Although unrelated hematopoietic cell transplantation (HCT) is curative for many hematologic malignancies, complications and relapse remain challenging obstacles. Natural killer (NK) cells, which recover quickly after transplantation, produce cytokines and express killer immunoglobulin-like receptors (KIRs) that regulate their cytotoxicity. Some clinical trials based on a KIR ligand mismatch strategy are associated with less relapse and increased survival, but results are mixed. We hypothesized that T cells in the graft may affect NK cell function and KIR expression after unrelated transplantation and that these differences correlate with clinical outcomes. NK cell function was evaluated using 77 paired samples from the National Marrow Donor Program Research Repository. Recipient NK cells at 100 days after both unmanipulated bone marrow (UBM) and T-cell depleted (TCD) transplants were compared with NK cells from their healthy donors. NK cells expressed fewer KIRs and produced more interferon γ (IFN-γ) after UBM compared to TCD transplants. Multivariate models showed that increased NK cell IFN-γ production correlated with more acute graft-versus-host disease (GVHD), and decreased KIR expression correlated with inferior survival. These results support the notion that T cells in the graft affect NK cell reconstitution in vivo. Understanding these mechanisms may result in strategies to improve clinical outcomes from unrelated HCT.
Introduction
Natural killer (NK) cells, first recognized for their ability to kill virally infected or tumor cells without prestimulation, are regulated by a net balance of activating or inhibitory signals to determine whether a target is killed.1,2 Although NK cell killing does not require class I major histocompatibility complex (MHC) for target recognition, ligation of class I through killer immunoglobulin-like receptors (KIRs) can engage an overriding inhibitory signal and prevent target lysis.3 As explained by Ljunggren and Karre in the “missing self” hypothesis, it is the class I down-regulation by transformation or infection that renders targets susceptible to NK lysis.4
The NK receptors that bind to class I MHC proteins were first identified in the mouse (Ly49 family of C-type lectin-related proteins), and later in humans as type I membrane glycoproteins of the immunoglobulin superfamily on chromosome 19.5-10 The KIRs are either activating or inhibitory, and the class I ligands of several inhibitory KIRs have been identified (KIR2DL2/L3 and group 1 HLA-C allotype, KIR2DL1 and group 2 HLA-C allotype, and KIR3DL1 and Bw4).7 The regulation of KIR expression is poorly understood, but it is believed that each NK cell must have at least one self-specific inhibitory receptor to suppress autoreactive NK cells. NK cells also express a related family of activating and inhibitory lectin-type receptors encoded on chromosome 12 (NKG2), which form dimers with CD94 and recognize nonclassic class Ib HLA-E and HLA-G molecules.11-14 CD56+bright cells, the major producers of interferon γ (IFN-γ),15 express high levels of CD94/NKG2 but almost no KIRs and are thought to be more primitive than CD56+dim cells.16 Still, the continuum of differentiation from a stem cell to a lineage-committed NK cell remains unclear. In vitro, NK cell receptor acquisition occurs after NK cell commitment and CD94/NKG2 expression precedes KIR expression.17
It has been hypothesized that allogeneic transplants selected for lack of donor KIRs matched to recipient MHC (ie, KIR ligand) allow the development of alloreactive donor-derived NK cells that could kill host tumor (graft versus leukemia [GvL]) and eliminate the host dendritic cells that present alloantigen and initiate graft-versus-host disease (GVHD).18 Several recent trials using KIR-ligand mismatch to exploit NK cell alloreactivity in the setting of haploidentical or unrelated allogeneic hematopoietic cell transplantation (HCT) have yielded discrepant results.19 In 2002, Ruggeri et al were the first to demonstrate increased overall survival, reduced GVHD, and improved engraftment when using KIR-ligand mismatched haploidentical, T-cell depleted (TCD) transplants for myeloid but not lymphoid malignancies.20 In a later trial that used less T-cell depletion, the KIR-mismatch patients developed more acute GVHD and had poorer survival.21 In the unrelated setting the results have also been mixed. A similar KIR-ligand mismatch strategy failed to provide a clinical benefit in myeloid malignancies when using unmanipulated T-cell replete unrelated donor graft.22 In a pediatric population, the use of minimally T-depleted HLA-nonidentical, KIR-ligand mismatched transplants did not improve clinical outcomes, and, in fact, alloreactive donor T cells were associated with an increased risk of acute GVHD, chronic GVHD, and death.23 The addition of in vivo T-cell depletion with anti-thymocyte globulin resulted in an overall survival advantage for patients with acute myeloid leukemia (AML) in one study,24 but was associated with increased relapse and no improvement in survival in a second study,25 and with decreased survival mainly due to increased infection rate in a third.26 We hypothesize that the variation in clinical results may be explained in part by the role of T cells on developing NK cells. In this study, we focused on the effect of T cells in the graft, their effect on NK cell reconstitution, and their correlation with clinical outcomes.
