Abstract
By means of its antiangiogenic activity, thrombospondin-1 (TSP-1) exerts indirect antitumoral action on solid tumors. Here, we investigated potential antitumor action in an in vitro cell model for promyelocytic leukemia (NB4-LR1), resistant to retinoid maturation. Purified soluble TSP-1 added to cultures induced a strong dose-dependent growth inhibition and a slowly developing maturation-independent cell death. Recombinant fragments of TSP-1 allowed mapping of these activities to its type 3 repeat/C-terminal domain, features that are distinct from those of TSP-1 action on solid tumors, previously ascribed to the type 1 repeat domain. Cell death in leukemia was characterized as a caspase-independent mechanism, without DNA fragmentation, but phosphatidylserine externalization followed by membrane permeabilization. Mitochondria membrane depolarization was inherent to TSP-1 action but did not produce release of death-promoting proteins (eg, noncaspase apoptosis regulators, apoptosis-induced factor [AIF], endonuclease G, or Omi/HtrA2 or the caspase regulators, cytochrome c or second mitochondrial activator of caspase/direct inhibitor of apoptosis protein-binding protein with low isoelectric point [Smac/DIABLO]). Although detected, reactive oxygen species (ROS) production was likely not involved in the death process. Finally, receptor agonist RFYVVM and RGD peptides indicated that TSP-1 death effects are mediated by membrane receptors CD47 and αvβ3. These results demonstrated a new domain-specific antitumoral activity of TSP-1 on a leukemia cell line, which extends TSP-1 therapeutic potential outside the area of vascularized solid tumors. (Blood. 2005;106:658-667)
Introduction
Cell interaction with extracellular matrix proteins is essential to regulate proliferation, differentiation, and cell death.1-3 Thrombospondin-1 (TSP-1) belongs to a family of multidomain and multifunctional glycoproteins that regulate cell proliferation, migration, and differentiation and is important for embryonic development, morphogenesis, inflammation, tumor metastasis, and multiple other processes.4-6 TSP-1 is a secreted component of extracellular matrix that supports attachment and motility of a variety of normal and neoplastic cell types.5,7,8 Because it also functions as soluble protein that antagonizes the proadhesive activities of other matrix proteins, TSP-1 has been defined as a matricellular protein modulating cell-matrix interactions.9,10 It can affect matrix structure through its ability to interact with matrix components and to activate transforming growth factor-β1 (TGF-β1).11 TSP-1 is also a potent physiological inhibitor of angiogenesis by impairing endothelial cell growth and migration and by acting on endothelial cell cycle progression and apoptosis; thus, down-expression of TSP-1 is important for tumor progression.12-15 Many of the TSP-1 functions have been located within specific domains of the molecule that bind to various membrane receptors, including integrins of the β1 and β3 family, CD47/integrin-associated protein (CD47/IAP), CD36, and proteoglycans.5,8 Therefore, cell responses to TSP-1 probably reflect the integration of multiple membrane signals depending on the cell type and its repertoire in membrane receptors.
TSP-1 function in tumor cell differentiation and apoptosis remains poorly explored. TSP-1 has been described to be positively involved in retinoic acid-induced maturation of neuroblastoma cells and the acute myeloblastic leukemic cell line HL-60.16,17 In the HL-60 cell line, it was shown to induce a caspase-dependent cell death mediated by CD36.18 It is also able to trigger a caspase-independent cell death that is accompanied by selective mitochondrial changes in B-chronic lymphocytic leukemia through binding to CD47.19,20 TSP-1 also induces CD47-mediated killing of breast cancer cells acting via heterotrimeric Gi-dependent inhibition of protein kinase A activity.21
NB4 cells have been derived from leukemic cells of a patient with acute promyelocytic leukemia (APL)22 and carry the characteristic t(15;17) translocation giving rise to the expression of the retinoic acid receptor fusion protein (promyelocytic leukemia-RARα [PML-RARα]).23,24 Pharmacologic doses of all-trans retinoic acid (ATRA) can convert the fusion protein into an active receptor and restore granulocytic maturation of these cells so that its administration to APL patients either alone or combined with chemotherapy is of therapeutic benefit and can improve the survival prognosis.25,26 The NB4-LR1 cell subline is resistant to maturation by ATRA and was isolated from the early culture of NB4 cells derived from leukemic cells of the APL patient.27 It was found that NB4-LR1 cells required adenosine 3′,5′-cyclic monophosphate (cAMP) analog and ATRA signaling cross-talk to undertake the granulocytic maturation program, suggesting interdependent ATRA and cAMP signaling pathways in APL maturation.28 Notably, a wide spectrum of membrane signals have been shown to modulate or to cooperate with retinoids to induce, in NB4 leukemic cells, maturation or cell death independently of maturation.29 No investigation has been carried out so far to know whether biologic response to TSP-1 signaling could be exploited in APL.
In this work, we investigated the biologic outcomes of TSP-1 signaling or ATRA and TSP-1 combined signaling in NB4-LR1 leukemic immature blast cells refractory to ATRA maturation and defective in endogenous TSP-1 synthesis and secretion. The homotrimeric TSP-1 molecule was analyzed by means of domain-specific recombinant TSP-1-derived proteins to map the antitumoral activities of this protein. The C-terminal domain of TSP-1 comprising the type 3 repeats and the C-terminal globular region is shown herein to signal, by itself or combined with ATRA, a caspase-independent cell death in these leukemic cells through simultaneous ligation of CD47 and the integrin αvβ3.
Materials and methods
Cell culture and treatment
The APL cell line NB4 and the resistant APL cell line NB4-LR1 were essentially cultured in RPMI 1640 medium (Invitrogen, Carlsbad, CA) as previously described.22,28 Cells (2 × 105/mL) were untreated or treated for 4 days with 1 μM ATRA (Sigma, St Louis, MO) in the absence or presence of soluble human purified platelet TSP-1 or recombinant fragments for specific domains of TSP-1. In some experiments, cells were cultured with benzoyloxycarbonyl-Val-Ala-Asp-fluoromethylketone (z-VAD-fmk) or RFYVVMWK (4N1-1), GRGDS, or VTCG peptides (BACHEM Biochimie, Voisins-le-Bretonneux, France), selenium (Sigma), or ebselen (Calbiochem, San Diego, CA). Cell morphology was evaluated by May-Grünwald-Giemsa (MGG) staining. Biochemical criterion of granulocytic differentiation was assessed by the nitroblue tetrazolium (NBT; Sigma) dye reduction assay.22,27,28
Purified TSP-1 and TSP-1 recombinant fragments
Human TSP-1 was purified from the supernatant of thrombin-activated platelets as previously described.30 Recombinant proteins including specific sequences for the NH2-terminal (NTSP-1), the 3 type 1 repeats (3TSR), and the type 3 repeat/C-terminal domain (T3C1) of TSP-1 were produced in Drosophila S2 cells. The preparation of 3TSR has been described previously.31 NTSP-1 was prepared using the forward primer 573htsp1f (GAT GAT CCA TGG AAC CGC ATT CCA GAG TCT GGC) and the reverse primer 574htsp1r (GAT ACC GGT GTT AGT GCG GAT GGC AGG GCT). The polymerase chain reaction (PCR) product was sequenced and cloned between the NcoI and the AgeI sites of the vector pMT/BiP/V5-HisA (Invitrogen). The recombinant protein includes the vector-derived sequence RSPW at the N-terminal. T3C1 was prepared using the forward primer 575htsp1f (GAT GAT CCC GGG GAC ACA GAC CTG GAT GGC TGG) and the reverse primer 576htsp1r (GAT ACC GGT GGG ATC TCT ACA TTC GTA TTT). The PCR product was sequenced and cloned between the XmaI and the AgeI sites of the vector. The recombinant protein includes the sequence RSPWPG at the N-terminal. All of the recombinant proteins contain the sequence TGHHHHHH at the C-terminal. Vector transfection, cell selection, and protein expression and purification were performed as described previously.31
RNA preparation and Northern blot analysis
Total RNA was extracted from 107 cells using TRIZOL Reagent (Invitrogen) according to the manufacturer's instructions. Twenty micrograms of RNA from each sample was denatured in formamide, electrophoresed on a 1% agarose gel containing 2.2 M formaldehyde, and transferred overnight onto nylon membrane (Hybond-N; Amersham Pharmacia Biotech, Orsay, France) using standard protocols.32 Membrane was probed with a 32P-labeled fragment of human cDNA specific for TSP-1 encoding amino acids sequence in the NH2-terminus of the molecule (a kind gift from Valerie Castle, University of Michigan Medical School).
