Macrophage inflammatory protein-3β (MIP-3β; 100 ng/mL; PeproTech, Rocky Hill, NJ) was added to the lower chambers, and migration of DCs was assessed after 1 hour at 37°C/5% CO2. DC migration in the absence of chemokine was subtracted as background.
Murine studies
The F10.9 clone of the B16 melanoma of C57BL/6 origin was used for the studies shown in Figure 5. Cells were maintained in Dulbecco modified Eagle medium (DMEM) supplemented with 10% fetal calf serum, 25 mM HEPES (N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid), 2 mM L-glutamine, and 1 mM sodium pyruvate. For generation of DCs, bone marrow from tibias and femurs of C57BL/6 mice was harvested. Bone marrow–derived cells were plated in RPMI 1640 medium supplemented with 5% fetal calf serum and the cytokines GM-CSF (15 ng/mL) and IL-4 (10 ng/mL) (PeproTech). Cells were plated at a concentration of 1 × 106 cells/mL and incubated at 37°C/5% CO2. Three days later, floating cells (mostly granulocytes) were removed, and the adherent cells were replenished with fresh GM-CSF and IL-4–containing medium. Four days later, the nonadherent cells were harvested, washed, and electroporated with RNA. For electroporation, DCs were resuspended in Opti-MEM (GIBCO, Grand Island, NY) at a concentration of 2.5 × 107 cells/mL. The used DC culture media were saved as conditioning media for later use. Cells were electroporated in 2-mm cuvettes at 300V/500μs using an Electro Square Porator ECM 830 (BTX, San Diego, CA). The amount of tyrosinase-related protein 2 (TRP-2) or actin mRNA used for DC transfection was 2 μg/1 × 106 DCs for TRP and 6 μg/1 × 106 for OX40L mRNA. Cells were immediately transferred to 6-well plates containing a 1:1 combination of conditioned DC medium and fresh RPMI 1640 supplemented with GM-CSF and IL-4. Transfected DCs were incubated at 37°C/5% CO2 overnight, washed twice in phosphate-buffered saline (PBS), and then injected into mice. Mice received 2.5 × 104 F10.9 tumor cells subcutaneously into the hind flank. Three days after tumor implantation, mice were immunized intraperitoneally with 3 × 105 RNA-transfected DCs per mouse (suspended in 200 μL PBS) twice, 7 days apart. Tumor growth was measured every other day starting on day 10. Mice were killed once tumors reached 20 mm in diameter.
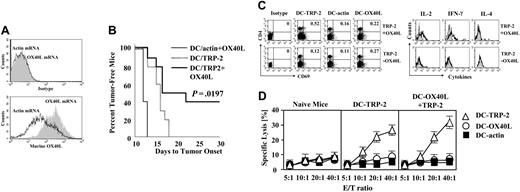
Enhancement of antitumor immunity in mice immunized with OX40L mRNA–cotransfected DCs. (A) Murine DCs (generated from bone marrow precursors in the presence of IL-4 and GM-CSF) were transfected with OX40L or actin (control) mRNA, and OX40L cell-surface expression was determined by flow cytometry. (A, top panel) Isotypic control; (A, bottom panel) staining with anti-OX40L antibody. (B) Mice were inoculated subcutaneously with 2.5 × 104 F10.9 tumor cells. Three days after tumor implantation, mice (n = 10 in each group) were immunized intraperitoneally with 3 × 105 mRNA-transfected DCs twice at 7-day intervals. Tumor growth was evaluated every other day starting on day 10. Mice were killed once the tumor size reached 10 mm in diameter. (C) Splenocytes were isolated from mice vaccinated with TRP-2 mRNA–transfected DCs (TRP-2 – OX40L) or TRP-2/OX40L mRNA–cotransfected DCs (TRP-2 + OX40L). Cells were restimulated for 8 hours using DCs transfected with either TRP-2 mRNA (DC–TRP-2), actin mRNA (DC-actin), or OX40L mRNA (DC-OX40L), with 10 μg/mL Brefeldin A added during the last 4 hours of stimulation. Subsequently, cells were stained with anti-CD4 and anti-CD69 antibodies and analyzed by FACS analysis. Cells were permeabilized and stained with anti–IL-2, anti–IL-4, and anti–IFN-γ antibody. After gating on CD4+CD69+ cells, intracellular levels of cytokines were determined by flow cytometry. (D) Cytolytic assays. Splenocytes were isolated from naive mice, mice vaccinated with TRP-2 mRNA–transfected DCs (DC–TRP-2), and mice vaccinated with TRP-2/OX40L mRNA–transfected DCs (DC–OX40L + TRP-2). Cells were restimulated once with actin mRNA–transfected DCs (DC-actin), TRP-2 mRNA–transfected DCs (DC–TRP-2), and OX40L mRNA–transfected DCs (DC-OX40L). After 5 days, restimulated cells were analyzed in standard chromium release assays for specific killing of TRP-2 mRNA–transfected DCs (▵), actin mRNA–transfected DCs (▪), or OX40L mRNA–transfected DC (○) at the indicated effector-to-target (E/T) ratios.