Patients, materials, and methods
Patients and samples
Analyses were performed using peripheral blood mononuclear cells (PBMCs) from 77 unrelated donor and recipient pairs; cells were collected and frozen by the National Marrow Donor Program (NMDP) Research Repository between 1990 and 1999. The donor samples were drawn before transplantation, and the recipient samples at a median day of +98 (92% of samples were drawn between days +70 and +130). All patients were undergoing transplantation for chronic myeloid leukemia (CML) and received either unmanipulated bone marrow (UBM, n = 37) or marrow processed with T-cell depletion (n = 40). Seventy-nine percent of donor and 90% of recipient samples were cryopreserved within 24 hours of collection. Data on patient characteristics and transplantation outcomes were provided by the NMDP. Samples and clinical data were obtained after informed consent and approval from the NMDP and University of Minnesota Institutional Review Boards according to the Declaration of Helsinki.
Flow cytometry
Immunophenotypic analysis of cryopreserved PBMCs was performed using 4-color analysis on a FACSCalibur (Becton Dickinson, San Jose, CA) with CELLQuest Pro software (Becton Dickinson). Thawed cells were stained with the following monoclonal antibodies (mAbs): fluorescein isothiocyanate (FITC)-conjugated DX9 (anti-CD158e), EB6 (anti-CD158a/h), GL183 (anti-CD158b/j), FES 173 (anti-CD158i), HP-3D9 (anti-CD94), peridinin chlorophyll A protein (PerCP)-conjugated SK7 (anti-CD3), and allophycocyanin (APC)-conjugated NCAM16.2 (anti-CD56), all from Becton Dickinson. Phycoerythrin (PE)-conjugated Z199 (anti-NKG2A) (Immunotech, Brea, CA) was used as indicated.
IFN-γ production detected by intracellular flow cytometry
Donor and recipient PBMCs (1 × 106) were thawed and incubated for 24 hours in RPMI with 10% fetal calf serum, 100 U/mL penicillin, 100 U/mL streptomycin, and 1% glutamine with interleukin 12 (IL-12; 10 ng/mL) and IL-18 (100 ng/mL) to stimulate maximal IFN-γ production27 or in media alone as a control. For the last 5 hours of incubation the cells were treated with brefeldin A at 0.4 mg/mL to trap the protein in the cytoplasm. The cells were surface stained with anti-CD3 and anti-CD56 as described, and then permeabilized with Fix/Perm Buffer/FACS Lyse (Becton Dickinson) with the addition of 250 μL polyoxyethylene-sorbitan monolaurate (Tween 20; Sigma, St Louis, MO). The intracellular IFN-γ was stained with PE-conjugated anti-human IFN-γ (clone 25723.11; Becton Dickinson).