Immunofluorescence analysis
Fresh or paraformaldehyde (PFA)-fixed cells33 in RPMI medium containing 2% bovine serum albumin (BSA) were incubated for 30 minutes at room temperature with mouse monoclonal antibodies to CD36, the β1 or αv integrin subunit (Immunotech, Marseille, France), the β3 integrin subunit or CD47 (BD Biosciences, Rungis, France), rabbit antiserum to TSP-1 (R1),34 or αv (Chemicon International, Temecula, CA). Alexa Fluor 488- and 594-conjugated anti-mouse and anti-rabbit immunoglobulins G (IgGs) were used as secondary antibodies (Molecular Probes, Eugene, OR). Immunofluorescence was analyzed using a FACSCalibur flow cytometer (BD Biosciences) or a Bio-Rad MRC 1024 confocal imaging system (Hemel Hempstead, United Kingdom) equipped with an inverted Diaphot 300 Nikon microscope (Nikon France, Champigny-Sur-Marne, France) and a krypton-argon ion laser. Confocal images were acquired using the Bio-Rad Lasersharp V3.2 software through a 60×/1.4 numerical aperture oil immersion objective lens (Nikon).
For analysis of mitochondrion protein localization, cells were permeabilized for 10 minutes with 0.1% saponin in phosphate-buffered saline (PBS) containing 10% BSA (PBS-BSA-0.1% saponin) and then incubated with monoclonal antibody to cytochrome c (BD Biosciences) or rabbit polyclonal antibodies to second mitochondrial activator of caspase/direct inhibitor of apoptosis protein-binding protein with low isoelectric point (Smac/DIABLO) (ProSci, Poway, CA), Omi/HtrA2 (Alexis Biochemicals, Paris, France), apoptosis-induced factor (AIF), or endonuclease G (Sigma) in PBS-BSA-0.1% saponin. Cells were washed in PBS-BSA-0.01% saponin and then incubated with Alexa Fluor-conjugated secondary antibodies.
Subcellular fractionation
Cells in PBS were resuspended in buffer (250 mM sucrose, 10 mM KCl, 1 mM MgCl2, 1.5 mM EDTA [ethylenediaminetetraacetic acid], 1.5 mM EGTA [ethylene glycol tetraacetic acid], 1 mM dithiothreitol [DTT], 20 mM HEPES [N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid] pH 7.4, 0.1 mM phenylmethylsulfonyl fluoride [PMSF], and 10 μg/mL leupeptin, sodium orthovanadate, sodium fluoride, and benzamidine) for 20 minutes on ice and then lysed using a Dounce tissue grinder. Nuclei and unlysed cells were sedimented at 1000g for 10 minutes, and the supernatant was centrifuged at 100 000g to recover organelle- and membrane-free cytosol (S100 fraction). Cytochrome c was immunodetected by Western blotting.
Immunoprecipitation and Western blot analysis
Cells (107) and culture media corresponding to the collected cells were solubilized for 30 minutes at 4°C by adding lysis buffer containing 1% Triton X-100, 1 mM MgCl2, 2 mM CaCl2, and the following protease inhibitors (Calbiochem): 100 μM leupeptin, 9 kallikrein inhibitory unit (KIU)/mL aprotinin, 2 mM sodium orthovanadate, 10 mM sodium fluoride, and 1 mM P-aminoethylbenzenesulfonyl fluoride (AEBSF) in 20 mM Tris (tris(hydroxymethyl)aminomethane)-HCl buffer (pH 7.4). Immunoprecipitation assays were carried out on soluble material essentially as reported,33 using P10 mouse monoclonal antibody to TSP-1 (Immunotech) and protein A Sepharose CL-4B (Amersham Pharmacia Biotech). The immune complexes were analyzed by Western blotting, as described,35 using P10 antibody (20 μg/mL) and peroxidase-conjugated secondary antibody (1:10 000; Dako, Glostrup, Denmark).
For Western blot analysis of total cell extract, cells were solubilized for 10 minutes at 100°C in the presence of 2% sodium dodecyl sulfate (SDS), 5 mM N-ethylmaleimide acid (NEM), and 2 mM EDTA and analyzed using mouse monoclonal antibody to poly(adenosine diphosphate-ribose) polymerase (PARP) (Calbiochem) or rabbit polyclonal antibodies to human caspase-3, caspase-8, or Bcl-2 (Santa Cruz Biotechnology, Santa Cruz, CA).
Assays for cell death
Annexin V binding and propidium iodide (PI) staining. Cell death was assessed by analyzing phosphatidylserine (PS) membrane outside exposure and cell membrane permeability36,37 by flow cytometry using an apoptosis detection kit (Bender MedSystems, Vienna, Austria) for cell double labeling with 1 μg/mL fluorescein isothiocyanate (FITC)-labeled annexin V and PI.
Caspase activity. Caspase-3 activity was measured on cell extract (20 to 50 μg) by a colorimetric procedure using the specific peptide substrate DEVD-pNa, as described.38
DNA fragmentation. DNA was isolated from 2 × 106 cells according to a salting out procedure previously described,39 and internucleosomal fragmentation was analyzed as already reported.40
Mitochondrial membrane potential determination. Determination of the mitochondrial transmembrane potential (ΔΨm) was assessed using the 3,3′dihexyloxacarbocyanine iodide (DiOC6(3)) lipophilic cationic fluorochrome (20 nM; Uptima, Montluçon, France).
Reactive oxygen species (ROS) production. Intracellular ROS was measured throught H2O2 production using the oxidant-sensitive nonfluorescent dye 2′-7′-dichlorofluorescein diacetate (DCFH-DA) (2 μM; Molecular Probes), which is oxidized by H2O2 and generates fluorescent dichlorofluorescein (DCF).
Results
TSP-1 and TSP-1 receptor expression in NB4 leukemic cell lines
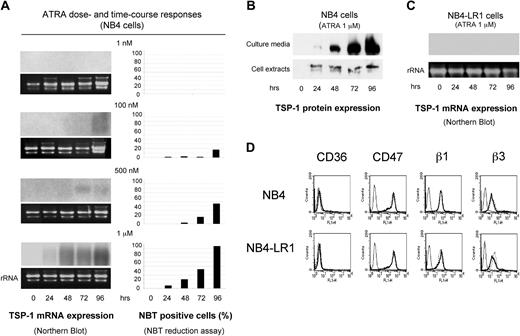
TSP-1 expression was examined both in ATRA maturation-sensitive NB4 cells and in ATRA maturation-resistant NB4-LR1 cells. In NB4 cells, ATRA dose-dependent TSP-1 mRNA expression was found to correlate with detection of granulocytic maturation, as measured by the NBT dye reduction assay (Figure 1A) and as viewed by MGG staining showing segmented nuclei typical of differentiated phenotype (not shown). TSP-1 protein expression, when examined by quantitative immunoprecipitation during 1 μM ATRA treatment (Figure 1B), showed a modulation in the pattern of TSP-1 protein expression similar to that obtained for TSP-1 transcript. Upon its induction by ATRA, TSP-1 was mostly secreted into the extracellular culture medium. In NB4-LR1 cells, neither TSP-1 transcript (Figure 1C) nor TSP-1 protein (not shown) expression was detected upon 1 μM ATRA treatment. However, when induced to mature by cotreatment with cAMP analog (8-(4-chlorophenylthio)-cAMP [8-CPT-cAMP]), NB4-LR1 expressed TSP-1 similarly to what was observed in ATRA-treated NB4 cells (not shown).
