In contrast to human immunodeficiency virus (HIV)-infected humans, natural hosts for simian immunodeficiency virus (SIV) very rarely progress to acquired immunodeficiency syndrome (AIDS). While the mechanisms underlying this disease resistance are still poorly understood, a consistent feature of natural SIV infection is the absence of the generalized immune activation associated with HIV infection. To investigate the immunologic mechanisms underlying the absence of AIDS in SIV-infected sooty mangabeys (SMs), a natural host species, we performed a detailed analysis of the SIV-specific cellular immune responses in 110 SIV-infected SMs. We found that while SIV-specific T-cell responses are detectable in the majority of animals, their magnitude and breadth are, in fact, lower than what has been described in HIV-infected humans, both in terms of cytokine production (ie, IFN-γ, TNF-α, and IL-2) and degranulation (ie, CD107a expression). Of importance, SIV-specific T-cell responses were similarly low when either SIVmac239-derived peptides or autologous SIVsmm peptides were used as stimuli. No correlation was found between SIV-specific T-cell responses and either viral load or CD4+ T-cell count, or between these responses and markers of T-cell activation and proliferation. These findings indicate that the absence of AIDS in naturally SIV-infected sooty mangabeys is independent of a strong cellular immune response to the virus. (Blood. 2006;108:209-217)
Introduction
The acquired immunodeficiency syndrome (AIDS) pandemic originated from zoonotic transmission of simian immunodeficiency viruses (SIVs) from infected African monkey species to humans.1 Of the natural SIV hosts, sooty mangabeys (Cercocebus atys, SMs) are of interest for 2 main reasons. First, SIVsmm, the virus infecting SMs, is the origin of the human immunodeficiency virus 2 (HIV-2) epidemic in humans.1-3 Second, SIVsmm is the source of the prototype SIVmac strains (ie, SIVmac239, SIVmac251) that induce an AIDS-like disease in the rhesus macaque (RM), a nonnatural host for SIV, and consequently are widely used for studies of AIDS pathogenesis and vaccines.2,4-6 SIVsmm and HIV-1/2 share many features in terms of life cycle and molecular structure, and the extent of virus replication is similarly high in naturally SIV-infected SMs and HIV-infected humans.7-9 However, the outcome of these infections is strikingly different. The vast majority of HIV-infected humans, unless treated chronically with antiretroviral therapy (ART), will develop progressive CD4+ T-cell depletion and eventually succumb to AIDS. In contrast, the vast majority of naturally SIV-infected SMs maintain normal CD4+ T-cell counts and live an apparently normal lifespan in captivity,7-9 with only one report of classic AIDS to date.10 It is important to note that the disease resistance of naturally SIV-infected SMs that show high levels of SIV viremia is substantially different from that of a rare subset of HIV-infected individuals defined as long-term nonprogressors, in whom viral replication is usually very low or undetectable.11-13 The mechanisms underlying the lack of disease progression in naturally SIV-infected SMs are still largely unknown. However, it is believed that a clear understanding of why CD4+ T-cell-tropic lentiviral infections are nonpathogenic in natural hosts may provide insight into the mechanisms of AIDS pathogenesis in HIV-infected patients.14,15
In previous work,9 we showed that SIV-infected SMs and HIV-infected individuals differ significantly in that the former do not manifest the chronic generalized immune activation that is associated with HIV replication in humans and that predicts progression to AIDS.9,16-18 We thus proposed that the limited immune activation in SIV-infected SMs is a mechanism that favors the preservation of CD4+ T-cell homeostasis.9 While chronic T-cell activation may favor disease progression in HIV-infected individuals, a number of observations provide evidence that CD8+ T-cell-mediated immune responses to HIV/SIV also play a role in controlling disease progression. First, the postpeak decline of viremia in acute HIV infection is coincident with the expansion of HIV-specific T cells.19,20 Second, during acute and chronic infection, immunologic pressure mediated by SIV/HIV-specific CD8+ T cells is manifested by viral escape mutations.21-27 Third, the depletion of CD8+ T cells in SIV-infected RMs leads to increased virus replication and rapid disease progression.28-31 Ultimately, however, these CD8+ T-cell responses to HIV/SIV fail to control viral replication and disease progression.
When it became apparent that naturally SIV-infected SMs do not develop AIDS, one hypothesis put forth was that these animals avoid disease by exerting enhanced cellular immune responses to SIV. The main theoretic problem with this hypothesis is that an effective cellular immune response would be predicted to result in low levels of viremia. It should be noted, however, that while the high viremia in SIV-infected SMs clearly indicates incomplete immune control (as seen in HIV-infected humans), it is still possible that the level of virus replication would be even higher in absence of cytotoxic T lymphocyte (CTL) responses, and that this partial control may be somehow critical in avoiding disease progression.
