Abstract
<Background> Invasive fungal infection is one of the most fatal complications after stem cell transplantation (SCT). EBMT group reported the risk factors of invasive fungal infections were delayed neutrophile engraftment and steroid use for acute graft versus host disease (GVHD) in cord blood transplantation with myeloablative regimens. However it has not been clear about invasive fungal infections after RICBT.
<Objective> The 1st purpose of this report was to investigate the incidence and pathogens of invasive fungal infections and the 2nd was to identify the risk factors for fungal infections after RICBT.
<Patients and Methods> We reviewed medical records of 103 patients with hematological diseases who had received RICBT between March 2002 and May 2005 at Toranomon Hospital, Tokyo, Japan. Median age was 57 years (17–79). Primary diseases were advanced (n=81) or standard (n=22). Median follow-up was 14 months (0.5–27). Conditioning regimen was fludarabine 125 mg/m2, melphalan 80 mg/m2 and TBI 4 Gy. GVHD prophylaxis was cyclosporine (n=67) or tacrolimus (n=43). Median total nucleated cells (TNC): 2.8 x 10^7 cells (1.7–5.2); Median CD34+: 0.78 x 10^5 cells (0.01–3.28); HLA match: 6/6 (n=2), 5/6 (n=16), 4/6 (n=88), 3/6 (n=1). Fluconazole 200mg/day was used as prophylaxis of fungal infections. Diagnosis of invasive fungal infection was made with the following EORTC/MSG criteria. The following factors were considered potential predictors of outcomes about 2nd purpose: patient’s age, infused TNC dose, disease status at transplantation, speed of netrophile engraftment, pre-engraftment reactions (PER) which we reported (
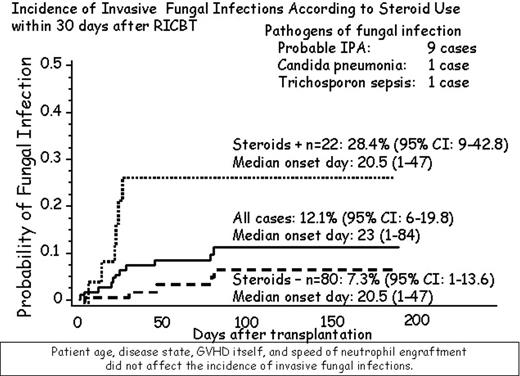
<Results> Neutrophile (>500/μL) and platelet recovery (>20,000/μL) were observed in 83% at day 60 (median; 22 day), 55% at day 100 (43day), respectively. Cumulative incidence of acute GVHD (II-IV) was 33%. OS were 39% (95% CI: 29–50) in all cases, 67% (95% CI: 47–87) in standard, and 32% (95% CI: 20–43) in advanced (p<0.05), respectively. Incidence of invasive fungal infections was 12% (95% CI: 6–20) and median onset day was 23 days (1–84) after RICBT. Pathogens of invasive fungal infections comprised 9 cases of probable invasive pulmonary aspergillosis, and one case each of Candida pneumonia and Trichosporon sepsis. Incidence of invasive fungal infections in patients with PER+/steroids + (n=22) was 28% (95% CI: 9–43), in patients without PER (n=80) was 7% (95% CI: 1–14). In multivariate analysis, the most important risk factor of invasive fungal infections was steroid use for PER (p<0.05), while other factors did not influence.
<Discussion/Conclusion> In our experience with reduced intensity cord blood transplantation, the only risk factor for invasive fungal infections was steroid use for PER within 30 days. Invasive fungal infections, especially invasive aspergillosis, remain an important complication after allogeneic stem cell transplantation, regardless of the type of conditioning regimens and the sources of stem cells.
Author notes
Corresponding author