Abstract
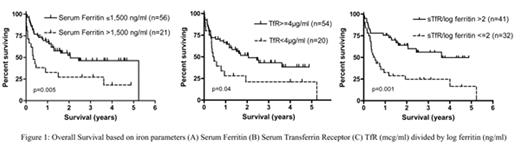
Transfusional iron overload is common in survivors of acute leukemia and hematopoietic stem cell transplantation and might cause long-term liver dysfunction. Routine evaluation for iron overload in such patients is recommended because excess iron can be readily removed from the body via phlebotomy or chelation. Iron overload might be associated with worse survival after stem cell transplantation in these diseases. We were interested in determining whether levels of the iron binding protein ferritin or the serum transferrin receptor (TfR) were predictive for survival. In a prospective study, we examined the correlation between iron parameters at the time of transplantation and overall survival. Serum ferritin, transferrin saturation, and TfR were measured before preparative regimen on patients who underwent hematopoietic stem cell transplantation between 1999 and 2004 for the diagnosis of aplastic anemia, MDS or acute leukemia (n=79). We used the number of transfusions before transplantation as a measure of iron load. Among these iron markers, serum ferritin correlated the most with the number of transfusions, regardless of remission status. High ferritin (>1,500 ng/ml), low TfR (≤4 μg/ml) and low TfR/log ferritin ratio (≤2) were associated with shorter survival (p=0.005, 0.04, and 0.001 respectively)(Figure 1). Among acute leukemia patients in remission, there was no difference in overall survival between patients with high or low iron markers. Markers of iron excess (serum ferritin >1,500 ng/ml, TfR/log ferritin ratio ≤2) at the time of stem cell transplantation is associated with shorter survival in MDS, aplastic anemia and acute leukemia with active disease. These results demonstrate that knowledge of patient ferritin and TfR levels can aid in risk stratification. The results also suggest that patients with high levels of ferritin may benefit from iron chelation before treatment.
Overall Survival based on iron parameters (A) Serum Ferritin (B) Serum Transferrin Receptor (C) TfR (mcg/ml) divided by log ferritin (ng/ml)
Overall Survival based on iron parameters (A) Serum Ferritin (B) Serum Transferrin Receptor (C) TfR (mcg/ml) divided by log ferritin (ng/ml)
Author notes
Corresponding author