TSP-1 and its membrane receptors' expression in NB4 and NB4-LR1 cell lines. Maturation-sensitive NB4 cells and maturation-resistant NB4-LR1 cells were cultured for 4 days either untreated or treated with 1 nM to 1 μM ATRA or 1 μM ATRA and processed for examination of TSP-1 transcript (A, C) and protein level expression (B) or TSP-1 receptors' membrane expression (D). (A) Cell maturation was monitored by the NBT dye reduction assay. Total RNA (20 μg) was hybridized with a 32P-labeled fragment of human cDNA for TSP-1. Equivalent loading and integrity of each RNA preparation were evaluated by ethidium bromide staining of the 28S rRNA bands. (B) Triton X-100 cell lysates were prepared from maturation-sensitive NB4 cells and processed for immunoprecipitation and Western blotting for analysis of TSP-1 protein expression, as described in “Materials and methods.” Cell secretion of TSP-1 into the extracellular medium was similarly analyzed upon Triton X-100 solubilization of the corresponding culture media. Here, Triton X-100 cell extract and Triton X-100-solubilized culture medium coming from 4 × 106 NB4 cells and 1.2 × 105 NB4 cells, respectively, were analyzed. (D) Untreated (dotted line) or ATRA-treated (1 μM; bold solid line) NB4 and NB4-LR1 cells (2 × 105) were incubated with 20 μg/mL monoclonal antibodies to CD36, CD47, the β1 or β3 integrin subunit, or 20 μg/mL isotype-match control antibody (thin solid line). Alexa Fluor 488-conjugated anti-mouse IgG was used as secondary antibody (1:700), and cells were analyzed by flow cytometry.
TSP-1 and its membrane receptors' expression in NB4 and NB4-LR1 cell lines. Maturation-sensitive NB4 cells and maturation-resistant NB4-LR1 cells were cultured for 4 days either untreated or treated with 1 nM to 1 μM ATRA or 1 μM ATRA and processed for examination of TSP-1 transcript (A, C) and protein level expression (B) or TSP-1 receptors' membrane expression (D). (A) Cell maturation was monitored by the NBT dye reduction assay. Total RNA (20 μg) was hybridized with a 32P-labeled fragment of human cDNA for TSP-1. Equivalent loading and integrity of each RNA preparation were evaluated by ethidium bromide staining of the 28S rRNA bands. (B) Triton X-100 cell lysates were prepared from maturation-sensitive NB4 cells and processed for immunoprecipitation and Western blotting for analysis of TSP-1 protein expression, as described in “Materials and methods.” Cell secretion of TSP-1 into the extracellular medium was similarly analyzed upon Triton X-100 solubilization of the corresponding culture media. Here, Triton X-100 cell extract and Triton X-100-solubilized culture medium coming from 4 × 106 NB4 cells and 1.2 × 105 NB4 cells, respectively, were analyzed. (D) Untreated (dotted line) or ATRA-treated (1 μM; bold solid line) NB4 and NB4-LR1 cells (2 × 105) were incubated with 20 μg/mL monoclonal antibodies to CD36, CD47, the β1 or β3 integrin subunit, or 20 μg/mL isotype-match control antibody (thin solid line). Alexa Fluor 488-conjugated anti-mouse IgG was used as secondary antibody (1:700), and cells were analyzed by flow cytometry.
Potential membrane receptors for TSP-1, such as CD47 and the β1 and β3 integrin families were similarly expressed in NB4 and NB4-LR1 cells. Expression of these membrane markers was not modulated by ATRA treatment (Figure 1D), contrasting with the leukocyte β2 integrin, CD11c, for which membrane expression was reported to be up-regulated.28,41 The 2 cell lines were negative for CD36.
We therefore investigated whether TSP-1, upon its synthesis and secretion induced by ATRA in NB4 cells, could play a role in maturation/apoptosis programs triggered by retinoids. To this aim, the ATRA maturation-resistant NB4-LR1 cells, which express potential TSP-1 receptors but do not synthesize TSP-1 in response to ATRA, constitute an exquisite cell model to check whether exogenous TSP-1 signaling could act with ATRA for antitumoral responses.
Cell growth inhibition and cell death induction by TSP-1 in NB4-LR1 cells
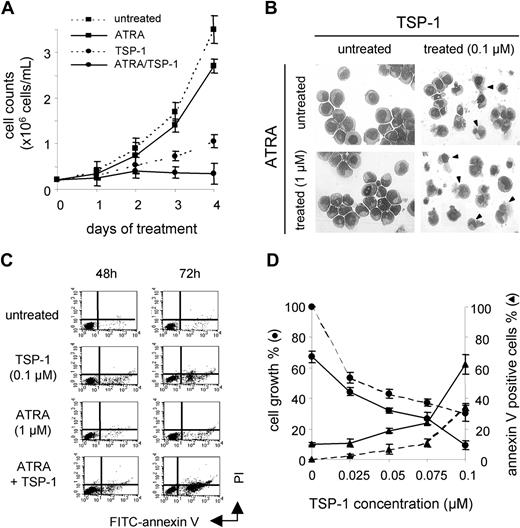
NB4-LR1 cells, untreated or treated with ATRA, were cultured in the absence or presence of soluble purified TSP-1. Within 1 to 2 days of cell treatment with TSP-1, cell growth was inhibited (Figure 2A), and within 3 days, cell death was observed under the microscope while it was not detected with ATRA alone. Cell morphology showed no cells with chromatin condensation, typical of nuclear events of apoptosis. Instead, cells with apparent intact nucleus but damaged plasma membrane were observed (Figure 2B), and features of differentiated cells were not seen, as further analyzed by NBT dye reduction assay (not shown). However, significant increase in membrane outside exposure of PS was detected at day 2 of both TSP-1 or ATRA treatment (Figure 2C). A further increase in PS exposure was observed upon ATRA/TSP-1 cotreatment essentially due to an additive effect. Cell necrosis was not detected at this time as determined by PI labeling but was present at day 3 in cells cultured with TSP-1 but not ATRA alone (Figure 2C, upper right rectangle, annexin V/PI-positive cells).
NB4-LR1 cell death induction by TSP-1. (A) NB4-LR1 cells untreated or treated with ATRA (1 μM) with or without TSP-1 (0.1 μM) were cultured in microwell culture plate for 4 days. Cell growth was quantified by cell counting in a Malassez hemocytometer. Results are expressed as mean ± SEM of 2 experiments. (B) Morphology of MGG-stained untreated or ATRA-treated cells after 4 days of culture in the absence or the presence of purified TSP-1 (0.1 μM) showed cells with no chromatin condensation but damaged plasma membrane when cultured with TSP-1 with or without ATRA (arrows). Cells were analyzed using an upright epifluorescence microscope (Leica DMR, Leica, Rueil-Malmaison, France) through a Plan Apo 63×/1.32 numerical aperture oil immersion objective lens (Leica), and images were captured with a color camera LEI-750D CE system and acquired using the Leica QWin V2.2 software. (C) Flow cytometry analysis of FITC-annexin V and PI-stained untreated or ATRA-treated (1 μM) NB4-LR1 cells cultured with or without TSP-1 (0.1 μM) for 3 days. Results, expressed as percent of positive cells for annexin V labeling, are as follows: at day 2: untreated 3%, TSP-1 10%, ATRA 8%, ATRA plus TSP-1 22%; and at day 3: untreated 6%, TSP-1 19%, ATRA 15%, ATRA plus TSP-1 42%. (D) NB4-LR1 cells untreated or treated with ATRA (1 μM) were cultured for 4 days with or without increasing concentrations of purified TSP-1 (0.025 to 0.1 μM). Cell growth was expressed as percent of growth compared with untreated cells (•), and cell death, as quantified by annexin V labeling (▴), was expressed as percent of positive cell detection upon flow cytometry analysis: broken line indicates untreated cells; solid line, ATRA-treated cells. Results are expressed as mean ± SEM of 3 experiments.