Statistical analysis
Nonparametric Wilcoxon tests were used to compare the distributions of protein expression levels. To test the differences in levels between donor and recipient pairs, a Wilcoxon signed rank test was used. A Wilcoxon rank sum test compared the differences in expression levels between UBM and TCD transplants. A Fisher exact test was used to test for differences in group proportions. Linear regression analysis was performed to examine the association between 2 continuous measures of protein expression. Finally, a time-to-event analysis for survival and acute GVHD outcomes was performed. The analysis used a multivariate Cox proportional hazards model stratifying the associations on transplant type.28 For models where GVHD is the outcome of interest, the competing risk of survival was accounted for in the Cox models and cumulative incidence curves using the methods of Fine and Gray.29
Results
Recipients have increased NK cells after unrelated transplantation
NK cells that develop from stem cells in vitro predict that immature NK cells express few KIRs soon after lineage commitment.17 Unrelated HCT was used as a model to study the effect of T-cell depletion on NK cell reconstitution in vivo. Donor and donor-derived recipient blood samples, both generated from the same stem cell source, were obtained from the NMDP Research Repository to study the effect of transplantation variables on NK cell receptor development. Patient characteristics and clinical outcome data were collected by the NMDP. The mean follow up was 4.1 years. Outcomes included survival, relapse, incidences and grades of acute and chronic GVHD, infections, and cause of death. Comparisons of patient characteristics, relapse, and survival were similar for 37 patients receiving UBM and 40 receiving TCD grafts as shown in Table 1. As expected, there was significantly less grade II to IV acute (P < .001) and chronic (P = .007) GVHD in recipients of TCD transplants and TCD graft recipients were more likely to be HLA mismatched (P = .01).
Flow cytometry was used to measure lymphocyte subsets in the reconstituted donor-derived cells in recipients at day +100, which were compared to their healthy donor baselines (Table 2). For all lymphocyte subsets there were no significant differences between the donors of UBM or TCD transplants. The percentage of CD56+/CD3- NK cells was increased approximately 4-fold in all recipients (9.8% ± 0.7% versus 40.2% ± 2.6%; P < .001) with no significant difference between recipients of UBM or TCD transplants (P = .26). The percentage of T cells was significantly decreased after both transplant types, more so after TCD transplants (UBM versus TCD graft recipients, P = .003). There were no significant differences in the percentages of CD56+/CD3+ NK/T cells between recipients and donors for either transplant type.
KIR expression is diminished after unrelated transplantation
KIR recovery was evaluated on reconstituted donor-derived NK cells with a cocktail of 4 mAbs that bind multiple KIRs (Figure 1). Compared to their donors, KIR expression by CD56+/CD3- NK cells was significantly decreased after unrelated UBM and TCD transplantation (donor, 50.6% ± 2.1% versus recipient, 35.2% ± 2.2%, n = 74; P < .001). KIR expression was lower after UBM (donor, 48.4% ± 2.4% versus recipient, 26.7% ± 1.9%, n = 36; P < .001) than after TCD transplantation (donor, 53.3% ± 3.3% versus recipient, 42.7% ± 3.3%, n = 38; P = .017), and the difference in KIR expression between the recipient groups was highly significant (P = .001). There was no difference in KIR expression between the UBM or TCD transplant donors.
To further understand the effect of transplantation on KIR recovery, immunophenotyping was performed using individual mAbs that bind KIRs known to recognize HLA class I ligands (Figure 2). Interestingly, after UBM transplantation the expression of KIR recognizing the HLA-C ligands was more diminished than was the expression of KIR3DL1, which binds HLA Bw4. Expressions of KIR2DL1/S1 and KIR2DL2/L3/S2 were both decreased approximately 50% (P < .001), whereas KIR3DL1 was decreased approximately 25% (P = .04).
NKG2A expression is inversely correlated with KIR expression after unrelated transplantation
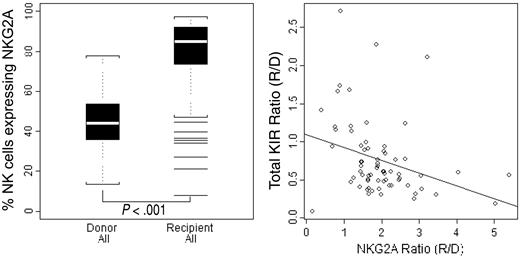
In human and mouse ontogeny, CD94/NKG2A is expressed before KIR and Ly49 receptors, respectively.17,30,31 These lectin receptors were evaluated after unrelated transplantation. In marked contrast to KIRs, both were significantly increased in recipients at day +100 compared to their donors (P < .001), with no significant difference between UBM and TCD transplants (Figure 3 left; data not shown for CD94). To evaluate the relationship between NKG2A recovery and KIR recovery, the ratios of the percent expression on recipient NK cells over that on donor NK cells (R/D) were compared (Figure 3 right). A KIR R/D ratio of 1.0 corresponds to a measured KIR expression that is 100% of the donor baseline level, whereas a ratio of 0.6 corresponds to a 60% recovery of KIR on the reconstituted donor-derived cells within the recipient. Linear regression analysis showed a significant inverse relationship between KIR R/D and NKG2A expression (β = -0.17, P = .01), which corresponds to a decrease in the KIR ratio of 0.17 for every fold increase in the NKG2A ratio.
