Abstract
It has been seen that a significant number of hemophiliacs show a co-existence of mutations related to an increased risk of thrombosis (Foka et al 2003). It has been also suggested that these thrombophilic genetic defects may actually protect hemophiliacs from recurrent bleeding episodes or may even lead to thrombosis in several cases (Makris et al 2003). Aim of the study was to investigate the coagulation activity and the existence of differences between hemophiliacs with and without thrombophilic mutations.
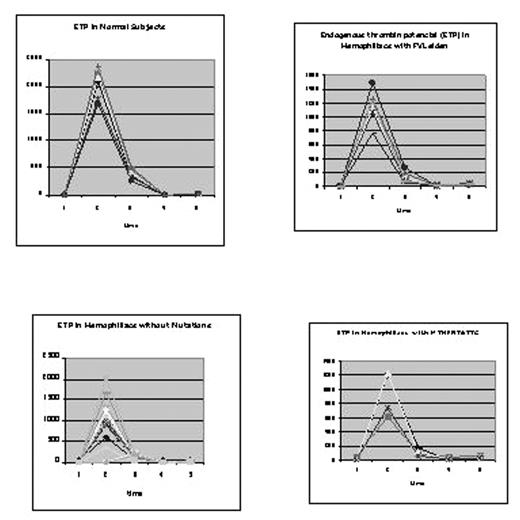
Materials and Methods: 65 subjects were studied (58 hemophiliacs 42±15 and 7 normal subjects 45±10 year old). We divided our subjects in 4 groups: 1- hemophiliacs without mutations (HN) 27 patients (pts), 2- hemophiliacs with FVLeiden and/or FIIG20210A mutations (HHet), 15 pts, 3- hemophiliacs with MTHFR mutation (homozygotes, HTT) 16 pts and 4-normal subjects (NS) 7.
Prothrombinase generation was evaluated by determination of F1+2 fragments of Prothrombin and the activation of coagulation by the determination of TAT levels (tested with Elisa). Simultaneously, we applied the Hicks and Pitney test to evaluate these results, and the Thrombin Generation test as a confirmatory standard test.
The Hicks and Pitney test was applied in an initial mixture of Cephaline and CaCl2 in equal and sufficient quantity of diluted PPP (1/10) incubated in 37°C. Initially, from this mixture, 0,1ml was transferred to a new tube containing 0,1ml substrate normal plasma and 0,1ml CaCl2. This procedure was repeated 10 consecutive times with 1 min interval. In parallel, 0,1ml from each incubation was frozen for measurement of F1+2 and TAT. Concerning the thrombin generation, we applied Endogenous Thrombin Potential (ETP) as described by Hemker et al (2000).
Our results are presented graphically with the picture. In these graphs it can be seen that hemophiliacs with no mutations show a gradual prothrombinase generation. On the contrary, HHet show a rapid generation that is also expressed by the concomitant increase in the levels of F1+2 and TAT. A similar response was observed in the group of normal subjects.
This observation can be explained as an adjustment mechanism of the coagulation defect, possibly able to prevent the high frequency and severity of bleeding episode in hemophiliacs with mutations. These results were more revelatory using the ETP test. The comparison between the different groups using the t-test distribution curve was as follow: a- Comparison between NS and HHet, p<0.1, in contrary the comparison between the NS curve and all the rest groups was statistically different (p<0,05).
Conclusion: The above results are in line with the observation that haemophilic patients bleed only after trauma etc. It seems probably that during the million years of human life on earth one or more compensatory mechanisms have developed. These appear to play a significant role in the rate of bleeding episodes in hemophiliacs and may also be able to explain the increasing frequency of thrombotic events in these patients.
Author notes
Corresponding author