NB4-LR1 cell death induction by TSP-1. (A) NB4-LR1 cells untreated or treated with ATRA (1 μM) with or without TSP-1 (0.1 μM) were cultured in microwell culture plate for 4 days. Cell growth was quantified by cell counting in a Malassez hemocytometer. Results are expressed as mean ± SEM of 2 experiments. (B) Morphology of MGG-stained untreated or ATRA-treated cells after 4 days of culture in the absence or the presence of purified TSP-1 (0.1 μM) showed cells with no chromatin condensation but damaged plasma membrane when cultured with TSP-1 with or without ATRA (arrows). Cells were analyzed using an upright epifluorescence microscope (Leica DMR, Leica, Rueil-Malmaison, France) through a Plan Apo 63×/1.32 numerical aperture oil immersion objective lens (Leica), and images were captured with a color camera LEI-750D CE system and acquired using the Leica QWin V2.2 software. (C) Flow cytometry analysis of FITC-annexin V and PI-stained untreated or ATRA-treated (1 μM) NB4-LR1 cells cultured with or without TSP-1 (0.1 μM) for 3 days. Results, expressed as percent of positive cells for annexin V labeling, are as follows: at day 2: untreated 3%, TSP-1 10%, ATRA 8%, ATRA plus TSP-1 22%; and at day 3: untreated 6%, TSP-1 19%, ATRA 15%, ATRA plus TSP-1 42%. (D) NB4-LR1 cells untreated or treated with ATRA (1 μM) were cultured for 4 days with or without increasing concentrations of purified TSP-1 (0.025 to 0.1 μM). Cell growth was expressed as percent of growth compared with untreated cells (•), and cell death, as quantified by annexin V labeling (▴), was expressed as percent of positive cell detection upon flow cytometry analysis: broken line indicates untreated cells; solid line, ATRA-treated cells. Results are expressed as mean ± SEM of 3 experiments.
Based on annexin V labeling (Figure 2D), cell death was found to be TSP-1 dose dependent. However, morphologically, cell death was only observed with the highest doses of TSP-1 (0.075 and 0.1 μM). Combinatorial effect of 0.1 μM TSP-1 with ATRA caused a greater enhancement of cell death at day 4 (62% annexin V-positive cells) when compared with TSP-1 alone (34% positive cells) or ATRA alone (11% positive cells). Quantification of cell growth also indicated a strong dose-dependent inhibition at all TSP-1 concentrations, in untreated (46% to 70% inhibition) or ATRA-treated cells (56% to 91% inhibition), when compared with control untreated cells (Figure 2D).
Given the known biologic effect of TSP-1 on TGF-β activation, we next examined whether cell death induced in the presence of TSP-1 could be mediated by endogenous TGF-β.11,31,42 Cotreatment of NB4-LR1 cells for 4 days with ATRA and purified recombinant TGF-β (10 μg/mL) showed no increase in the rate of annexin V-positive cells when compared with ATRA alone (not shown).
Together, these results indicated that soluble TSP-1 action on NB4-LR1 leukemic immature blast cells leads to a composite biologic response linking growth inhibition and cell death. These responses are increased in the presence of ATRA independently of any maturation response.
Involvement of the TSP-1 C-terminal domain in NB4-LR1 cell death induction
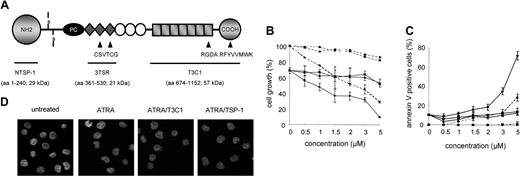
To further decipher the molecular mechanisms by which TSP-1 induced NB4-LR1 cell death, 3 recombinant fragments of TSP-1 (0.5 to 5 μM) containing the specific sequence for the N-terminal domain (NTSP-1), the type 1 repeat (3TSR), and the type 3 repeat/C-terminal domain (T3C1) of TSP-1 (Figure 3A), were assayed on NB4-LR1 cells.
While only slight growth inhibition was demonstrated either with the NTSP-1 or the 3TSR fragment, a T3C1 dose-dependent strong inhibition of cell growth was measured in untreated cells (15% to 71% inhibition) and ATRA-treated cells (44% to 90% inhibition) (Figure 3B). The T3C1/ATRA curve paralleled the T3C1 curve, suggesting an additive effect of TSP-1 with ATRA. Thus, ATRA does not appear to make cells more sensitive to T3C1 action. Cell death was observed under the microscope in untreated or ATRA-treated cells within 3 days of culture with 2 to 5 μM of the T3C1 fragment, similar to what was observed with the entire TSP-1. When quantified, cell death by T3C1 alone was dose dependent, showing 28% of annexin V-positive cells for the highest dose (5 μM) (Figure 3C), while no positive cell was detected with the NTSP-1 or the 3TSR fragment. By contrast to the growth inhibition response, the cell death response to T3C1 high dose (5 μM) was amplified by ATRA treatment (10% positive cells with ATRA alone versus 72% positive cells with 5 μM T3C1). Time-course experiments with T3C1/ATRA cotreatment (not shown) indicated a slight increase of PS exposure at 24 hours of culture that clearly rose at 48 hours, and necrosis was detected at day 3 with T3C1, similar to what was found with the entire TSP-1 (Figure 2C).
Induction of NB4-LR1 cell death by the C-terminal domain of TSP-1. (A) Schematic representation of TSP-1 structural and functional domains. TSP-1 is a disulfide-bonded trimeric protein composed of 3 identical subunits with a molecular mass of about 140 kDa each. Each subunit comprises multiple domains: an amino-terminal domain, a procollagen homology region (PC), 3 types of repeated sequence motifs—designated type 1 (filled diamond), type 2 (open circle), and type 3 (filled square) repeat—and a carboxy-terminal domain. The recombinant fragments used in this study are identified by their amino-terminal and carboxy-terminal amino acids (aa). VTCG, RGDA, and RFYVVMWK peptide sequences identified from TSP-1 for its respective binding to CD36, β3 integrin, and CD47 membrane receptors are indicated. (B, C) NB4-LR1 cells untreated (broken line) or treated (solid line) with ATRA (1 μM) were cultured for 4 days in the absence or the presence of increasing doses (0.5 to 5 μM) of TSP-1 recombinant fragments corresponding to the N-terminal (NTSP-1; ▴), the type 1 repeat (3TSR; ▪), or the type 3 repeat/C-terminal domain (T3C1; •) of the molecule. Cell growth of NB4-LR1 cells was expressed as percent of untreated cells growth (B), and cell death, as quantified by annexin V labeling, was expressed as percent of positive cell detection upon flow cytometry analysis (C). Results are expressed as mean ± SEM of 3 experiments. (D) Nucleus morphology of NB4-LR1 cells untreated or treated with ATRA with or without the T3C1 TSP-1 recombinant fragment (3 μM) or the entire TSP-1 (0.075 μM), as analyzed by confocal microscopy using Vectashield containing DAPI as mounting medium.