Enhancement of antitumor immunity in mice immunized with OX40L mRNA–cotransfected DCs. (A) Murine DCs (generated from bone marrow precursors in the presence of IL-4 and GM-CSF) were transfected with OX40L or actin (control) mRNA, and OX40L cell-surface expression was determined by flow cytometry. (A, top panel) Isotypic control; (A, bottom panel) staining with anti-OX40L antibody. (B) Mice were inoculated subcutaneously with 2.5 × 104 F10.9 tumor cells. Three days after tumor implantation, mice (n = 10 in each group) were immunized intraperitoneally with 3 × 105 mRNA-transfected DCs twice at 7-day intervals. Tumor growth was evaluated every other day starting on day 10. Mice were killed once the tumor size reached 10 mm in diameter. (C) Splenocytes were isolated from mice vaccinated with TRP-2 mRNA–transfected DCs (TRP-2 – OX40L) or TRP-2/OX40L mRNA–cotransfected DCs (TRP-2 + OX40L). Cells were restimulated for 8 hours using DCs transfected with either TRP-2 mRNA (DC–TRP-2), actin mRNA (DC-actin), or OX40L mRNA (DC-OX40L), with 10 μg/mL Brefeldin A added during the last 4 hours of stimulation. Subsequently, cells were stained with anti-CD4 and anti-CD69 antibodies and analyzed by FACS analysis. Cells were permeabilized and stained with anti–IL-2, anti–IL-4, and anti–IFN-γ antibody. After gating on CD4+CD69+ cells, intracellular levels of cytokines were determined by flow cytometry. (D) Cytolytic assays. Splenocytes were isolated from naive mice, mice vaccinated with TRP-2 mRNA–transfected DCs (DC–TRP-2), and mice vaccinated with TRP-2/OX40L mRNA–transfected DCs (DC–OX40L + TRP-2). Cells were restimulated once with actin mRNA–transfected DCs (DC-actin), TRP-2 mRNA–transfected DCs (DC–TRP-2), and OX40L mRNA–transfected DCs (DC-OX40L). After 5 days, restimulated cells were analyzed in standard chromium release assays for specific killing of TRP-2 mRNA–transfected DCs (▵), actin mRNA–transfected DCs (▪), or OX40L mRNA–transfected DC (○) at the indicated effector-to-target (E/T) ratios.
Results
OX40L expression by immature or mature DCs
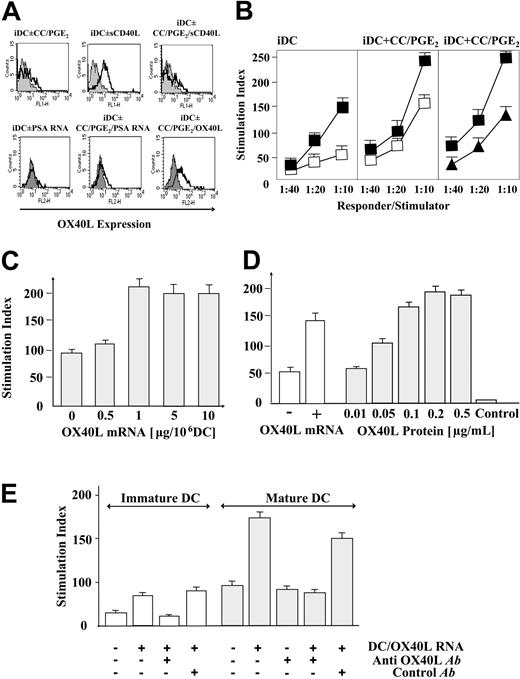
We first analyzed OX40L cell-surface expression by immature DCs or DCs matured using the proinflammatory cytokines TNF-α, IL-1β, IL-6, and PGE2 (cytokine cocktail).12,13 Immature DCs were generated from the PBMCs of healthy volunteers following culture in IL-4 and GM-CSF–containing, serum-free medium.4 Aliquots of the immature DCs were matured either by addition of cytokine cocktail (CC/PGE2) or by using soluble CD40L trimer (sCD40L). Another set of DCs was incubated with sCD40L after maturation with the cytokine cocktail. In all samples, OX40L expression was determined by cell-surface staining and subsequent flow cytometric analysis. As shown in Figure 1A (upper panels), immature DCs (iDCs) and cytokine cocktail–matured DCs (iDCs ± CC/PGE2) exhibited only low amounts of OX40L expression. In contrast, 24-hour exposure of immature DCs to sCD40L triggered significant OX40L up-regulation (iDCs ± CD40L), which was sustained in culture for a minimum of 5 days (data not shown). Interestingly, when sCD40L was added after the DC maturation step (iDCs ± CC/PGE2/sCD40L), no significant increase in OX40L expression was observed, suggesting that cocktail-matured DCs were insusceptible to CD40L-mediated stimuli.
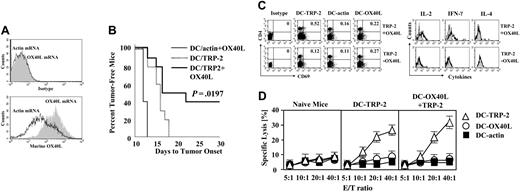
Expression and immunostimulatory function of OX40L on monocyte-derived DCs. (A, top row) OX40L expression was determined by fluorescence-activated cell sorting (FACS) on immature DCs (gray histograms) or 24 hours after maturation with cytokine cocktail/PGE2 (iDCs ± CC/PGE2), with 3 μg/mL soluble trimeric CD40 ligand (iDCs ± sCD40L), or with cytokine cocktail plus sCD40L (iDCs ± CC/PGE2/sCD40L). (A, bottom row) OX40L expression was determined on immature DCs (gray histograms), immature DCs transfected with prostate-specific antigen (PSA) control mRNA (iDCs ± PSA RNA), cocktail-matured and control RNA–transfected DCs (iDCs ± CC/PGE2/PSA RNA), or OX40L-transfected and cocktail-matured DCs (iDCs ± CC/PGE2/OX40L mRNA). (B) Allogeneic mixed lymphocyte reactions (MLRs). Allogeneic CD4+ T cells were stimulated with immature DCs (iDC) or cocktail-matured DCs (iDC + CC/PGE2) at the indicated responder-to-stimulator ratios. DCs were transfected with PSA mRNA (□), green fluorescent protein (GFP) mRNA (▴), or OX40L mRNA (▪). Proliferation was assessed by incorporation of tritiated thymidine. Results are presented as the mean stimulatory index with standard deviation (SD) calculated from triplicate wells. (C) DCs were transfected with increasing amounts of OX40L mRNA, matured with cytokine cocktail, and used as stimulators in an allogeneic MLR at a stimulator-to-responder ratio of 1: 10. (D) Allogeneic MLR in the presence of increasing concentrations of OX40 agonist (recombinant human OX40L protein). Allogeneic CD4+ T cells were incubated with OX40L RNA–transfected and cocktail-matured DCs (+ OX40L mRNA) or control (PSA) RNA–transfected and cocktail-matured DCs (–OX40L mRNA) at a stimulator-to-responder ratio of 1: 10. Increasing amounts of OX40L protein (range, 0.01-0.5 μg/mL) plus anti-FLAG antibody (1 μg/mL) were added to reactions. No stimulation of CD4+ T cells could be observed in the absence of DCs (Control). (E) Allogeneic MLR in the presence of OX40L-neutralizing antibody. Immature or cocktail-matured DCs were transfected with control (PSA) mRNA or OX40L mRNA and used as stimulators for allogeneic CD4+ T cells (stimulator-to-responder ratio, 1:10). Anti-OX40L antibody (5 μg/mL) was added as indicated. As a control, an anti-CD8 antibody (5 μg/mL) was used in these assays. Results are presented as the mean stimulatory index with SD calculated from triplicate wells.