IFN-γ-producing NK cells are increased after UBM transplantation
To understand the function of day +100 reconstituted NK cells, the production of IFN-γ was measured by flow cytometry after a 24-hour stimulation with IL-12 and IL-18 and was compared with that of their healthy donors (Figure 4). Compared to their donors, the recipients of UBM transplants showed a significant increase in the percentage of NK cells producing IFN-γ (donor, 39.6% ± 3.8% versus recipient, 54.0% ± 4.5%; P = .03), but IFN-γ production was not increased in recipients of TCD transplants (donor, 31.7% ± 3.0% versus recipient, 34.9% ± 5.8%; P = .55). There was no significant difference between donor groups. In contrast, the amount of IFN-γ production by recipient NK cells was significantly different based on whether they received an UBM or TCD transplant graft (P = .007).
Recipients of UBM transplants exhibit lower KIR expression compared to their donors than recipients of TCD transplants. Donor or day +100, donor-derived recipient PBMCs were stained with a cocktail of directly conjugated mAbs to KIR (DX9, EB6, GL183, and FES173, which stain CD158e, CD158a, CD158b, and CD158i, respectively). The means, 25th to 75th percentile ranges, and extreme values of the percentages of CD56+/CD3- cells expressing KIR by flow cytometry are shown in the box plot. Results are presented for donors or recipients separated by graft type (UBM or TCD) or combined (ALL). P = not significant (NS) between any donor groups.
Recipients of UBM transplants exhibit lower KIR expression compared to their donors than recipients of TCD transplants. Donor or day +100, donor-derived recipient PBMCs were stained with a cocktail of directly conjugated mAbs to KIR (DX9, EB6, GL183, and FES173, which stain CD158e, CD158a, CD158b, and CD158i, respectively). The means, 25th to 75th percentile ranges, and extreme values of the percentages of CD56+/CD3- cells expressing KIR by flow cytometry are shown in the box plot. Results are presented for donors or recipients separated by graft type (UBM or TCD) or combined (ALL). P = not significant (NS) between any donor groups.
Incidence of acute GVHD correlates with increased IFN-γ production by NK cells
NK cells reconstituting after unrelated transplantation differed in their display of KIR, which corresponded to functional changes identified in vitro, but the physiologic importance of these findings was still unknown. A multivariate Cox proportional hazards model was used to evaluate the relationship between KIR recovery and NK cell function on clinical outcomes after unrelated transplantation. The input variables included the KIR expression ratio (R/D), IFN-γ production by the donor-derived NK cells, transplant type (UBM or TCD), and the percentage of CD56+bright cells. Patient characteristics including race, Karnofsky performance status, and age were also analyzed and had no significant effect on the outcome. The only independent variable affecting the incidence of acute GVHD was the percentage of NK cells expressing IFN-γ. In a model stratified for graft type, each 1% increase in the percentage of NK cells expressing IFN-γ was associated with a relative risk of 1.03 (P < .001). Thus, an increase of 10% in IFN-γ production, a clinically relevant change, is associated with a relative risk of 1.28, or a 28% increase in risk for acute GVHD. Cumulative incidence curves are shown with IFN-γ production stratified to equal to or more than 50% or less than 50% of NK cells, which was approximately the median percentage of NK cells producing IFN-γ for all samples (Figure 5). The relative risk of acute GVHD for IFN-γ production by 50% or more of NK cells was 4.6 (P < .001). When stratified by T-cell depletion status, which did not exert an independent effect, the same calculation yielded a relative risk of 3.7 (P < .001). We also evaluated chronic GVHD as an end point and detected no association with any of the variables tested.
