Abstract
At present, a large number of clinical trails make use of inhibitors that target leukemia specific defects, such as BCR-ABL, c-kit mutations or tandem duplications in the FLT3 gene (FLT3-ITD). Irrespective of their target, these studies all share the need for a short term read out parameter. Nowadays remission rate, remission duration and survival are used as a final read out in such studies. Previously we have observed that after different cycles of chemotherapy the frequencies of Minimal Residual Disease (MRD) cells, as determined using aberrant immunophenotypes, is highly correlated with clinical outcome (
Feller, Leukemia 2004; 18:1380
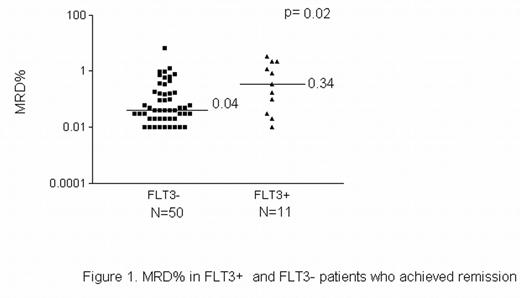
). Based on these observations we have examined whether MRD might function as the desired short term read out. As a proof of principle we have examined this for FLT3-ITD. We determined ITD status in bone marrow (BM) samples of 162 newly diagnosed AML patients by gel electrophoresis and GeneScan analysis. Frequencies of MRD cells were assessed in 316 BM samples of these 162 patients: 146 after 1st, 95 after 2nd and 75 after 3rd cycle of chemotherapy using LAP technology. As also shown by others, FLT3-ITD at diagnosis was predictive for OS (p=0.04, B (exp)=1.80 and RFS (p=0.05, B (exp)=1.91). This study now shows in addition, that in remission patients after 1st cycle (70% of all patients), the presence of an ITD (21% of the cases) at diagnosis is associated with 8.5-fold higher MRD% (median 0.34%, range 0.01-3.3%), compared to wild type FLT3 (median 0.04%, range 0.01–1.27%), p=0.020. Similar to our previous observations, MRD level taken as a continuous variable in the total patient group after 1st cycle was inversely correlated to OS (p=0.041) and RFS (p=0.0001). Using previously described clinically relevant MRD cut-offs, such 8.5-fold differences in frequencies of MRD cells resulted in significant differences in OS and RFS, in the whole range of MRD frequencies (0.01-6.8%). Based on this we conclude that efficacy of FLT3 inhibitors in terms of survival can be predicted with MRD frequency after 1st cycle of therapy that includes the inhibitor. MRD frequency may thus serve as an early read out parameter, for efficacy of targeted therapy in AML.Author notes
Corresponding author
2005, The American Society of Hematology
2005