Expression and immunostimulatory function of OX40L on monocyte-derived DCs. (A, top row) OX40L expression was determined by fluorescence-activated cell sorting (FACS) on immature DCs (gray histograms) or 24 hours after maturation with cytokine cocktail/PGE2 (iDCs ± CC/PGE2), with 3 μg/mL soluble trimeric CD40 ligand (iDCs ± sCD40L), or with cytokine cocktail plus sCD40L (iDCs ± CC/PGE2/sCD40L). (A, bottom row) OX40L expression was determined on immature DCs (gray histograms), immature DCs transfected with prostate-specific antigen (PSA) control mRNA (iDCs ± PSA RNA), cocktail-matured and control RNA–transfected DCs (iDCs ± CC/PGE2/PSA RNA), or OX40L-transfected and cocktail-matured DCs (iDCs ± CC/PGE2/OX40L mRNA). (B) Allogeneic mixed lymphocyte reactions (MLRs). Allogeneic CD4+ T cells were stimulated with immature DCs (iDC) or cocktail-matured DCs (iDC + CC/PGE2) at the indicated responder-to-stimulator ratios. DCs were transfected with PSA mRNA (□), green fluorescent protein (GFP) mRNA (▴), or OX40L mRNA (▪). Proliferation was assessed by incorporation of tritiated thymidine. Results are presented as the mean stimulatory index with standard deviation (SD) calculated from triplicate wells. (C) DCs were transfected with increasing amounts of OX40L mRNA, matured with cytokine cocktail, and used as stimulators in an allogeneic MLR at a stimulator-to-responder ratio of 1: 10. (D) Allogeneic MLR in the presence of increasing concentrations of OX40 agonist (recombinant human OX40L protein). Allogeneic CD4+ T cells were incubated with OX40L RNA–transfected and cocktail-matured DCs (+ OX40L mRNA) or control (PSA) RNA–transfected and cocktail-matured DCs (–OX40L mRNA) at a stimulator-to-responder ratio of 1: 10. Increasing amounts of OX40L protein (range, 0.01-0.5 μg/mL) plus anti-FLAG antibody (1 μg/mL) were added to reactions. No stimulation of CD4+ T cells could be observed in the absence of DCs (Control). (E) Allogeneic MLR in the presence of OX40L-neutralizing antibody. Immature or cocktail-matured DCs were transfected with control (PSA) mRNA or OX40L mRNA and used as stimulators for allogeneic CD4+ T cells (stimulator-to-responder ratio, 1:10). Anti-OX40L antibody (5 μg/mL) was added as indicated. As a control, an anti-CD8 antibody (5 μg/mL) was used in these assays. Results are presented as the mean stimulatory index with SD calculated from triplicate wells.
In a second set of experiments (Figure 1A, lower panel), we investigated whether OX40L expression can be induced by transfection with plasmid-derived OX40L mRNA. In parallel, DCs were transfected with control mRNA species encoding PSA or GFP (latter not shown). No significant OX40L induction was noted when control mRNA was transfected into immature (iDCs ± PSA RNA) or cocktail-matured DCs (iDCs ± CC/PGE2/PSA RNA). In contrast, high-level OX40L expression (range, 45-65%) was observed when immature DCs were transfected with OX40L mRNA (iDCs ± CC/PGE2/OX40L).
In summary, these experiments suggest that immature and cocktail-matured DCs express only low levels of OX40L on their cell surface and that cytokine cocktail–induced maturation renders DCs unresponsive to CD40L-mediated stimuli. It appears, however, that this obstacle can be overcome by transfection of DCs with mRNA encoding the costimulatory molecule OX40L.
Optimization and functional validation of OX40L mRNA transfection
Next, we determined whether mRNA-mediated expression of OX40L was capable of augmenting the allostimulatory capacity of cocktail-matured DCs. As shown in Figure 1B, transfection of immature (iDCs) or cocktail-matured DCs (iDCs + CC/PGE2) with OX40L mRNA (▪) but not PSA mRNA (□) or GFP mRNA (▴) consistently resulted in a marked increase in CD4+ T-cell proliferation in allogeneic MLRs.
Next, we transfected immature DCs with increasing amounts of OX40L mRNA (range, 0-10 μg/106 cells) and matured these cells using cytokine cocktail. The immunostimulatory function of the transfected DCs was then evaluated in allogeneic MLRs. As shown in Figure 1C, optimal stimulation of CD4+ T-cell proliferation could be achieved using OX40L mRNA concentrations of 1 μg/106 cells and higher, while concentrations lower than 1 μg/106 cells resulted in significantly inferior allostimulatory capacity.