Induction of NB4-LR1 cell death by the C-terminal domain of TSP-1. (A) Schematic representation of TSP-1 structural and functional domains. TSP-1 is a disulfide-bonded trimeric protein composed of 3 identical subunits with a molecular mass of about 140 kDa each. Each subunit comprises multiple domains: an amino-terminal domain, a procollagen homology region (PC), 3 types of repeated sequence motifs—designated type 1 (filled diamond), type 2 (open circle), and type 3 (filled square) repeat—and a carboxy-terminal domain. The recombinant fragments used in this study are identified by their amino-terminal and carboxy-terminal amino acids (aa). VTCG, RGDA, and RFYVVMWK peptide sequences identified from TSP-1 for its respective binding to CD36, β3 integrin, and CD47 membrane receptors are indicated. (B, C) NB4-LR1 cells untreated (broken line) or treated (solid line) with ATRA (1 μM) were cultured for 4 days in the absence or the presence of increasing doses (0.5 to 5 μM) of TSP-1 recombinant fragments corresponding to the N-terminal (NTSP-1; ▴), the type 1 repeat (3TSR; ▪), or the type 3 repeat/C-terminal domain (T3C1; •) of the molecule. Cell growth of NB4-LR1 cells was expressed as percent of untreated cells growth (B), and cell death, as quantified by annexin V labeling, was expressed as percent of positive cell detection upon flow cytometry analysis (C). Results are expressed as mean ± SEM of 3 experiments. (D) Nucleus morphology of NB4-LR1 cells untreated or treated with ATRA with or without the T3C1 TSP-1 recombinant fragment (3 μM) or the entire TSP-1 (0.075 μM), as analyzed by confocal microscopy using Vectashield containing DAPI as mounting medium.
Finally, T3C1 treatment also induced maturation-independent cell death, as evaluated through NBT dye reduction and MGG staining assays (not shown). In addition, condensed chromatin or fragmented nuclei were not observed upon DAPI (4′,6-di-amidino-2-phenylindole) staining of the cells (Figure 3D).
Caspase-independent cell death induced by TSP-1 in NB4-LR1 cells
We next investigated the involvement of caspase activity in cell death triggered by TSP-1 by comparison with staurosporine, a well-known inducer of cell apoptosis. Experimental conditions for staurosporine treatment were chosen to induce a level of annexin V-positive NB4-LR1 cells similar to that obtained with ATRA/T3C1 treatment. Whereas staurosporine-treated cells displayed about 50-fold increase in caspase-3-like activity compared with untreated cells, ATRA/T3C1-treated cells showed no caspase-3 activity and neither did cells treated with the other TSP-1 recombinant fragments (Figure 4A). In addition, we found that the broad-spectrum caspase inhibitor z-VAD-fmk, used at a noncytotoxic dose (25 μM) that was able to inhibit both caspase activity and cell death in staurosporine-treated cells, did not prevent cell death upon ATRA/T3C1 treatment, as measured by annexin V-positive detection and microscopic cell observation (not shown). Furthermore, caspase-3 as well as caspase-8 were found to remain in precursor form (ie, not activated) when analyzed by Western blotting in ATRA/T3C1- or ATRA/TSP-1-treated NB4-LR1 cell lysates (Figure 4B). Additionally, no proteolysis of caspase substrates such as the DNA repair enzyme PARP or the antiapoptotic protein Bcl-2 was found. Finally, analysis of low-molecular-weight DNA extracted from ATRA/T3C1- or ATRA/TSP-1-treated cells showed absence of characteristic ladder pattern resulting from internucleosomal cleavage of genomic DNA (Figure 4C).
TSP-1 C-terminal domain induction of mitochondrial dysfunction with ROS production in the absence of cytochrome c and other mitochondrial intermembrane protein release
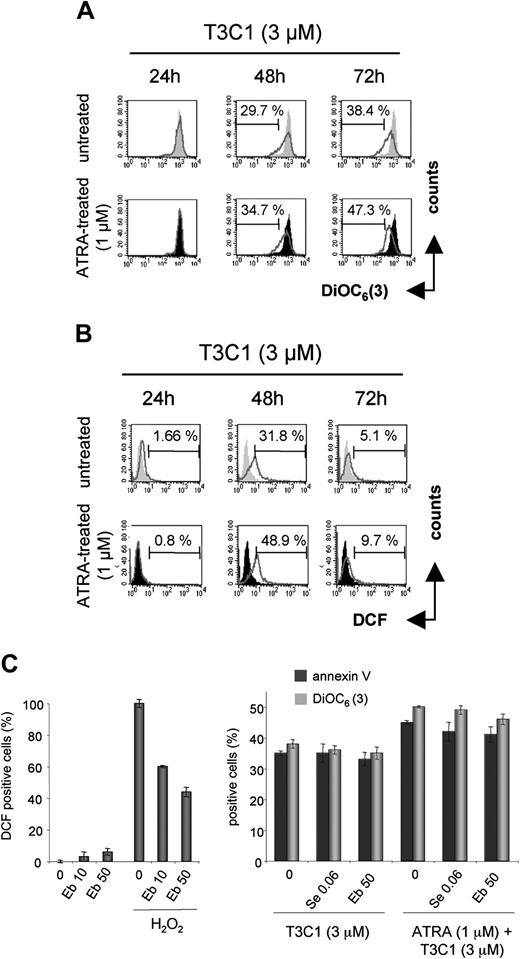
Many types of cell death are accompanied by the permeabilization of mitochondrial membrane resulting from the opening of mitochondrial pores and disruption of the mitochondrial transmembrane potentiel (ΔΨm).36 As shown in Figure 5A, kinetics analysis showed a drop in ΔΨm of T3C1- or ATRA/T3C1-treated cells that was detected at day 2 and was more pronounced at day 3. Importantly, ATRA by itself had only very slight effect on ΔΨm reduction, and staurosporine was found to induce a drop in ΔΨm similar to that detected after T3C1 treatment (not shown).
Mitochondria are the major source of ROS whose intracellular accumulation, upon ΔΨm disruption, induces cellular oxydative stress that is implicated both in apoptosis and necrosis.36,37 Intracellular ROS production upon T3C1/ATRA treatment was detected at day 2 in close correlation with loss of ΔΨm and was essentially due to the T3C1 fragment effect (Figure 5B). The lower level of ROS observed at day 3 was very likely resulting from ROS leakage due to membrane alterations. Pretreatment of the cells with selenium, known to reduce oxidative stress, or ebselen, a seleno-organic compound that converts H2O2 to H2O,43 showed no inhibitory effect, indicating that mitochondria-derived ROS were likely not involved in the cell death process induced by T3C1 (Figure 5C).
Caspase-independent cell death induced by TSP-1 in NB4-LR1 cells. NB4-LR1 cells untreated or treated with ATRA (1 μM) were cultured for 4 days with or without the NTSP-1, 3TSR, or T3C1 fragment (3 μM) or the entire purified TSP-1 (0.075 μM). NB4-LR1 cells were also treated with staurosporine (STP; 5 μM) for 3.5 hours. (A) Caspase-3-like activity was determined in cell extracts by means of a colorimetric assay of the DEVD-pNa substrate hydrolysis. NB4-LR1 cells treated with STP with or without the broad-spectrum caspase inhibitor z-VAD-fmk (25 μM) were used as positive control for the detection of caspase-3-like activity as measured by spectrophotometry. OD indicates optical density. (B) SDS cell lysates (about 10 μg proteins corresponding to 105 cells) prepared from NB4-LR1 cells were processed for Western blotting for analysis, under reducing conditions, of caspase-3 or caspase-8 activation, through cleavage of their precursor forms, cleavage analysis of the caspase substrate PARP, or the antiapoptotic protein Bcl-2. Polyclonal antibodies specific to caspase-3 or caspase-8 (1:500), monoclonal antibodies specific to PARP (1:200), or Bcl-2 (1:1000), respectively, were used. (C) Genomic DNA from NB4-LR1 cells (106) was extracted, as described in “Materials and methods,” and electrophoresed on 2% agarose gel and then analyzed upon ethidium bromide visualization.
