Abstract
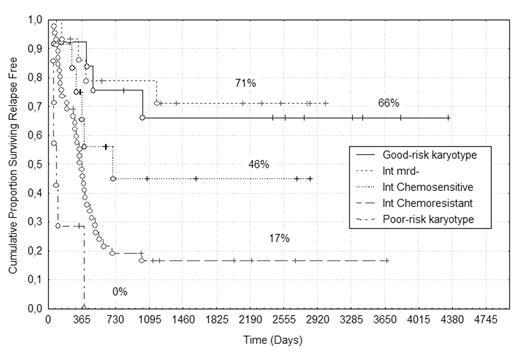
According to the prognostic classifications of karyotypic abnormalities of AML (MRC and SWOG), the intermediate group includes patients either lacking good and poor karyotype or with normal karyotype. Therefore, it represents, by definition, a miscellaneous group for which the evaluation of the better treatment strategy is difficult due to its heterogeneity. Moreover, patients belonging to this intermediate group account for the large majority of AML cases enrolled into clinical trials. The aim of our study was to analyze the factors specifically affecting the outcome of patients bearing intermediate risk karyotypic abnormalities in a group of 94 AML cases entered into the EORTC/GIMEMA protocols AML10/AML12 (age <61yrs) or AML13/AML15 (age >61 yrs), consisting in intensive induction and consolidation cycles. The clinico-biological variables evaluated in our model included age, FAB, WBC count, MDR1 phenotype, FLT3 mutations and level of post-consolidation bone marrow residual leukemic cells (BMRCL) assessed by multiparametric flow-cytometry (MPFC). In our experience, patients with <2.0 x10−4 BMRLC at the end of consolidation therapy were considered MRDneg and showed a better outcome, patients whose level of MRD were >2.0x10−4 at the end of consolidation were considered MRDpos and showed a poor prognosis. However, the category of MRDpos patients could be divided into 2 subgroups depending on whether they had a reduction of BMRLC between induction and consolidation, even not reaching the threshold of MRD negativity. In fact, we identified patients whose BMRLC were reduced by at least 1-log between induction and consolidation, referred to as “chemosensitive MRDpos” with an intermediate prognosis, and those showing no reduction of MRD levels between induction and consolidation, referred to as “chemoresistant MRDpos” with the worst outcome. Using the MRC classification, 14/94 patients (15%) had a good-risk cytogenetics, 74/94 (79%) an intermediate-risk and 6/94 (6%) a poor-risk. When we restricted the analysis to cases with intermediate-risk karyotype we found that: 1) in multivariate model, MRD status after consolidation was the only variable significantly affecting relapse free survival (RFS)(P=0.001); 2) patients in the MRDneg, “chemosensitive MRDpos” and “chemoresistant MRDpos” group differed significantly in terms of relapse rate (25% vs. 50% vs. 78%, respectively, P<0.001); 3) the 5 years median duration of RFS was 71%, 46% and 16%, respectively (P<0.001); 4) MRDneg patients had an outcome slightly better than those bearing good risk karyotype; 5) “chemoresistant MRDpos” patients showed a dismal outcome comparable to poor-risk cytogenetic patients; 6) “chemosensitive MRDpos” patients showed a true intermediate behavior (Fig. 1). These results suggest that the inclusion of MPFC assessment of MRD in patients with intermediate risk karyotype may be particularly useful in discriminating subgroups with different outcomes, allowing to design risk-based therapeutic programs in a very heterogeneous group of AML.
Author notes
Corresponding author