UBM recipients express fewer KIRs that recognize HLA-C ligands compared to KIRs that recognize Bw4. Aliquots of donor or day +100, donor-derived recipient PBMCs were stained with 3 directly conjugated mAbs to designated KIR (DX9, KIR3DL1; EB6, KIR2DL1/2DS1; GL183, KIR2DL2/2DL3/2DS2). The means, 25th to 75th percentile ranges, and extreme values of the percentages of CD56+/CD3- cells expressing KIR by flow cytometry are shown in the box plots. Results are presented for donors or recipients separated by graft type (UBM: n = 33 donor, n = 38 recipient; TCD: n = 34 donor, n = 37 recipient). P = NS between any donor groups.
UBM recipients express fewer KIRs that recognize HLA-C ligands compared to KIRs that recognize Bw4. Aliquots of donor or day +100, donor-derived recipient PBMCs were stained with 3 directly conjugated mAbs to designated KIR (DX9, KIR3DL1; EB6, KIR2DL1/2DS1; GL183, KIR2DL2/2DL3/2DS2). The means, 25th to 75th percentile ranges, and extreme values of the percentages of CD56+/CD3- cells expressing KIR by flow cytometry are shown in the box plots. Results are presented for donors or recipients separated by graft type (UBM: n = 33 donor, n = 38 recipient; TCD: n = 34 donor, n = 37 recipient). P = NS between any donor groups.
NKG2A expression is increased in recipients of unrelated transplants, irrespective of graft manipulation, and is inversely correlated with KIR expression. Donor or day +100, donor-derived recipient PBMCs from UBM or TCD transplants were labeled with the directly conjugated mAb Z199, which stains NKG2A. The means, 25th to 75th percentile ranges, and extreme values of the percentages of CD56+/CD3- cells expressing NKG2A by flow cytometry are shown in the box plot on the left. Results are presented for donors (n = 71) or recipients (n = 70). The same cells were stained with a cocktail of directly conjugated mAbs KIR (DX9, EB6, GL183, and FES173, which stain CD158e, CD158a, CD158b, and CD158i, respectively). The percentage of NKG2A recovery was calculated as a ratio of the percent expression on recipient NK cells over that on donor NK cells (R/D) and plotted on the x-axis versus the R/D ratio of total KIR recovery (right). There was no difference between recipients of UBM or TCD transplants, so data are presented for both transplant types.
NKG2A expression is increased in recipients of unrelated transplants, irrespective of graft manipulation, and is inversely correlated with KIR expression. Donor or day +100, donor-derived recipient PBMCs from UBM or TCD transplants were labeled with the directly conjugated mAb Z199, which stains NKG2A. The means, 25th to 75th percentile ranges, and extreme values of the percentages of CD56+/CD3- cells expressing NKG2A by flow cytometry are shown in the box plot on the left. Results are presented for donors (n = 71) or recipients (n = 70). The same cells were stained with a cocktail of directly conjugated mAbs KIR (DX9, EB6, GL183, and FES173, which stain CD158e, CD158a, CD158b, and CD158i, respectively). The percentage of NKG2A recovery was calculated as a ratio of the percent expression on recipient NK cells over that on donor NK cells (R/D) and plotted on the x-axis versus the R/D ratio of total KIR recovery (right). There was no difference between recipients of UBM or TCD transplants, so data are presented for both transplant types.
It is possible that the corticosteroids used to treat acute GVHD may have affected NK cell recovery and function. However, patients receiving systemic corticosteroids (n = 52) had more NK cells (steroids; 45.7% ± 21.7% versus no steroids, 28.7% ± 21.0%: P = .002) and a higher percentage of NK cells producing IFN-γ (steroids, 51.8% ± 23.2% versus no steroids, 22.0% ± 16.4%: P = .001), demonstrating that any steroid effect does not completely impair NK cell recovery in vivo.
Recipients of UBM transplants have more IFN-γ-producing NK cells than recipients of TCD transplants. Donor or day +100, donor-derived recipient PBMCs from UBM (n = 24) or TCD (n = 25) transplants were incubated for 24 hours in IL-12 (10 ng/mL) and IL-18 (100 ng/mL). Harvested cells were permeabilized and stained intracellularly with a directly conjugated mAb to IFN-γ. The means, 25th to 75th percentile ranges, and extreme values of the percentages of CD56+/CD3- cells expressing IFN-γ by flow cytometry are shown in the box plot. Results are presented for donors or recipients.
