Abstract
AIMS Computerised Tomography (CT) scanning is the primary modality for assessment of therapeutic response in DLBCL. We evaluated whether functional imaging utilising FDG-PET may provide additional prognostic information in response assessment prior to completion of chemotherapy for patients with DLBCL.
METHODS We performed a retrospective, single-centre study of patients with DLBCL who received anthracycline-based chemotherapy +/− radiotherapy (RT) and had PET prior to completion of therapy.
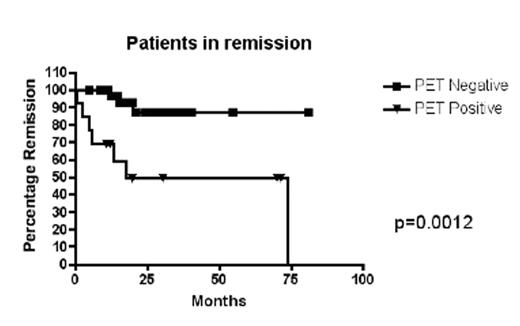
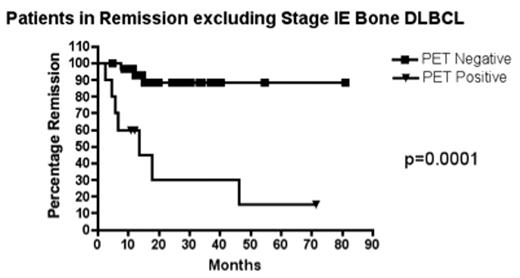
RESULTS From 1996–2004 there were 45 eligible patients. Median age was 59 years (range 26–82) with disease stage I–II (n=25) or III–IV (n=20). Median IPI was 2[IPI 0–2(n=27), IPI 3–4(n=13)] in 40 evaluable patients. Therapy included full-course CHOP/CHOP-like therapy (n=26); HyperCVAD (n=6) and limited (3–4 cycles) CHOP/CHOP-like chemotherapy with RT (n=13). Rituximab was used concurrently in 18 patients. Planned RT was administered in 23 patients. 13 (29%) patients were PET positive after a median of 3 chemotherapy cycles (range 1–5). Of these, 7 (54%) progressed a median of 7.2 months following completion of therapy. Of the 6 progression-free, 4 demonstrated residual low-grade activity at sites of prior bone involvement (median follow-up 50.8 months), while 2 patients (stage I and IV disease) had limited follow-up (<8 months). Of 32 patients who were PET-negative, only 3 have progressed (median 7.7 months follow-up); 2 with stage IV (IPI 1 and 2 respectively) and 1 with stage I disease. Overall the Positive predictive value (PPV) of a positive-interim PET was 58.3% [Hazard Ratio of 6.67 (95% C.I. 2.6 – 46.3)] and Negative PV(NPV) was 90.9% (see figure 1). Excluding patients with Stage IE bone lymphoma (see Figure 2), the PPV of positive-interim PET was 88%(77–98%) and NPV was 91%(82–100%). The median number of chemotherapy cycles after which PET was performed was equivalent according to interim PET status (3 cycles) as was median baseline IPI [IPI 2(PET-positive), IPI 1.5(PET-negative); p=0.17].
CONCLUSIONS Patients with DLBCL receiving chemotherapy who have persisting PET-positivity during their therapy have a greatly increased risk of treatment failure and should be considered for treatment intensification. Bone lymphoma may represent a distinct entity with a good prognosis despite some minor persisting PET-positivity prior to completion of therapy.
Patients in remission
Patients in Remission excluding Stage IE Bone DLBCL
Author notes
Corresponding author