Caspase-independent cell death induced by TSP-1 in NB4-LR1 cells. NB4-LR1 cells untreated or treated with ATRA (1 μM) were cultured for 4 days with or without the NTSP-1, 3TSR, or T3C1 fragment (3 μM) or the entire purified TSP-1 (0.075 μM). NB4-LR1 cells were also treated with staurosporine (STP; 5 μM) for 3.5 hours. (A) Caspase-3-like activity was determined in cell extracts by means of a colorimetric assay of the DEVD-pNa substrate hydrolysis. NB4-LR1 cells treated with STP with or without the broad-spectrum caspase inhibitor z-VAD-fmk (25 μM) were used as positive control for the detection of caspase-3-like activity as measured by spectrophotometry. OD indicates optical density. (B) SDS cell lysates (about 10 μg proteins corresponding to 105 cells) prepared from NB4-LR1 cells were processed for Western blotting for analysis, under reducing conditions, of caspase-3 or caspase-8 activation, through cleavage of their precursor forms, cleavage analysis of the caspase substrate PARP, or the antiapoptotic protein Bcl-2. Polyclonal antibodies specific to caspase-3 or caspase-8 (1:500), monoclonal antibodies specific to PARP (1:200), or Bcl-2 (1:1000), respectively, were used. (C) Genomic DNA from NB4-LR1 cells (106) was extracted, as described in “Materials and methods,” and electrophoresed on 2% agarose gel and then analyzed upon ethidium bromide visualization.
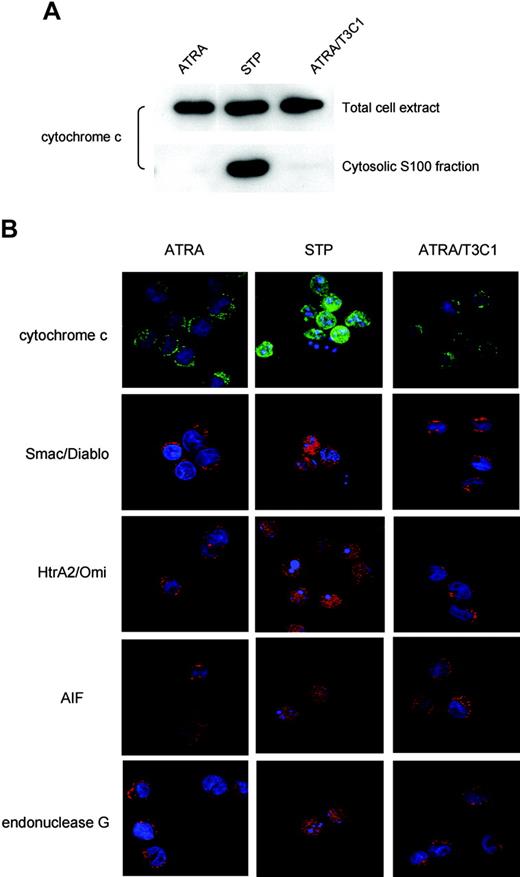
We then examined whether cytochrome c was released from mitochondria, whose release process is independent of caspase activity and needs outer membrane permeabilization without mitochondrial depolarization.44 Whereas cytosolic accumulation of cytochrome c was clearly detected in staurosporine-treated NB4-LR1 cells through subcellular analysis, it was undetected in T3C1-treated cells (Figure 6A). Supporting this finding, immunofluorescence analysis indicated no change in cytochrome c subcellular localization after T3C1/ATRA treatment, as illustrated in Figure 6B, whereas staurosporine treatment clearly induced change in subcellular distribution. Mitochondrial release of other soluble intermembrane proteins that occurs upon ΔΨm loss and contributes to both caspase-independent (endonuclease G, AIF, Omi/HtrA2) or caspase-dependent (Smac-DIABLO) cell death processes45,46 was also examined by immunofluorescence (Figure 6B). Collectively, these data indicated no mitochondrial release upon T3C1 action.
CD47 and αvβ3 integrin receptors mediate cell death induced by the TSP-1 C-terminal domain
Given that the T3C1 recombinant fragment contains both TSP-1 binding sequences to CD47 and αvβ3 receptors (Figure 3A),8 involvement of these receptors in the death responses of NB4-LR1 cells to T3C1 was next examined.
At first, immunofluorescence experiments were performed that showed colocalization of αvβ3 with CD47 in the membrane of untreated or ATRA-treated NB4-LR1 cells, as illustrated in Figure 7Aa for ATRA-treated cells. Moreover, when treated for 48 hours with the T3C1 fragment, untreated cells (not shown) or ATRA-treated cells displayed colocalization of T3C1 with CD47 (Figure 7Ab) or αvβ3 (Figure 7Ac). Of note was the absence of TSP-1 signal when cells were not treated with T3C1 (not shown).
Further experiments were carried out using the CD47 agonist peptide RFYVVMWK (4N1-1) from the C-terminal domain of TSP-1 47 and the GRGDS peptide mimetic for the αvβ3-binding activity of the RGDA sequence identified from type 3 repeat domain of TSP-1.30 The VTCG peptide corresponding to a binding sequence of TSP-1 for CD36 was used as peptide control. The VTCG sequence is not present in the T3C1 fragment, and CD36 is not expressed in NB4 cells (Figures 1D and 3A). The 4N1-1, GRGDS, and VTCG peptides alone were not found to have death induction effect on either untreated or ATRA-treated NB4-LR1 cells through cell microscopic observation and PS positive detection (not shown). In addition, none of the peptides displayed significant cell growth inhibitory effect. When tested for their ability to interfere with the effect of T3C1 by itself or combined with ATRA, the 4N1-1 and GRGDS peptides were found to exert dose-dependent inhibitory action on cell killing, as quantified by annexin V cell staining at day 4. The GRGDS peptide showed a stronger action than 4N1-1, while the VTCG control peptide had no significant effect. When added together, the 4N1-1 and GRGDS peptides showed a greater inhibitory effect that was found to be unchanged by ATRA treatment (Figure 7B). Furthermore, combinatorial effect of these 2 peptides measured at day 2 indicated substantial inhibition of NB4-LR1 cell death induced by T3C1, as defined by PS exposure, inhibition of ΔΨm disruption, and ROS production (Figure 7C).
Discussion
In this study, the APL cell line NB4-LR1, resistant to maturation by ATRA,28,29 was used to investigate whether TSP-1 plays a role in the maturation/apoptotic program triggered by ATRA. Indeed, in contrast to the features of the parental NB4 cell line, this subcloned cell line expressed no endogenous TSP-1 in response to ATRA but constitutively expressed potential membrane receptors for the matrix protein. Therefore, it constituted an appropriate cell model to check whether TSP-1 membrane signaling acts to trigger antitumor responses. We show here that membrane signals by TSP-1 induce strong inhibition of cell growth and caspase-independent cell death in APL that is not subsequent to cell maturation. Cell death is characterized by an atypical mitochondrial dysfunction and is mediated by ligation of the TSP-1 membrane receptors CD47 and αvβ3.
Of note, the reduction of tumor cell growth in vivo by TSP-1 is a well-documented consequence of its inhibitory effect on tumor angiogenesis by acting on endothelial cell proliferation and apoptosis and/or by activating TGF-β.11-13,15,31 Indeed, activated TGF-β has been shown to inhibit tumor cell growth and induce tumor cell apoptosis. These activities are increased by TSP-1 and mediated by specific sequences present in the type 1 repeat domain of TSP-1.11,31 Importantly, in this report, we show that TGF-β did not induce NB4-LR1 cell death. Furthermore, we gained evidence that TSP-1 action on NB4-LR1 cells was mapped to its C-terminal domain, which does not contain activation sequence for TGF-β.
