Abstract
Background: Patients with immune thrombocytopenic purpura (ITP) infected with Helicobacter pylori (H. pylori) are often treated with antibiotics to eradicate infection and raise platelet counts. We aimed to systematically review the evidence regarding this practice to better quantify response rate.
Study Design and Methods: We searched MEDLINE through April 2005, without language restriction; reviewed reference lists and queried experts for articles describing treatment of ITP with antibiotics targeting H. pylori. We included studies of any design involving more than 5 patients. Response rates were tabulated using the authors’ definitions, and pooled using a random effects model. Techniques of meta-regression were used to assess whether patient or study characteristics influenced response rates.
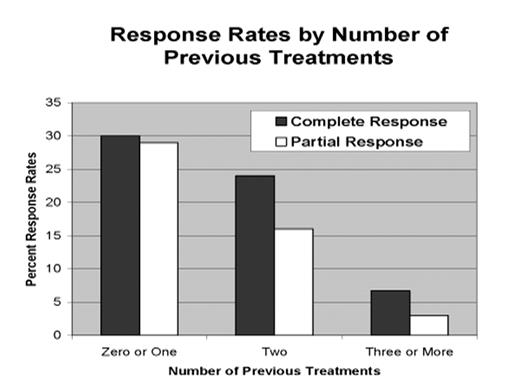
Results: We retrieved 52 potentially eligible studies. Of these, 16 studies met our inclusion criteria. From 10 studies, we had individual level patient data. None of the studies was a controlled trial. The pooled response rate (both partial and complete responses) was 45% [95% confidence interval (C.I.) 32% to 58%]. The number of previous treatments (0–1, 2, 3 or more) influenced the response rate with an 18% (p=0.001) decline in response rate with each higher category; duration of disease did not independently predict response. In analyses of individual patient data, quartile of platelet count upon entry also influenced response rate; 58% of patients in the highest quartile responded compared to 34% in the lowest quartile (p=0.018).
Conclusions: No randomized controlled trial has tested H. pylori eradication with antibiotics as a treatment for ITP. The sixteen observational studies we reviewed were fairly consistent with approximately half of treated patients having a platelet response to therapy. Without control groups, these studies do not provide strong evidence to support practice recommendations. However, given the low toxicity of antibiotic therapy, this treatment may be appropriate for patients who have not demonstrated refractoriness to multiple therapies.
Response Rates by Number of Previous Treatments
Author notes
Corresponding author