Having determined the optimal OX40L mRNA concentration for DC transfection, we compared the OX40L mRNA–driven stimulation of T-cell proliferation with the level of T-cell activation that can be achieved by using an OX40 agonist. As an agonist for OX40, we chose a recombinant OX40L protein that contains a FLAG-tag that allows cross-linking of OX40L protein with an anti-FLAG antibody (enhancer). Allogeneic CD4+ T cells were incubated with either OX40L or control mRNA–transfected mature DCs (Figure 1D). In parallel, mature DCs were incubated with increasing concentrations of both OX40L protein and enhancer over a 4-day period. Optimal stimulation of T-cell proliferation could be observed using OX40L protein concentrations of 0.2 μg/mL or higher, while OX40L protein alone (Control) had no direct stimulatory effect on CD4+ T cells, which is consistent with the fact that T cells express OX40 only after activation of their T-cell receptor.14 As demonstrated by the experiments shown in Figure 1D, the level of CD4+ T-cell proliferation achieved by using OX40L mRNA–transfected DCs was approximately 80% of the level achieved by using saturating concentrations of OX40 protein.
To provide direct evidence that OX40L mRNA transfection is capable of enhancing the immunostimulatory properties of DCs, we also performed blocking experiments using an anti–human OX40L antibody in allogeneic MLR reactions. OX40L mRNA–transfected immature and cytokine cocktail–matured DCs were used as stimulators for allogeneic CD4+ T cells. Previous analyses on OX40L mRNA–transfected DCs revealed that the saturating amounts of blocking antibody were 5 μg/mL (data not shown). As shown in Figure 1E, OX40L mRNA transfection significantly increased the allostimulatory capacity of both immature and mature DCs in vitro. In contrast, OX40L-blocking antibody (Anti-OX40L Ab) led to complete inhibition of the observed OX40L-driven CD4+ T-cell stimulation, while the addition of anti-CD8 antibody (Control Ab) did not significantly inhibit T-cell proliferation.
In summary, these data show that enhanced OX40L expression on DCs potentiates the proliferative capacity of allogeneic CD4+ T cells in vitro and that this effect can be reversed by using OX40L-blocking antibody. Optimized conditions for mRNA transfection resulted in T-cell proliferation levels that were 80% of the level achieved by using an agonistic OX40L protein. Although prior studies suggested that RNA in itself induces, albeit modest, DC activation and up-regulation of the maturation marker CD83,4,15 DCs transfected with control mRNA encoding PSA or GFP did not significantly affect OX40L cell surface expression or enhanced CD4+ T-cell proliferative capacity.
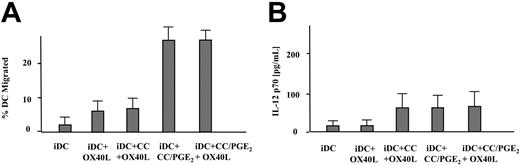
Migratory and IL-12p70 secretory function
Next, we analyzed whether OX40L mRNA transfection affects the migratory and IL-12p70 secretory capacity of DCs in vitro. Immature and mature DCs were generated as described in the experiments shown in Figure 1, and their migratory capacity toward a chemokine (MIP3-β) gradient was determined in transwell assays. IL-12p70 secretion was measured by ELISA. As shown in Figure 2A, immature DCs (iDCs) exhibited only background levels of migration, while DCs that were matured in the presence of PGE2 acquired high-level migratory function (iDCs + CC/PGE2; iDCs + CC/PGE2/OX40L). DC migration was clearly dependent on the presence of PGE2 within the maturation cocktail, while OX40L mRNA transfection contributed little to the chemotactic responsiveness of DCs when PGE2 was omitted (iDCs + OX40L; DCs + CC + OX40L). Furthermore, as shown in Figure 2B, IL-12p70 secretion by mature or immature DCs did not change significantly after OX40L mRNA transfection, regardless of whether PGE2 was used for maturation or not.
In vitro migration and IL-12p70 secretion of OX40L mRNA–transfected DCs. (A) Migration of immature DCs (iDC), OX40L mRNA–transfected immature DCs (iDC + OX40L), OX40L mRNA–transfected and cytokine cocktail (without PGE2)–matured DCs (iDC + CC + OX40L), immature DCs matured with cytokines plus PGE2 (iDC + CC/PGE2), or OX40L mRNA–transfected and cytokine cocktail/PGE2–matured DCs (iDC + CC/PGE2 + OX40L) toward a MIP-3β gradient in transwell assays with SD (error bars) calculated from triplicate wells. (B) The same cell preparations were analyzed for secretion of bioactive IL-12p70 by ELISA. Results are presented as mean percentage of migrated cells with SD calculated from triplicate wells.
In vitro migration and IL-12p70 secretion of OX40L mRNA–transfected DCs. (A) Migration of immature DCs (iDC), OX40L mRNA–transfected immature DCs (iDC + OX40L), OX40L mRNA–transfected and cytokine cocktail (without PGE2)–matured DCs (iDC + CC + OX40L), immature DCs matured with cytokines plus PGE2 (iDC + CC/PGE2), or OX40L mRNA–transfected and cytokine cocktail/PGE2–matured DCs (iDC + CC/PGE2 + OX40L) toward a MIP-3β gradient in transwell assays with SD (error bars) calculated from triplicate wells. (B) The same cell preparations were analyzed for secretion of bioactive IL-12p70 by ELISA. Results are presented as mean percentage of migrated cells with SD calculated from triplicate wells.
The experiments shown in Figure 2 underscore the critical role of PGE2 in facilitating migration of monocyte-derived DCs. These data also demonstrate that transfection of DCs with OX40L mRNA neither negatively affected DC migration nor affected IL-12p70 secretion.