Alteration of the mitochondrial transmembrane potential and ROS production induced by the C-terminal domain of TSP-1. (A, B) NB4-LR1 cells untreated (gray shaded curves) or treated with ATRA (1 μM; filled curves) were cultured for 3 days without or with the TSP-1 T3C1 recombinant fragment (3 μM; open curve). At each day of the treatment, cells were stained with the lipophilic fluorochrome DiOC6(3) (A) or the oxidant-sensitive dye DCFH-DA (B), as described in “Materials and methods,” and then analyzed by flow cytometry. Percentage of positive cells are indicated. (C, left) Cells were preincubated for 2 hours with noncytotoxic doses of ebselen (Eb; 10 μM and 50 μM) and then treated or not with H2O2 (50 μM; 6 hours) for detection of ROS production upon cell staining with DCFH-DA. (Right) Untreated or ATRA-treated (1 μM) cells were cultured for 3 days with T3C1 without or with selenium (Se; 0.06 μM) or ebselen (Eb; 50 μM), and cell death, as quantified by annexin V and DiOC6(3) staining, was analyzed at day 3. Results are expressed as mean ± SEM of 2 experiments.
Alteration of the mitochondrial transmembrane potential and ROS production induced by the C-terminal domain of TSP-1. (A, B) NB4-LR1 cells untreated (gray shaded curves) or treated with ATRA (1 μM; filled curves) were cultured for 3 days without or with the TSP-1 T3C1 recombinant fragment (3 μM; open curve). At each day of the treatment, cells were stained with the lipophilic fluorochrome DiOC6(3) (A) or the oxidant-sensitive dye DCFH-DA (B), as described in “Materials and methods,” and then analyzed by flow cytometry. Percentage of positive cells are indicated. (C, left) Cells were preincubated for 2 hours with noncytotoxic doses of ebselen (Eb; 10 μM and 50 μM) and then treated or not with H2O2 (50 μM; 6 hours) for detection of ROS production upon cell staining with DCFH-DA. (Right) Untreated or ATRA-treated (1 μM) cells were cultured for 3 days with T3C1 without or with selenium (Se; 0.06 μM) or ebselen (Eb; 50 μM), and cell death, as quantified by annexin V and DiOC6(3) staining, was analyzed at day 3. Results are expressed as mean ± SEM of 2 experiments.
Antitumor effects of TSP-1 were mapped to its type 3 repeat/C-terminal domain using recombinant fragments of the protein. The T3C1 recombinant domain was less active than the intact protein (ie, about 40 times less at the respective doses of 3 μM for T3C1 and 0.075 μM for TSP-1). Interestingly, this was also observed in a study by Miao et al31 on the tumor growth inhibitory function of the TSP-1 type 1 repeat recombinant protein. This may mean that the 2 distinct antitumor domains identified independently by us and by Miao et al each cooperate with another domain of the native TSP-1 that plays an enhancer role. Alternatively, these data may mean that the effects of these domains are partly dependent upon the trimer structure of the TSP-1 molecule that cannot be achieved by the recombinant fragments. In keeping with this notion, although substantial growth inhibition was induced by either the entire TSP-1 or the T3C1 recombinant fragment at low concentration, only high doses could induce cell death based on morphologic or biochemical criteria (Figures 2 and 3). This could indicate that in the leukemic NB4-LR1 cell model, TSP-1 exerts dual effects relevant to differential or composite membrane signals. Further studies are needed to determine whether TSP-1 signals for inhibition of cell proliferation could occur independently of its action leading to cell death.
Absence of mitochondrial intermembrane protein release upon NB4-LR1 cell treatment with the C-terminal domain of TSP-1. NB4-LR1 cells were either treated with ATRA (1 μM) for 3 days without or with the T3C1 recombinant fragment (3 μM) or treated with staurosporine (STP; 5 μM) for 3.5 hours. (A) Western blot analysis, under reducing conditions, of total cell extract and cytosolic S100 fraction prepared from 5 × 106 cells, as described in “Materials and methods,” for detection of cytochrome c, using monoclonal antibody (1:100), in the respective fraction each corresponding to 105 cells. (B) Immunofluorescence analysis of mitochondria protein in NB4-LR1 cells. Upon fixation by 2% PFA and permeabilization with 0.1% saponin, as described in the “Materials and methods,” cells were incubated with antibodies to cytochrome c (1:200), AIF (1:500), Smac/DIABLO (1:150), Omi/HtrA2 (1:150), or endonuclease G (6 μg/mL). Alexa Fluor 594-conjugated anti-rabbit IgG and Alexa Fluor 488-conjugated anti-mouse IgG were used as secondary antibodies. Vectashield containing DAPI for nucleus staining was used as mounting medium for confocal microscopy analysis.
Absence of mitochondrial intermembrane protein release upon NB4-LR1 cell treatment with the C-terminal domain of TSP-1. NB4-LR1 cells were either treated with ATRA (1 μM) for 3 days without or with the T3C1 recombinant fragment (3 μM) or treated with staurosporine (STP; 5 μM) for 3.5 hours. (A) Western blot analysis, under reducing conditions, of total cell extract and cytosolic S100 fraction prepared from 5 × 106 cells, as described in “Materials and methods,” for detection of cytochrome c, using monoclonal antibody (1:100), in the respective fraction each corresponding to 105 cells. (B) Immunofluorescence analysis of mitochondria protein in NB4-LR1 cells. Upon fixation by 2% PFA and permeabilization with 0.1% saponin, as described in the “Materials and methods,” cells were incubated with antibodies to cytochrome c (1:200), AIF (1:500), Smac/DIABLO (1:150), Omi/HtrA2 (1:150), or endonuclease G (6 μg/mL). Alexa Fluor 594-conjugated anti-rabbit IgG and Alexa Fluor 488-conjugated anti-mouse IgG were used as secondary antibodies. Vectashield containing DAPI for nucleus staining was used as mounting medium for confocal microscopy analysis.
Involvement of CD47 and αvβ3 integrin receptors in mediating cell death induced by the C-terminal domain of TSP-1. (A) NB4-LR1 cells were treated with ATRA (1 μM) for 2 days without or with the T3C1 recombinant fragment (3 μM) and then fixed by the addition of 2% PFA. (i) Cells cultured without T3C1 were successively incubated with mouse monoclonal antibody to CD47 (20 μg/mL) and polyclonal antiserum to the αv integrin subunit (1:50). (ii, iii) ATRA-treated cells cultured with the T3C1 fragment were successively incubated with rabbit antiserum to TSP-1 (R1; 1:50) and mouse monoclonal antibody to αv or CD47 (20 μg/mL). Alexa Fluor 594-conjugated anti-rabbit IgG and Alexa Fluor 488-conjugated anti-mouse IgG were used as secondary antibodies. Vectashield containing DAPI for nucleus staining was used as mounting medium for confocal microscopy analysis. Yellow color in the merge confocal images indicates the superimposition of the 2 fluorochromes. (B, C) NB4-LR1 cells, untreated or treated with ATRA (1 μM), were incubated for 2 hours with 4N1-1 (25 to 200 μM), GRGDS (0.1 to 1 mM), 4N1-1 (100 μM), and GRGDS (100 μM) or the VTCG (1 mM) peptide control and then cultured for 4 days (B) or 2 days (C) with the T3C1 recombinant fragment (3 μM). (B) At 4 days of the treatment, cell death was quantified by annexin V labeling and expressed as percent of positive cell detection upon flow cytometry analysis. Results are expressed as mean ± SEM of 3 experiments. (C) At 2 days of the treatment, cell death induction was monitored by annexin V (top), DiOC6(3) (middle), or DCFH-DA (bottom) staining for detection of PS membrane outside exposure, mitochondrial transmembrane potential alteration, and ROS production, respectively. Results are expressed as mean ± SEM of 2 experiments.