Recipients of UBM transplants have more IFN-γ-producing NK cells than recipients of TCD transplants. Donor or day +100, donor-derived recipient PBMCs from UBM (n = 24) or TCD (n = 25) transplants were incubated for 24 hours in IL-12 (10 ng/mL) and IL-18 (100 ng/mL). Harvested cells were permeabilized and stained intracellularly with a directly conjugated mAb to IFN-γ. The means, 25th to 75th percentile ranges, and extreme values of the percentages of CD56+/CD3- cells expressing IFN-γ by flow cytometry are shown in the box plot. Results are presented for donors or recipients.
Incidence of acute GVHD correlates with increased IFN-γ production by donor-derived NK cells. Cumulative incidence estimates of acute GVHD in recipients of UBM or TCD transplants are shown. The percentage of day +100, donor-derived recipient CD3-/CD56+ NK cells producing IFN-γ was analyzed as described, and the results were analyzed with a Cox multivariate proportionate hazards model that included KIR expression, percentage of CD56+bright cells, graft type, IFN-γ production, and the incidence of acute GVHD. The recipients were further stratified by IFN-γ production by equal to or more than 50% or less than 50% of NK cells, which was the mean percentage of NK cells producing IFN-γ for all samples (left panel). The type of graft (UBM or TCD) did not independently correlate with acute GVHD but did accentuate the effect of IFN-γ expression (right panel).
Incidence of acute GVHD correlates with increased IFN-γ production by donor-derived NK cells. Cumulative incidence estimates of acute GVHD in recipients of UBM or TCD transplants are shown. The percentage of day +100, donor-derived recipient CD3-/CD56+ NK cells producing IFN-γ was analyzed as described, and the results were analyzed with a Cox multivariate proportionate hazards model that included KIR expression, percentage of CD56+bright cells, graft type, IFN-γ production, and the incidence of acute GVHD. The recipients were further stratified by IFN-γ production by equal to or more than 50% or less than 50% of NK cells, which was the mean percentage of NK cells producing IFN-γ for all samples (left panel). The type of graft (UBM or TCD) did not independently correlate with acute GVHD but did accentuate the effect of IFN-γ expression (right panel).
Increased KIR expression correlates with increased survival
Using the same Cox model, the only variable that was independently predictive of survival was KIR expression. Fitting KIR as a continuous variable in a Cox model yields a relative risk of 0.36 (β = -1.02, P = .037). Thus, an increase in KIR ratio of 0.1 corresponds to an average decreased risk of death of 25%. Adjusting for T-cell depletion status results in a more pronounced association between KIR and survival, producing a relative risk of 0.26 (β = -1.36, P = .02). The worst survival was seen in recipients of TCD transplants with low KIR expression. The Kaplan-Meier survival estimate curves are stratified by KIR expression ratio of equal to or more than 0.6 or less than 0.6, which was the median R/D ratio of all samples (Figure 6). The relative risk of death for a KIR ratio of equal to or more than 0.6 was 0.5 (P = .056). Stratification by T-cell depletion status accentuated the correlation between KIR expression and survival, but did not exert an independent effect, and yielded a relative risk of 0.4 (P = .03).
Discussion
Alloreactive NK cells have the potential to affect clinical outcomes after HCT.20 Clinical trials using KIR-ligand mismatched donors in several transplantation settings have produced conflicting results.20-26,32 Some discrepancies may be explained by the inconsistent use of T-cell depletion. To evaluate our hypothesis that T cells in unrelated grafts hinder the development or function of recovering NK cells, we analyzed pairs of donor and donor-derived recipient NK cells at day +100. This study provides the first demonstration that in vivo KIR reconstitution and NK cell function are affected by T cells in the graft and that these alterations correlate with clinical outcomes after unrelated adult donor transplantation.