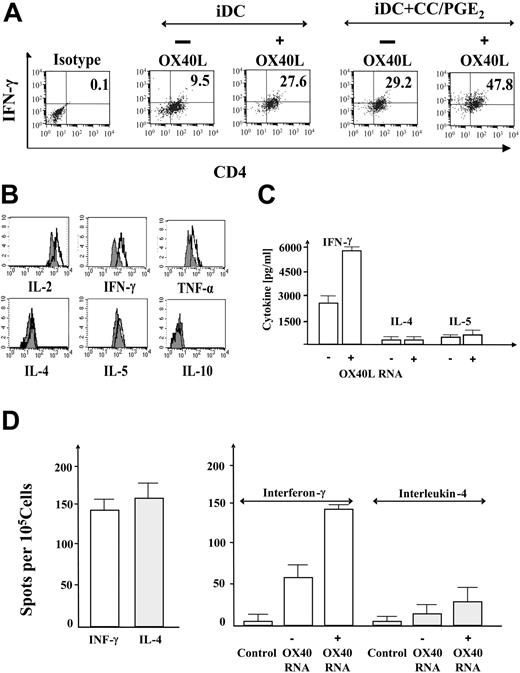
DCs transfected with OX40L mRNA can enhance a Th1-biased CD4+ T-cell response in the presence of PGE2
To provide further evidence that the cocktail-matured, OX40L mRNA–transfected DCs are capable of improving the CD4 T-cell arm of the immune response, we analyzed the effects of OX40L mRNA transfection on the polarization of naive CD4+ T cells. Naive CD4+CD45RA+ cells were stimulated with allogeneic DCs. After 5 days, T cells were exposed to PMA/ionomycin and analyzed for production of the Th1 cytokine interferon-γ, or the Th2 cytokine IL-4 (data not shown) by flow cytometry–based cytokine secretion assays. As shown in Figure 3A, OX40L mRNA transfection of cocktail-matured DCs significantly improved interferon-γ but not IL-4 (data not shown) production of polarized naive CD4+ T cells, suggesting the development of a primary Th1 response. Th1-type phenotype was displayed in 47.8% of expanded T cells. As expected, significantly lower numbers of interferon-γ–producing CD4+ T cells could be detected when stimulation was performed with either OX40L mRNA–transfected immature DCs (27.6%) or with cytokine cocktail–matured DCs (29.2%). Cumulatively, these results suggest that OX40L mRNA transfection is capable of enhancing a Th1-biased CD4+ T-cell response.
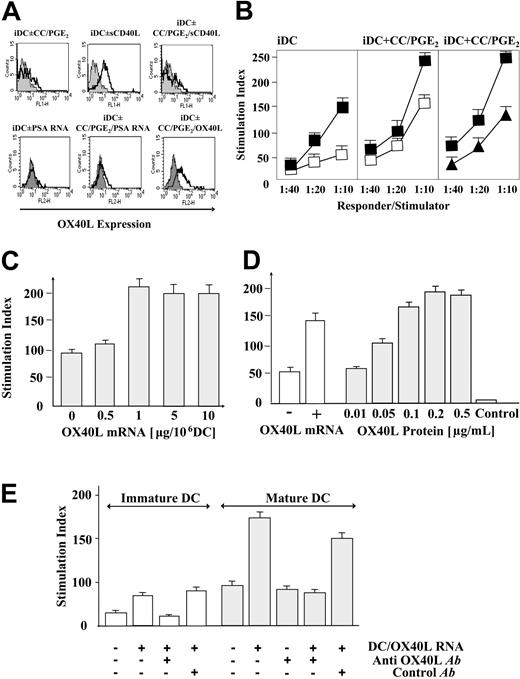
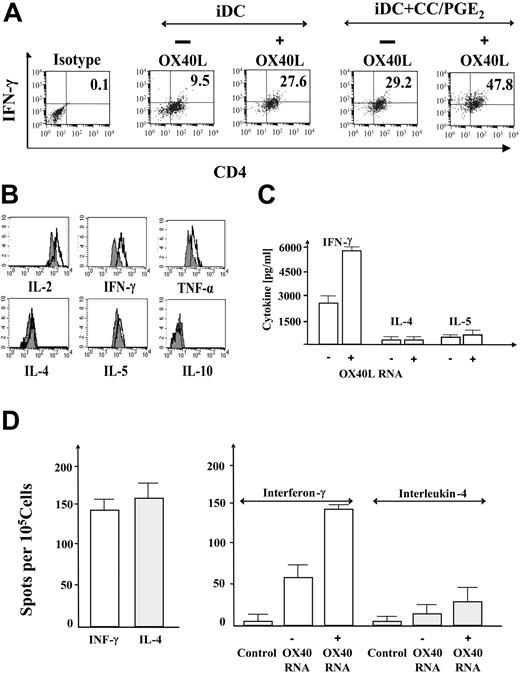
Secretion of Th1- and Th2-type cytokines by polarized CD4+cells. (A) Cytokine secretion assays. Control mRNA–transfected (–OX40L) or OX40L mRNA–transfected (+OX40L) immature or cytokine cocktail–matured DCs were used to polarize allogeneic CD4+CD45RA+ T cells at responder-to-stimulator ratios of 10: 1. After 5 days, T cells were stimulated and analyzed by cytokine secretion assay and double-stained with anti–interferon-γ–phycoerythrin (PE) and anti–CD4–fluorescein isothiocyanate (FITC) antibody. The percentage of CD4+/interferon-γ+ cells is indicated. (B) Cytometric bead arrays. CD4+CD45RA+ T cells were polarized with allogeneic control mRNA–transfected and cytokine cocktail–matured DCs (gray histograms) or allogeneic OX40L-transfected CC/PGE2-matured DCs (black overlays) and analyzed via cytometric bead array for secretion of Th1-type cytokines IL-2, IFN-γ, TNF-α (top row) or Th2-type cytokines IL-4, IL-5, IL-10 (bottom row) in cytometric bead arrays or by IFN-γ and IL-4 ELISA (C). (D, left panel) Frequency of tetanus toxoid (TTp30) peptide-specific Th1 (IFN-γ)– and Th2 (IL-4)–type CD4+ T-helper cells within the CD4+ population of a healthy donor were determined by interferon-γ ELISPOT analysis. (D, right panel) CD45RA+naive CD4+ T cells isolated from the same donor were stimulated with cytokine cocktail–matured, tetanus toxoid–pulsed DC with (+OX40L) or without (–OX40L) mRNA transfection. After 7 days, cells were restimulated with autologous DCs pulsed with the DR11.5-restricted helper epitope TTp30, and frequencies of TTp30 epitope–specific CD4+ T helper cells were determined by IFN-γ and IL-4 ELISPOT assays. Unpulsed, autologous DCs were used as control stimulators (control). Results are presented as mean number of spots with SD calculated from triplicate wells.