Involvement of CD47 and αvβ3 integrin receptors in mediating cell death induced by the C-terminal domain of TSP-1. (A) NB4-LR1 cells were treated with ATRA (1 μM) for 2 days without or with the T3C1 recombinant fragment (3 μM) and then fixed by the addition of 2% PFA. (i) Cells cultured without T3C1 were successively incubated with mouse monoclonal antibody to CD47 (20 μg/mL) and polyclonal antiserum to the αv integrin subunit (1:50). (ii, iii) ATRA-treated cells cultured with the T3C1 fragment were successively incubated with rabbit antiserum to TSP-1 (R1; 1:50) and mouse monoclonal antibody to αv or CD47 (20 μg/mL). Alexa Fluor 594-conjugated anti-rabbit IgG and Alexa Fluor 488-conjugated anti-mouse IgG were used as secondary antibodies. Vectashield containing DAPI for nucleus staining was used as mounting medium for confocal microscopy analysis. Yellow color in the merge confocal images indicates the superimposition of the 2 fluorochromes. (B, C) NB4-LR1 cells, untreated or treated with ATRA (1 μM), were incubated for 2 hours with 4N1-1 (25 to 200 μM), GRGDS (0.1 to 1 mM), 4N1-1 (100 μM), and GRGDS (100 μM) or the VTCG (1 mM) peptide control and then cultured for 4 days (B) or 2 days (C) with the T3C1 recombinant fragment (3 μM). (B) At 4 days of the treatment, cell death was quantified by annexin V labeling and expressed as percent of positive cell detection upon flow cytometry analysis. Results are expressed as mean ± SEM of 3 experiments. (C) At 2 days of the treatment, cell death induction was monitored by annexin V (top), DiOC6(3) (middle), or DCFH-DA (bottom) staining for detection of PS membrane outside exposure, mitochondrial transmembrane potential alteration, and ROS production, respectively. Results are expressed as mean ± SEM of 2 experiments.
Cell death, as induced by the soluble form of T3C1 in NB4-LR1, is representative of a new form of caspase-independent death pathway, being similar to that recently described in B-cell chronic lymphocytic leukemia or normal B cells19 and cytotoxic T or breast cancer cells20,21,48 upon exposure to CD47 agonists. In the latter case, death triggered by TSP-1, RFYVVM peptide, or monoclonal antibodies to CD47 is accompanied with PS membrane outside exposure and loss of mitochondrial transmembrane potential (ΔΨm), which are typical of cell apoptosis, but not by cytochrome c or AIF release or DNA fragmentation. However, at variance with our results in NB4-LR1 cells, cell death rapidly proceeded, within 18 hours, and no plasma membrane breakdown was observed.19,49 Importantly, antibodies to CD47 or RFYVVM peptide were either more potent than TSP-1 in inducing cell death21,49 or were effective only in immobilized form.19,20 We therefore used the antibody to CD47 B6H12 or the RFYVVM 4N1K peptide, as used in these studies, and found them to have no death induction effect on NB4-LR1 cells when used either in soluble or immobilized form (A.S. and V.D., unpublished data, April 2003). These apparently contradictory findings would mean that other epitopes on CD47 were active in NB4-LR1 because, in fact, not all the CD47 agonists were able to activate cell death.48 Alternatively, this could be relevant to death signals by T3C1 that required CD47/αvβ3 integrin double signaling in NB4-LR1 leukemic cells to take effect. In this regard, NB4-LR1 cell death triggered by this domain of TSP-1 was not inhibited or delayed when cells were treated with a cAMP analog (A.S., M.B.S., and V.D., unpublished data, October 2003), indicating that TSP-1 action does not involve regulation of cAMP intracellular level and subsequent signal effects, as has been reported for CD47-dependent killing of cytotoxic T or breast cancer cells.21
The mitochondrial dysfunction induced by action of the C-terminal domain of TSP-1 on NB4-LR1 did not lead to cytochrome c or AIF release, as shown in other studies reporting on death effects by CD47 agonists.20,21 We extended these studies to other death-promoting factors and found no release of endonuclease G and Omi/HtrA2 or of Smac-DIABLO. Absence of AIF or endonuclease G leakage is consistent with the absence of chromatin condensation and nuclear fragmentation (Figure 3D).45,46 On the other hand, ROSs, which function as second messengers and regulating molecules for cell death, were shown increased in cells.37 However, through use of ROS scavenger or oxidative stress inhibitor, we did not find ROS to be involved in cell damage. This result could be related to the absence of cytochrome c release, which preserves normal redox state,36,37 so that only moderate levels of ROS are produced. It remains to be determined whether a mitochondrial dysfunction featured by a partial (or differential) membrane permeabilization defect could be one rate-limiting step of this TSP-1-dependent cell death.
Finally, many forms of caspase-independent programmed cell death are mediated by other proteases such as cathepsins, calpains, and serine proteases that can cleave at least some of the caspase substrates.38,50,51 However, this alternative cell death pathway generally produces mitochondrial intermembrane protein leakage and leads to incomplete chromatin condensation.52-55 We investigated the involvement of calpain activity because among numerous calpain substrates are cytoskeletal and membrane-associated proteins suggesting that calpains are important in destruction of cellular architecture.53,56 However, no inhibitory effect was exerted by the calpain inhibitors PD150606 and calpeptin on NB4-LR1 cell death induction by the T3C1 (A.S. and V.D., unpublished data, September 2003).
This is the first report showing the ability of soluble source of the matrix protein TSP-1 to trigger a novel noncaspase cell death pathway in ATRA-resistant APL. This activity is mapped to the type 3 repeat/C-terminal domain of the molecule. Cell death is mediated by the TSP-1 membrane receptors CD47 and the αvβ3 integrin and is accompanied by ΔΨm collapse that does not result in the release of well-known death-promoting proteins, such as the noncaspase apoptosis regulators AIF, endonuclease G, or Omi/HtrA2. This kind of cell death may resemble in some way necrosis-like programmed cell death in which increased PS membrane exposure is detected in the absence of chromatin condensation and occurs before cell damage.50 However, the level of necrosis is low and not consistent with the apparent substantial cell damage, suggesting it could not be a major event, and cell death might actually be related to an alternative, unidentified process.
Retinoids have important physiological functions in regulating cell growth, differentiation, and death.57 Upon its induction and secretion following ATRA treatment, TSP-1 could mediate growth inhibition and death responses. Therefore, TSP-1 signaling could well contribute to the therapeutic response of APL cells to retinoids. A pharmacologic ligation of TSP-1 receptors on cells for which ATRA-dependent TSP-1 induction is deficient could be envisioned. Alternatively, identification of the molecular targets of TSP-1 signaling (receptors, signal transduction enzymes) the most appropriate to a pharmacologic exploitation will need specific investigation. Mediators of cell death program execution are under current investigation, and their identification would contribute to elaborate new targets in the field of cancer, especially to sensitize tumor cells to death and to overcome resistance to drug therapy.
Prepublished online as Blood First Edition Paper, March 22, 2005; DOI 10.1182/blood-2004-09-3585.
Supported by INSERM, the Association Claude Bernard, Fondation pour la Recherche Médicale, Association pour la Recherche contre le Cancer, Ligue Nationale Contre le Cancer, and National Institutes of Health grants HL68003 and CA92644.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
The authors are most grateful to Dr Santos Susin and Marlène Bras for their help in immunofluorescence analysis of mitochondria. The authors also thank Mark Duquette and Eric Galardi for expert technical assistance and Dr Evelyne Segal-Bendirdjian for her critical reading of the manuscript.