In agreement with others, we observed that NK cells are the predominant lymphocyte subset to reconstitute by day +100 after unrelated transplantation.33 The overall percentage of NK cells was not affected by the presence of T cells in the graft, suggesting that T cells influence the function rather than the quantity of NK cells. Accordingly, we found significantly diminished KIR recovery in UBM transplant recipients compared to their donors, whereas TCD transplant recipients were much less affected. Remarkably, in our multivariate model impaired KIR expression was the only independent predictor of decreased overall survival. The ability to correlate a single KIR measurement from day +100 with survival underscores the importance of rapid recovery of mature, functional NK cells. Our findings are consistent with a previous analysis of KIR expression after HLA-matched related or unrelated transplantation in 18 patients. Parham et al showed that the KIR repertoires of recovering NK cells usually recapitulate those of their donors over 6 to 9 months, but that the idiosyncratic low KIR recovery was associated with severe clinical complications.34 Although it is unlikely that KIR alloreactivity confounded our results (the TCD and UBM groups had similar numbers of KIR mismatch transplants), our study was underpowered to look for an independent effect of KIR alloreactivity on NK cell recovery or transplantation outcomes. KIR acquisition in the presence or absence of KIR ligands may be important clinically. Studies of larger cohorts that include stratification by KIR mismatch status and more detailed infection and complication data are underway and will clarify the role of KIR mismatch on NK cell function and clinical outcomes.
The finding that expression of HLA-C-binding KIRs was more affected after UBM transplantation than was KIR3DL1, which binds to HLA Bw4, is intriguing. Several possible mechanisms may regulate KIR expression. Hypomethylated DNA is required for KIR gene expression.35-37 However, even if DNA is accessible, it is still unknown whether the same transcription factors act on individual KIR gene loci.38 Although not yet demonstrated in humans, we anticipate that forward and reverse transcriptional switches may be active on KIR similar to those identified to control the variegated expression of murine Ly49 genes.39 There may also be posttranscriptional mechanisms to determine the final KIR repertoire. An HCT study with matched sibling donors demonstrated that the class I HLA-type (KIR ligand) of the recipient has a subtle effect on KIR expression.40 A similar effect of class I HLA ligands is seen in murine models studying Ly49 expression,41,42 suggesting that NK cell receptors are “selected” or “educated” by the environment during NK cell development. Understanding the role of each of these possible mechanisms will be crucial to determine how T cells may interfere with KIR expression.
Survival correlates with increased KIR expression on donor-derived NK cells after transplantation. Kaplan-Meier survival estimates in recipients of UBM or TCD transplants are shown below. The ratios of day +100, donor-derived recipient CD3-/CD56+ NK cells to donor cells expressing KIR were analyzed as described. The results were analyzed with a Cox multivariate proportionate hazards model that included KIR expression, percentage of CD56+bright cells, IFN-γ production, and survival (n = 72). The recipients were further stratified by KIR expression ratio of equal to or more than 0.6 or less than 0.6, which was the mean R/D ratio of all samples (left panel). Stratification based on graft type (UBM, n = 35; TCD, n = 37) accentuates the correlation of KIR expression with survival but was not an independent predictor (right panel).
Survival correlates with increased KIR expression on donor-derived NK cells after transplantation. Kaplan-Meier survival estimates in recipients of UBM or TCD transplants are shown below. The ratios of day +100, donor-derived recipient CD3-/CD56+ NK cells to donor cells expressing KIR were analyzed as described. The results were analyzed with a Cox multivariate proportionate hazards model that included KIR expression, percentage of CD56+bright cells, IFN-γ production, and survival (n = 72). The recipients were further stratified by KIR expression ratio of equal to or more than 0.6 or less than 0.6, which was the mean R/D ratio of all samples (left panel). Stratification based on graft type (UBM, n = 35; TCD, n = 37) accentuates the correlation of KIR expression with survival but was not an independent predictor (right panel).
High levels of CD94/NKG2A expression after both UBM and TCD transplantation were found in this study. Both human and murine NK cell developmental models have demonstrated very early expression of CD94/NKG2A, which later decreases as KIR or Ly49 are expressed on maturing cells.17,30,31 The significant inverse correlation found between CD94/NKG2A and KIR is consistent with this model and raises the possibility that low KIR expression in UBM transplants reflects a relative block in NK cell development rather than an independent effect on KIR expression per se. This interpretation is supported by a recent study of immune reconstitution after T-cell depletion, haploidentical, KIR-ligand mismatched HCT where the low KIR and high CD94/NKG2A-expressing NK cells were functionally impaired in vitro as evidenced by poor cytotoxicity.43
We found a significant difference between the percentages of recipient NK cells that were able to produce IFN-γ after UBM transplantation compared to TCD transplantation. In our multivariate model, however, the only independent predictor of acute GVHD was increased NK cell IFN-γ production, regardless of transplant type or the percentage of CD56+bright NK cells. The relationship between IFN-γ, T cells, and acute GVHD is complex and not fully understood. It is established that T cells mediate GVHD44 and that IFN-γ can induce class I molecule up-regulation further stimulating T cells,45 but the cause and effect roles are unclear. Different factors may influence the development of chronic GVHD, with which there was no association with any of the variables tested in our model. Although the mechanisms are unknown, our data show that measurable variations in the function of reconstituted NK cells can have a profound impact on clinical outcomes. It remains to be shown whether diminished KIR in UBM transplantation and loss of self-discrimination is directly responsible for increased IFN-γ production.
