Abstract
Background: Acute ATL is an aggressive hematologic malignacy with a median survival of 9 months. It is a malignant disease of mature activated T-cells caused by human T-cell lymphotropic virus (HTLV-I). Chemotherapy is disappointing for ATL, particulary for acute ATL. Antiretroviral therapy with combination interferon/zivodudine increases responses and improves survival. However, the disease is characterized by repeated relapses with few novel therapeutic options available for patients. Allogeneic stem cell transplant is the only known cure for ATL. We present a case report of refractory acute ATL and relapsed leukemic meningitis with marked clinical response and hematologic remission to single-agent denileukin diftitox.
Method: The patient (pt) is a 55 year-old black man (from Mississippi) who presented Janurary 2004 with mild fatigue, lymphocytosis and was found to be in chronic-phase ATL. Peripheral blood (PB) flow cytometry showed a 72% clonal T-cell population: CD3+, CD7−, CD5+, CD2+, CD4+, and CD25+. Serology was + for HTLV-1 and T-cell genes were rearranged.
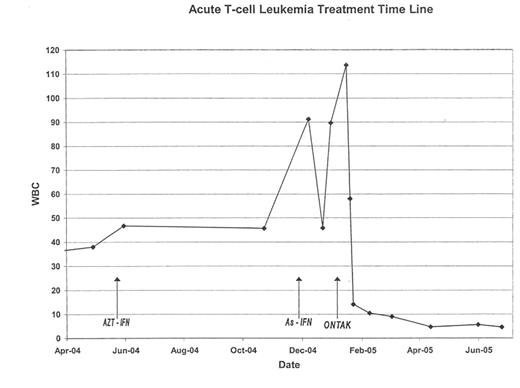
Results: The pt was initially observed without therapy. Within 6 months, he developed profound fagtigue, weight loss, severe headaches, eye pain, tinnitus and myalgias. White blood count (WBC) increased and acute ATL and leukemic meningitis was diagnosed. The pt began daily zidovudine/α interferon (1 gram and 9 million units, respectively) and intrathecal (IT) methotrexate. Cerebral spinal fluid (CSF) cleared with slight decrease in WBC, and improvement in symptoms. He relapsed 5 months later with reccurrence of constitutional and CNS symptoms. Repeated ommaya catheter CSF analysis at that time was negative, however, a lumbar puncture was floridly positive. The pt subsequently began daily aresenic trioxide and weekly pegylated interferon therapy. There was a transient decline in symtoms and WBC with clearing of the CSF, although the patient quickly relapsed with massive PB and CSF infiltration of ATL cells (PB absolute lymphocyte count 89.3 cc3/mm3) and severe constitutional symtpoms including 20 pound weight loss.
Acute T-cell Leukemia Treatment Time Line
At this relapse, the pts CSF T-cells were 87% CD25-positive. Denileukin diftitox was started at 18 μg/kg/day IV(days 1–5) every 21 days with concurrent IT cytarabine. The only other concomitant medications were diflucan and gabapentin (no steroids given at any time). The pt had rapid resolution of all symptoms and normalization of the WBC following his 1st cycle. The pt has tolerated 8 denileukin diftitox cycles well. PB flow cytometry now shows 1% CD25 T-cell positivity. The pt is currently asymptomatic and proceeding to 6/6 matched sibling allogeneic transplant.
Conclusion: This case demonstrates a marked and sustained response to single-agent denilekin difitox. There is 1 published case of ATL treated with denileukin diftitox. However, that pt was also treated with hyper-CVAD chemotherapy. Despite the anecdotal nature of this case, we believe it is important to report this information, especially in a disease with often few therapeutic options.
Author notes
Corresponding author