Abstract
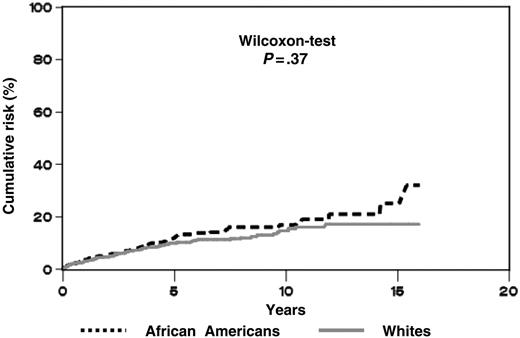
The age-adjusted incidence of multiple myeloma (MM) is 2-fold higher in African Americans than in whites. A few small studies have reported a higher prevalence of monoclonal gammopathy of undetermined significance (MGUS) in African Americans versus whites. Etiologic factors for MGUS and determinants for transformation of MGUS to MM are unknown. We quantified the prevalence of MGUS and subsequent risk of MM among 4 million African American and white male veterans admitted to Veterans Affairs (VA) hospitals. The age-adjusted prevalence ratio of MGUS in African Americans compared with whites was 3.0 (2.7-3.3 95% confidence interval). Among 2046 MGUS cases, the estimated cumulative risk of MM during the first 10 years of follow-up was similar (P = .37) for African Americans (17%) and whites (15%). In the largest study to date, we suggest that the excess risk of MM in African Americans results from an increase in risk of MGUS rather than an increased risk of progression from MGUS to MM.
Introduction
Multiple myeloma (MM) is a B-cell malignancy morphologically characterized by a monoclonal proliferation of plasma cells in the bone marrow. In contrast with the white predominance of most hematopoietic neoplasms, age-adjusted incidence of MM is 2-fold higher in African Americans (9.5 per 100 000 per year) than in whites (4.1 per 100 000 per year).1 The basis for this race-related difference is unknown.
Monoclonal gammopathy of undetermined significance (MGUS), a benign disorder with a strikingly elevated monoclonal immunoglobulin level of less than 30 g/L in individuals lacking evidence of MM or other lymphoproliferative malignancies, often precedes MM. A screening study conducted in the 1960s in Sweden demonstrated MGUS prevalence of 0.1% to 0.2% in persons aged 30 to 49 years, 1.1% to 2.0% in those aged 50 to 79 years, and 5.7% in those aged 80 to 89 years.2 Long-term follow-up of patients with MGUS reveals a 1% to 3% annual risk of developing MM or, to a lesser extent, other lymphoproliferative malignancies.3 Although investigators have recently described potential models of pathogenesis of MGUS and MM, it is unknown whether MGUS precedes all cases of MM or if MM can arise de novo without preceding MGUS.4,5
Etiologic factors for MGUS and determinants for transformation of MGUS to MM are unknown, but data on the prevalence and progression of MGUS and MM according to race may provide clues to etiology. For example, if the prevalence ratio for MGUS parallels the incidence ratio for MM according to race and the probability of progression to MM is the same in both races, then better understanding of the exogenous and genetic risk factors for MGUS would be a priority in order to explain the racial disparity. If however the racial differences result from a more rapid rate of progression from MGUS to MM in African Americans compared with whites, the focus would move to factors that influence progression. A few small studies have reported a higher prevalence of MGUS in African Americans compared with whites.6-8 The objective of the present study was to quantify and compare the prevalence of MGUS and risk of MM following MGUS among African Americans and whites using data from the largest study to date.
Study design
Hospitals, patients, and outcomes
The cohort was identified from discharge records for inpatient hospitalizations at 142 nationwide United States Veterans Affairs (VA) hospitals between October 1, 1980, and September 30, 1996. The target population for calculation of MGUS prevalence included all African American (n = 749 020) and white (n = 3 248 795) veterans hospitalized at least once at age 18 or older. MGUS cases were patients from the eligible population with an ICD-9 (International Classification of Diseases, Ninth Revision) discharge diagnosis of 273.1 (Table 1). For estimating risk of malignancy, all subjects without a prior discharge diagnosis of malignancy were followed from one year after index hospital discharge (MGUS diagnosis for MGUS cases and first discharge for any reason for all others) until the diagnosis of a first malignancy, death, or the end of the observation period (September 30, 1996), whichever came first. Dates of death were ascertained from record linkage to Social Security Administration mortality files. The length of the time period for progression to MM was estimated by subtracting the date of discharge for the first hospitalization listing a discharge diagnosis of MGUS from the date of discharge for the first hospitalization listing a discharge diagnosis of MM. Approval was obtained from the National Institutes of Health (NIH) institutional review board for these studies. Informed consent was waived because we had no contact with study subjects.