In this study, we sought to determine the relationship between levels of SIV-specific T-cell responses and markers of disease progression in naturally SIV-infected SMs. To this end, we measured the magnitude and breadth of SIV-specific T-cell responses in 110 naturally SIV-infected SMs belonging to the colony of the Yerkes National Primate Research Center of Emory University (Atlanta, GA). This study is, to the best of our knowledge, the largest of its nature ever performed in a natural host for SIV infection, and, in fact, the first systematic analysis of SIV-specific responses in natural hosts using state-of-the-art immunologic assays. We found that natural SIV infection of SMs is associated with low levels of SIV-specific cellular immune responses whose magnitude and breadth do not correlate with either control of viral replication or maintenance of T-cell homeostasis. We conclude that the AIDS resistance of naturally SIV-infected SMs is independent of cellular immunity to the virus.
Materials and methods
Animals
Thirty uninfected SMs and 110 naturally SIV-infected SMs were used in this study. All SMs were housed at the Yerkes National Primate Research Center and maintained in accordance with NIH guidelines. In uninfected animals, negative SIV-polymerase chain reaction (PCR) of plasma and negative HIV-2 serology confirmed the absence of SIV infection. Eight experimentally SIV-infected rhesus macaques (Macaca mulatta, RMs), 6 of which were infected with uncloned SIVsm derived from the plasma of naturally SIV-infected SMs and 2 of which were infected with SIVsm-E660, were also tested. All RMs were tested during the chronic phase of the infection. These studies were approved by the Emory University Institutional Animal Care and Use Committee.
Determination of plasma viral RNA
Quantitative real-time reverse-transcriptase (RT)-PCR assay to determine SIV viral load was performed as described in Silvestri et al.9
Lymphocyte studies and flow cytometry
Four-color flow cytometric analysis was performed in whole-blood samples using human monoclonal antibodies that were found to cross-react with SMs. The antibodies used were as follows: anti-CD4-PE (clone SK3), anti-CD4-APC (clone SK3), anti-CD8-APC (clone SK1), anti-CD25-PE (clone 2A3), and anti-CD28-PE (clone L293; all from Becton Dickinson, San Jose, CA); Ki67-FITC (clone B56), anti-CD3-PE (clone SP34-2), anti-CD69-CyChrome (clone FN50), anti-CD95-CyChrome (clone DX2), anti-HLA-DR-CyChrome (clone G46-6), anti-interferon-γ (IFN-γ)-APC (clone B27), anti-tumor necrosis factor-α (TNF-α)-PE (clone MAB11), and anti-interleukin-2 (IL-2)-PE (clone MQI-17H12; all from BD-Pharmingen, San Diego, CA); and anti-CCR7 (clone 3D12; from Beckman Coulter, Fullerton, CA). Seven color experiments were stained with anti-IFN-γ FITC (clone B27), anti-CD107a PE (clone H4A3), anti-CD4 PerCP-Cy5.5 (clone L200), anti-CD69 PE-Cy7 (clone FN50), anti-IL-2 APC (clone MQI-17H12), anti-CD3 Alexa 700 (clone SP34), and anti-CD8 Pacific Blue (clone RPA-T8; all from Becton Dickinson). Samples stained for Ki67 were surface stained first with the appropriate antibodies, then fixed and permeabilized using the BD-Pharmingen CytoFix/Perm-Kit and stained intracellularly with anti-Ki67. Four-color flow cytometric acquisition was performed on at least 100 000 events on a FACScaliber cytometer driven by the CellQuest software package (Becton Dickinson), and 7-color acquisition was performed on an LSR-II driven by the FACS DiVa software (Becton Dickinson). Analysis of the acquired data was performed using FlowJo software (TreeStar, Ashland, OR).
Intracellular cytokine staining and T-cell degranulation in response to SIV peptides
SIV-specific T-cell responses were measured in naturally SIV-infected SMs by intracellular cytokine staining for IFN-γ, TNF-α, and IL-2 in response to pools of 15-mer peptides overlapping by 11 amino acids and spanning the entire sequence of the 4 major antigenic proteins of SIVmac239 (Gag, Pol, Env, Nef). Complete peptide sets for SIVmac239 were obtained from the NIH AIDS Research & Reference Reagent Program. The number of peptides per pool was as follows: Gag (3 pools of 41 peptides); Env (2 pools of 54 peptides and 2 pools of 55 peptides); Pol (2 pools of 52 peptides and 3 pools of 53 peptides); and Nef (1 pool of 64 peptides). Optimization of our intracellular cytokine staining (ICS) assay in SMs was performed in a series of preliminary experiments that indicated that (1) the level of measured responses was not significantly affected by freezing and thawing of cells; (2) the optimal length of the stimulation was for 6 hours; (3) the optimal peptide concentration was 2 to 5 μg/mL; and (4) the intra-assay variability was consistently less than 10%, and the interassay variability was consistently less than 20%.
