Abstract
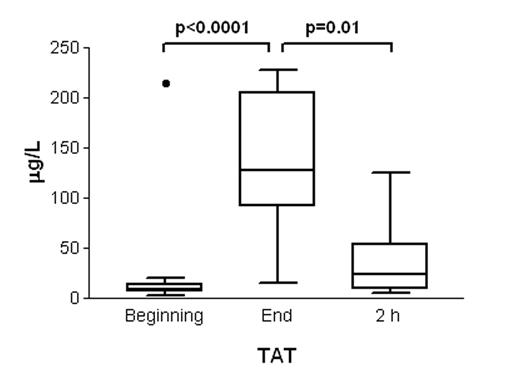
Exchange transfusion (ET) is a standard procedure in newborn infants with severe hyperbilirubinemia. Although infant’s whole blood volume is exchanged with adult blood containing different amounts of coagulation factors and anticoagulants, the effects of ET on newborn blood coagulation system remain virtually unstudied. We now prospectively evaluated the effect of ET on thrombin formation and on coagulation profile in newborns. ET was performed by composite blood (200mL/kg). After parental consent the blood samples were collected from the infused blood and from the arterial line of newborns (n=16) at the beginning (pre-ET), at the end (post-ET), and two hours after completing ET. The samples were assayed for platelet count, thrombin-antithrombin complexes (TAT), prothrombin fragment F1+2, FV, FVII, FVIII, antithrombin, protein C, protein S, von Willebrandt factor (vWf) multimers, and for tissue factor-initiated thrombin formation (endogenous thrombin potential - ETP, thrombin peak) with or without added activated protein C (APC). Venous blood from 9 healthy adults and cord blood from 8 deliveries of healthy women were used as controls. TAT increased significantly during ET and returned to pre-ET levels two hours after the ET (Figure). F1+2 changed similarly with TAT. Platelet count was significantly reduced during ET (Pre-ET 272±23 109/L vs. Post-ET 45±4 109/L; mean±SEM; p=0.0005). The measured coagulation factors and anticoagulants increased significantly (p<0.05), except FV. At the end of ET the newborn plasma levels of FV, FVII, antithrombin, and protein S were similar with the respective levels in the infused blood, whereas protein C levels remained lower (p<0.001) and FVIII higher (p<0.001) than in the infused blood. The functional high-molecular weight forms of vWf multimers in newborn plasma were reduced during ET, thus changing the multimer distribution to an adult-like pattern. The pre-ET thrombin peak level and ETP were similar with cord control group but only ~60% of adult levels. ETP increased in the newborn plasma during ET reaching adult levels. APC decreased ETP in newborn plasma similarly at the beginning (31±5%) and at the end (35±4%) of ET. This thrombin reduction by APC was similar with cord control group but significantly less (p<0.0001) than the decrease achieved by APC in adults (79±4%); thus the resistance to APC, characteristic to newborn plasma, remained the same throughout ET. In conclusion, ET causes profound temporary thrombin escalation despite the procedure-associated thrombocytopenia. Multiple procoagulant changes in post-ET plasma could be demonstrated partially explaining the enhanced thrombin formation. ET-induced coagulopathy may be clinically significant in sick newborns already prone to bleeding and thrombotic complications.
The evolution of TAT around exchange transfusion in newborn infants (median, 25th and 75th percentile, minimun and maximum; n = 16; • = outlier). Wilcoxon test was used for comparisons.
The evolution of TAT around exchange transfusion in newborn infants (median, 25th and 75th percentile, minimun and maximum; n = 16; • = outlier). Wilcoxon test was used for comparisons.
Author notes
Corresponding author