Statistical methods
Age-adjusted prevalence rates were directly standardized to the year 2000 United States standard population. Using the Kaplan-Meier procedure, we calculated the cumulative probability of developing MM among MGUS cases according to race, testing for statistical significance using the Wilcoxon test appropriate for censored data. The Cox proportional hazards model was applied. Poisson regression was used for analyses comparing risk for MM among MGUS versus non-MGUS cohorts.
Results and discussion
Age-adjusted prevalence rates for MGUS
We identified 734 cases of MGUS in African Americans and 1312 in whites (Table 1). The age-adjusted prevalence rate for MGUS was 3.0-fold (2.7-3.3 95% confidence interval [CI]) higher in African Americans than in whites.
Risk of multiple myeloma subsequent to MGUS
Among MGUS cases, the estimated cumulative risk of developing MM during the first 10 years of follow-up was similar (Wilcoxon test P = .37) for African Americans (17%) and whites (15%; Figure 1). The relative risk (RR) of MM for African Americans (relative to whites) was 1.22 (0.91-1.65, 95% CI); the estimate did not change during each quartile of the study period and was similar for each age group at MGUS diagnosis. As expected, the risk of developing MM among all MGUS (versus other than MGUS) cases was very high (RR = 89.1; 74.7-106.3, 95% CI).
An increased prevalence of MGUS in African Americans (vs whites) has been reported in 3 previous studies of 44 (Singh et al6 ), 86 (Schechter et al7 ), and 106 (Cohen et al8 ) MGUS cases, respectively. The strength of the current study includes its substantially larger size (n = 2046) in a patient population with relatively stable and standardized access to medical care, which is provided to United States veterans independent of socioeconomic status. In addition, patients were followed for intervals as long as 16 years subsequent to MGUS. Limitations include the lack of information about demographic, clinical, laboratory, or biomarker information for individual patients in the database. Identification of the cohort from discharge diagnoses, rather than from screening, is likely to have led to underascertainment of MGUS in the hospitalized population studied. Because MGUS is generally asymptomatic, it is not surprising that the prevalence in the United States VA hospitals is lower than the prevalence of MGUS reported from screening studies.2 It is also likely that patients of both races with specific medical conditions (such as inflammatory disorders and liver disease) or African Americans with certain symptoms occurring in MM (such as severe low back pain, severe bone pain, and/or repeated infections) but no diagnosis of MM may be more likely to undergo testing with serum protein electrophoresis. The use of a retrospective cohort rather than a prospective cohort study design could have potentially caused underascertainment of MM cases; however, the observed rates of 17% and 15% at 10 years are very similar to reported rates from the Mayo clinic,3 suggesting that most MM cases were identified in this study.
Cumulative risk of a subsequent diagnosis of multiple myeloma in the absence of other causes of death among African American (n = 734) and white (n = 1312) United States veterans with a previous history of MGUS. The cumulative risk was computed as 1.00 minus the Kaplan-Meier estimate.
Cumulative risk of a subsequent diagnosis of multiple myeloma in the absence of other causes of death among African American (n = 734) and white (n = 1312) United States veterans with a previous history of MGUS. The cumulative risk was computed as 1.00 minus the Kaplan-Meier estimate.
Our finding of a 3-fold higher prevalence of MGUS in African Americans than in whites, along with a similar cumulative probability of MM occurring subsequent to MGUS in both races, suggests that identification of etiologic factors of MGUS may be key to understanding factors that contribute to the racial disparity for MM. We conclude that the focus of epidemiologic research on MM should be shifted to studies examining postulated risk factors for MGUS in order to understand the etiology of MM.
Prepublished online as Blood First Edition Paper, October 6, 2005; DOI 10.1182/blood-2005-08-3449.
Supported by the Intramural Research Program of the National Institutes of Health (NIH), National Cancer Institute (NCI).
O.L. and G.G. designed the study and obtained data; O.L., G.G., and T.R.F. analyzed data; all authors were involved in the interpretation of the results; and O.L. initiated this work and wrote the report. All authors read, gave comments, and approved the final version of the manuscript. O.L., G.G., and T.R.F. had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
The authors thank the Medical Administration Service of the Veterans Health Services and Research Administration, which provided the data on which this study is based, and Ms Heather Morris (Information Management Services, Silver Spring, MD) for assistance with data preparation.