Secretion of Th1- and Th2-type cytokines by polarized CD4+cells. (A) Cytokine secretion assays. Control mRNA–transfected (–OX40L) or OX40L mRNA–transfected (+OX40L) immature or cytokine cocktail–matured DCs were used to polarize allogeneic CD4+CD45RA+ T cells at responder-to-stimulator ratios of 10: 1. After 5 days, T cells were stimulated and analyzed by cytokine secretion assay and double-stained with anti–interferon-γ–phycoerythrin (PE) and anti–CD4–fluorescein isothiocyanate (FITC) antibody. The percentage of CD4+/interferon-γ+ cells is indicated. (B) Cytometric bead arrays. CD4+CD45RA+ T cells were polarized with allogeneic control mRNA–transfected and cytokine cocktail–matured DCs (gray histograms) or allogeneic OX40L-transfected CC/PGE2-matured DCs (black overlays) and analyzed via cytometric bead array for secretion of Th1-type cytokines IL-2, IFN-γ, TNF-α (top row) or Th2-type cytokines IL-4, IL-5, IL-10 (bottom row) in cytometric bead arrays or by IFN-γ and IL-4 ELISA (C). (D, left panel) Frequency of tetanus toxoid (TTp30) peptide-specific Th1 (IFN-γ)– and Th2 (IL-4)–type CD4+ T-helper cells within the CD4+ population of a healthy donor were determined by interferon-γ ELISPOT analysis. (D, right panel) CD45RA+naive CD4+ T cells isolated from the same donor were stimulated with cytokine cocktail–matured, tetanus toxoid–pulsed DC with (+OX40L) or without (–OX40L) mRNA transfection. After 7 days, cells were restimulated with autologous DCs pulsed with the DR11.5-restricted helper epitope TTp30, and frequencies of TTp30 epitope–specific CD4+ T helper cells were determined by IFN-γ and IL-4 ELISPOT assays. Unpulsed, autologous DCs were used as control stimulators (control). Results are presented as mean number of spots with SD calculated from triplicate wells.
Although the flow cytometry–based assays shown in Figure 3A did not reveal a significant increase in numbers of IL-4–secreting T cells, their overall frequency was rather low (< 10%). Since the sensitivity of flow cytometry–based cytokine secretion assays may be suboptimal in determining minor changes in IL-4 secretion or to quantitate the numbers of cytokine-secreting T cells, we repeated the experiment shown in Figure 3A and analyzed cytokine secretion using cytometric bead array assays (Figure 3B), as well as by IL-4, IL-5, and interferon-γ ELISA (Figure 3C). We observed no significant increase in IL-4 or IL-5 secretion after transfection of DCs with OX40L mRNA, while interferon-γ secretion was significantly improved (2400 pg/1 × 106 cells to 5160 pg/1 × 106 cells) upon transfection with OX40L mRNA (Figure 3C). Similarly, the cytometric bead array assays shown in Figure 3B demonstrated increased secretion of Th1-type cytokines (IFN-γ, TNF-α, and IL-2), but not Th2-type cytokines, including IL-4, IL-5, and IL-10.
In conclusion, these results indicate that transfection of DCs with OX40L mRNA leads to enhanced numbers of Th1-polarized T cells, while only minor increases of Th2-type T cells were observed under the described experimental conditions.
Enhancement of MHC class II epitope-specific CD4+ T-helper cell responses
The experiments shown thus far demonstrate that transfection of DCs with OX40L mRNA is capable of enhancing the magnitude of a polyclonal, allogeneic Th1-type CD4+ T-cell response in an OX40L mRNA dose-dependent manner. Here, we investigated whether OX40L mRNA cotransfection was also capable of augmenting CD4+ epitope-specific T-cell responses in vitro. Because of the lack of well-defined tumor antigen-specific MHC class II epitopes, we used the model antigen tetanus toxoid (TT) in the experiments shown in Figure 4. We first isolated CD4+/CD45RA+ naive CD4+ T cells from a HLA-DR11.5–positive donor and stimulated these cells with TT-loaded, cytokine-matured DCs. After 7 days, cells were restimulated using autologous DCs that were pulsed with the HLA-DR11.5–restricted TT helper epitope TTp30. Frequencies of TTp30 epitope–specific CD4+ T-helper cells were determined in interferon-γ and IL-4 ELISPOT assays. To provide a reference for the Th1-skewing capacity of our DC vaccine, we determined the ratio of TTp30-specific Th1- and Th2-biased CD4+ T-helper cells within the CD4+ T-cell population isolated from a previously TT-vaccinated donor. As shown in Figure 3D (left panel), vaccination-induced exposure to TT leads to an equivalent induction of TT epitope–specific Th1 (IFN-γ) and Th2 (IL-4) CD4+ T-helper cells. In contrast, induction of TT-specific CD4+ T-helper cells from naive CD4+/CD45RA+ cells using cocktail-matured DCs lead to a modest bias of an epitope-specific TT response toward Th1, and OX40L mRNA transfection could further increase the frequencies of TT epitope–specific Th1-biased CD4+ T cells (Figure 3D, right panel).