The therapeutic success of KIR-mismatch strategies that use donor selection criteria to predict the alloreactivity of NK cells is ultimately dependent on the development of mature, functional, alloreactive NK cells. We show that the processes of NK development and KIR expression are affected by the presence of T cells. T cells may act directly, via competition for cytokines such as IL-15 or IL-7, which are known to play a role in homeostasis of both NK and T cells.46-49 They may also act indirectly, by their effect on the posttransplantation hematopoietic environment. T cells have been shown to activate CD56+bright NK cells via IL-2 in the lymph nodes of healthy donors,50 and 2 studies suggest that the beneficial effect of alloreactive NK cells in KIR-ligand mismatched transplantation is overwhelmed by T cell-mediated processes such as acute GVHD.21,23
Although many transplant variables may potentially disrupt NK cell reconstitution, our study is the first to directly compare KIR reconstitution and NK function between UBM and TCD transplant recipients and demonstrates a definitive role for the presence of T cells in the graft. Although the UBM and TCD groups were well matched for patient characteristics, T cells themselves may not be directly responsible for all findings. We acknowledge that several variables associated with UBM versus TCD grafts may be involved in the mechanism explaining lower KIR expression, such as greater incidences of GVHD and more intense use of immunosuppressive medications. Cyclosporin, for example, has been shown to affect NK cell differentiation and cytotoxicity in vitro,51 but there was no significant difference in its use between the transplantation groups studied here. Similarly, there was no significant difference in systemic corticosteroid use in our study population. Other potentially confounding transplant variables include the choice of preparative regimen (which was not significantly different between transplant types in our study), the extent and method of T-cell depletion, and the precise choice and intensity of GVHD prophylaxis. We are reassured that regardless of technique, the T-cell depletions were effective; we measured approximately 40% fewer T cells in the TCD graft recipients compared to UBM graft recipients, and those patients had lower incidences of acute and chronic GVHD.
In summary, we conclude that the development of functional NK cells expressing mature KIR repertoires is affected by T cells in the graft, whether by direct or indirect mechanisms, and correlates with improved clinical outcomes after unrelated transplantation. Our findings provide a compelling explanation for many of the discrepant clinical outcomes seen among trials of KIR-ligand mismatched transplants. Prospective, well-controlled, longitudinal studies are underway to examine the kinetics of NK development and KIR reconstitution and to clarify the mechanisms underlying the correlations with clinical outcomes.
Prepublished online as Blood First Edition Paper, August 30, 2005; DOI 10.1182/blood-2005-04-1644.
Supported in part by National Institutes of Health grants P01-CA-65493 (J.S.M.), P01-CA-111412-01 (J.S.M.), R01-HL-55417 (J.S.M.), and T32 HL-07062 (S.C.). Additional support was through the NMDP, the Health Resources and Services Administration no. 240-97-0036, and Office of Naval Research N00014-93-1-0658 to the NMDP.
S.C. planned experiments, analyzed data, and wrote the paper; V.M. and R.W. performed research; T.L.B. analyzed data; S.S. procured the sample and selected the cohort; D.J.W. designed the research and wrote the paper; and J.S.M. designed research, analyzed data, and wrote the paper.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We would like to thank Tanya Warren at the Center for International Blood and Marrow Transplant Research (CIBMTR) for her assistance in sample procurement and data collection and John Klein at the CIBMTR for reviewing the manuscript. The views expressed in this article do not reflect the official policy or position of the Department of the Navy, the Department of Defense, or the US Government.