Improved cytolytic function following stimulation with OX40L mRNA–cotransfected DCs. (A) Priming of PSA epitope–specific CTLs using PSA mRNA– or PSA-mRNA/OX40L mRNA–cotransfected DCs as stimulators. CTLs were generated using the indicated stimulators. After 7 days, CTLs were restimulated with PSA-HLA A0201 epitope VISNDVCAQV or control peptide HLSTAFARV, and interferon-γ release was determined by ELISA. (B) PBMCs from a healthy HLA-A0201–positive volunteer were stimulated twice with lymph node carcinoma of the prostate (LNCaP) RNA–transfected DCs (□) or with LNCaP/OX40L mRNA–cotransfected DCs (▪) to generate CTLs. These CTLs were then used in cytolytic assays using DC targets transfected with the following mRNAs: LNCaP RNA, PSA mRNA, GFP mRNA, and OX40L mRNA. Representative results from 3 healthy donors are shown. Results are presented as the mean value of cytokine secretion or target cell lysis with SD (error bars) calculated from triplicate wells.
Improved cytolytic function following stimulation with OX40L mRNA–cotransfected DCs. (A) Priming of PSA epitope–specific CTLs using PSA mRNA– or PSA-mRNA/OX40L mRNA–cotransfected DCs as stimulators. CTLs were generated using the indicated stimulators. After 7 days, CTLs were restimulated with PSA-HLA A0201 epitope VISNDVCAQV or control peptide HLSTAFARV, and interferon-γ release was determined by ELISA. (B) PBMCs from a healthy HLA-A0201–positive volunteer were stimulated twice with lymph node carcinoma of the prostate (LNCaP) RNA–transfected DCs (□) or with LNCaP/OX40L mRNA–cotransfected DCs (▪) to generate CTLs. These CTLs were then used in cytolytic assays using DC targets transfected with the following mRNAs: LNCaP RNA, PSA mRNA, GFP mRNA, and OX40L mRNA. Representative results from 3 healthy donors are shown. Results are presented as the mean value of cytokine secretion or target cell lysis with SD (error bars) calculated from triplicate wells.
OX40L mRNA–transfected DCs improve the generation of MHC class I–restricted CTL responses
We next performed experiments to investigate whether transfection of DCs with OX40L mRNA was also capable of improving antigen-specific CD8+ T-cell responses. PBMCs from a healthy HLA-A0201–positive volunteer were stimulated with autologous immature or cytokine cocktail–matured DCs transfected with PSA mRNA only, or using autologous DCs cotransfected with PSA and OX40L mRNA. After 7 days, cell cultures were restimulated with autologous DCs pulsed with the PSA peptide VISNDVCAQV or with an HLA-A0201–specific control peptide HLSTAFARV. Supernatants were harvested after 16 hours for the detection of interferon-γ secretion by ELISA. As shown in Figure 4A (right panel), the mature PSA mRNA– and OX40L mRNA–cotransfected DCs were superior (4-fold) in stimulating PSA peptide–specific, but not control peptide–specific CTL responses, than cytokine cocktail–matured, PSA mRNA–transfected DCs alone. As expected, cytokine cocktail–matured DCs (CC/PGE2) were generally more efficient than immature DCs in stimulating CTL responses against a single PSA epitope.
Next, we investigated whether OX40L mRNA–cotransfection was capable of enhancing CTL-mediated killing of tumor target cells in an antigen-specific fashion. PBMCs from a healthy HLA-A0201–positive volunteer were used to generate DCs. Immature DCs were transfected with total RNA (5 μg/106 DCs) extracted from the human prostate cancer cell line LNCaP (HLA-A0201+/PSA+) and used as stimulators to generate CTLs in vitro. A second set of CTLs was generated from LNCaP RNA–transfected DCs that were cotransfected with OX40L mRNA (2.5 μg/106 DCs). As targets, LNCaP RNA–, PSA mRNA–, GFP mRNA–(control), and OX40L mRNA–transfected (control) DCs were used in cytolytic assays. As shown in Figure 4B, the LNCaP-specific CTLs were not only capable of recognizing and lysing their cognate targets (LNCaP RNA–transfected DCs, left panel), but also PSA-expressing targets, albeit less efficiently, suggesting the presence of PSA-specific CTLs within the polyclonal LNCaP-specific T-cell response. Control targets in the form of GFP mRNA–transfected DCs were not lysed. Consistently, we observed improved lytic activity when OX40L RNA–cotransfected DCs were used as stimulators compared with LNCaP RNA–transfected DCs only. Interestingly, we did not observe significant killing of OX40L-expressing cellular targets by LNCaP-specific CTLs (generated by stimulation with OX40L mRNA–cotransfected DCs), suggesting that cross-reactivities against OX40L-expressing cells or generation of different autoreactive CTLs may not be a major issue in a vaccination setting.
OX40L-mediated enhancement of antitumor immunity
The studies shown thus far suggest that OX40L mRNA transfection is capable of enhancing the immunostimulatory properties of DCs in vitro. To provide evidence that this strategy could also translate into a therapeutic effect in murine systems, we performed a series of experiments in which mice carrying pre-established B16F10 tumors were immunized using OX40L mRNA–transfected DCs, cotransfected with mRNA encoding the self-antigen TRP-2.16 Mice were vaccinated twice at weekly intervals using DCs transfected with actin/OX40L mRNA (control), TRP-2 mRNA, or TRP-2/OX40L mRNA and monitored for the appearance of tumors.
As shown in Figure 5A, transfection with OX40L mRNA resulted in increased cell surface expression of OX40L on murine bone marrow–derived DCs and significantly enhanced the antitumor effect stimulated by TRP-2 mRNA–transfected DC vaccines (Figure 5B). Vaccination performed in this manner resulted in 40% tumor-free animals 30 days after tumor inoculation (P = 0.0197 relative to TRP-2 mRNA–vaccinated mice, and P = 0.001 relative to actin/OX40L mRNA–transfected mice).
To determine the effector cells involved in this TRP-2–specific T-cell response, we further analyzed the vaccine-induced CD4+ and CD8+ T-cell responses phenotypically and functionally. As shown in Figure 5C (upper panel, TRP-2 + OX40L), approximately 2% of the CD4+ T cells (0.52% of total cells) obtained from mice vaccinated with TRP-2/OX40L mRNA–cotransfected DCs up-regulated the activation marker CD69 upon restimulation, while only 0.12% of CD4+ T cells from mice vaccinated with TRP-2 mRNA–transfected DCs up-regulated CD69 (lower panel, TRP-2/OX40L). We have seen similar background levels of CD69 expression by CD4+ T cells obtained from nonvaccinated mice after restimulation with TRP-2 or actin mRNA–transfected DCs. Interestingly, we also observed a modest, but significant, increase (2-fold) in the numbers of CD4+/CD69+ cells when splenocytes of naive mice were restimulated with OX40L mRNA–transfected DCs (data not shown).
CD4+CD69+ cells expressed the Th1 cytokines IL-2 and IFN-γ, but not the Th2 cytokine IL-4, as evidenced by intracellular staining (Figure 5C, right panel). In contrast, no significant differences in CD69 expression or cytokine secretion were observed when splenocytes from TRP-2 mRNA–transfected DC-vaccinated mice were restimulated with TRP-2 mRNA– or actin mRNA–transfected DCs, suggesting that no TRP-2–specific CD4+ T cells had been stimulated in these animals (Figure 5C, left bottom panel). Additionally, intracellular cytokine staining did not reveal detectable levels of cytokine production by TRP-2–induced CD4+CD69+ T cells (Figure 5C, right bottom panel).
We next analyzed whether the OX40L-mediated enhancement of CD4+ T-cell immunity was capable of augmenting a CTL response, as suggested in the in vitro studies shown in Figure 4. Splenocytes were isolated from untreated mice and from animals vaccinated with TRP-2 mRNA–transfected or TRP-2/OX40L mRNA–cotransfected DCs, and TRP-2–specific killing was determined in cytolytic assays (Figure 5D). In contrast to the OX40L-mediated improvement in CD4+ T-cell immunity, there was only a modest, statistically insignificant improvement in CTL-mediated killing activity or cytokine secretion (data not shown) between CTLs isolated from mice vaccinated with TRP-2 mRNA– or with TRP-2/OX40L mRNA–cotransfected DCs. As shown in Figure 5D, CTLs generated from TRP-2/OX40L mRNA–vaccinated mice exhibited an only modest improvement in cytolytic activity against TRP-2 mRNA–transfected DC targets, when compared with CTLs generated from TRP-2 mRNA–vaccinated mice.
These data suggest that the OX40L-induced antitumor effect, allowing successful vaccination against the weak self-antigen TRP-2, was predominantly mediated by TRP-2–reactive CD4+ T cells, but not MHC class I–restricted CD8+ T cells. These findings are consistent with prior reports demonstrating that antigen-specific CD4+ T cells can eradicate tumors even in the absence of CD8+ T cells, or may represent the dominant effector arm in the antitumor response.17
Discussion
In this study, we demonstrate that transfection of cytokine cocktail–matured DCs with OX40L mRNA significantly potentiated antigen-specific CD4+ and CD8+ T-cell responses. Moreover, in vitro differentiation of naive CD4+ T cells was consistently skewed toward Th1. Our data also suggest that an improved CD4+ response can enhance a CTL response, as reported previously.6,18 Finally, vaccination of tumor-bearing mice using OX40L mRNA–transfected DCs resulted in significant enhancement of therapeutic antitumor activity as a result of in vivo priming of Th1-type CD4+ T-cell responses.
Although prior studies suggested that OX40 costimulation predominantly facilitates the stimulation of Th2 and, hence, B-cell responses,19 there is ample evidence that OX40 ligation has equally profound effects on Th1 immunity. It was previously shown that vaccination with antigen-loaded DCs resulted in the stimulation of strong cellular immunity in the absence of a detectable humoral immune response against the target antigen.20 Similarly, retroviral transduction of leukemia-derived DCs with OX40L resulted in the preferential stimulation of Th1-type immunity and augmented their antigen-presenting activity in vitro.21 Importantly, and of direct relevance to this study, triggering OX40 costimulation exhibited potent adjuvant antitumor effects in multiple tumor models, including models for sarcoma, breast carcinoma, glioma, melanoma, and colon cancer.22,23
Surprisingly, OX40L-driven stimulation of potent Th1 responses was observed despite PGE2-mediated IL-12p70 suppression. Although “downstream” events, such as up-regulation of 4-1BB ligand or DC-mediated expression of cytokines such as IL-2, IL-15, or IL-18, may have contributed to the IL-12p70–independent Th1 polarization, the blocking experiments shown in Figure 2 argue against this possibility.
We also show that transfection of monocyte-derived DCs with OX40L mRNA was capable of prolonging survival of mice carrying established B16/F10 melanomas. Consistent with other reports,24,25 our data suggest that tumor rejection was predominantly mediated by TRP-2–reactive and interferon-γ–producing CD4+ T cells and, to a lesser degree, by antigen-specific CTLs. While the mechanisms responsible for the observed antitumor effect are still being explored, possible effector mechanisms may include Fas/FasL-mediated killing,26 interferon-γ–mediated angiostasis,27 interferon-γ–mediated restoration of the antigen-presenting pathway,28 or the recruitment or activation of innate effectors, including macrophages and eosinophils.17,24
These data presented in this manuscript suggest that OX40L mRNA transfection represents a promising technology to enhance the DC-mediated stimulation of antigen-specific antitumor immunity and may be incorporated into active immunotherapy protocols to ultimately achieve T-cell responses with clinical effect. Transfection of cells with mRNA encoding biologic reagents such as cytokines or costimulatory molecules may represent a new approach for manipulating cells ex vivo for research and clinical applications, thereby eliminating the dependence on costly and often unavailable reagents from commercial sources.
Supported in part by the Morris Foundation and by the National Center for Research Resources, General Clinical Research Centers Program, National Institutes of Health (M01-RR-30).
Two of the authors (J.V. and E.G.) have declared a financial interest in a company (Argos Therapeutics) whose potential product was studied in the present work.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
Prepublished online as Blood First Edition Paper, December 23, 2004; DOI 10.1182/blood-2004-10-3944.