SM peripheral-blood mononuclear cells (PBMCs) were isolated using density gradient centrifugation and, after freezing, were thawed, resuspended to 2 × 106 cells/mL in complete RPMI media, and rested overnight at 37°C. The following morning, PBMCs were adjusted to 1 × 106 cells/mL in complete RPMI and stimulated for 6 hours with staphylococcus enterotoxin-B (SEB, 1 μg/mL final concentration; Sigma, St. Louis, MO) or PMA + A23187 (both positive controls), DMSO alone (negative control), or SIV antigenic peptides (5 μL of each peptide mix with each peptide at a final concentration of 2 μg/mL) in the presence of brefeldin-A (Sigma). In a subset of experiments (18 SIV-infected SMs), anti-CD107a-PE (clone H4A3; BD-Pharmingen) was added to the cells at a pretitrated volume. Costimulation, when used, was provided using anti-CD28 and anti-CD49d antibodies (1 μg/mL final concentration; BD-Biosciences, San Jose, CA). Cells were then incubated for 6 hours at 37°C. Following incubation, cells were washed, surface stained for CD3 and CD8, fixed, and permeabilized (CytoFix/CytoPerm; BD-Pharmingen), washed twice in the supplied buffer, and then stained intracellularly for IFN-γ, TNF-α, and IL-2. Following staining, cells were washed a final time and fixed in PBS containing 1% paraformaldehyde. The fixed cells were stored at 4°C until time of fluorescence-activated cell sorter (FACS) analysis.
Characterization of viral subtypes and generation of SIVsmm-Gag subtypes-1 and -2 consensus sequences
PCR. SIVsmm RNA was extracted from 280 μL plasma using the QIAamp Viral RNA Mini Kit (QIAGEN, Valencia, CA). Nested PCR was performed to obtain amplified fragments from the gag and env regions. A 793-bp gag fragment was obtained by a nested PCR protocol using gagA/gagB and gagC/gagF primers, as described.32 Alternatively, primers GF1/GR1 and GF2A/GR312 were used in a nested PCR to generate a 909-bp fragment in the gag region. These 2 fragments are completely overlapped. Nested primers were used for sequencing. A 438-bp fragment in the gp36 env region was obtained using a previously described nested PCR protocol, using primers EF4/ER1 and EF5A/ER2A.33
Phylogenetic analysis. The gag and env nucleotide sequence alignments were obtained from the Los Alamos National Laboratory HIV Sequence Database (http://hiv-web.lanl.gov). Newly derived SIVsmm sequences were aligned using the CLUSTALW profile alignment option.34 The resulting alignments were adjusted manually where necessary. Regions of ambiguous alignment and all gap-containing sites were excluded. Phylogenetic trees were inferred from the nucleotide sequence alignments by the neighbor-joining method35 using the HKY85 model of nucleotide substitution36 implemented using PAUP*.37 The reliability of branching order was assessed by performing 1000 bootstrap replicates, again using neighbor-joining and the HKY85 model. Phylogenetic trees were also inferred by maximum likelihood using PAUP* with models inferred from the alignment using Modeltest.38 The neighbor-joining tree topology was used as the starting tree in a heuristic search using TBR branch swapping. Generation of consensus amino acid sequences for SIVsmm-Gag subtypes-1 and -2 was performed using Modeltest, and alignment with SIVmac239-Gag was conducted to determine any amino acid mismatch in positions 33 to 269. Two sets of 15-mer peptides overlapping by 11 were then designed for SIVsmm-Gag subtypes-1 and -2, and all peptides showing sequence mismatches with SIVmac239 were custom synthesized (SynPep, Dublin, CA), pooled (one pool each for SIVsmm-Gag subtypes-1 and -2), and used as described under “Intracellular cytokine staining and T-cell degranulation in response to SIV peptides” for the SIVmac239 peptides.
Statistical analysis
Correlation analyses within the same group of animals for 2 different parameters were performed using the Spearman rank correlation test and significance was determined as P below .05. The Mann-Whitney U test (2-tailed, α= .05) was used to analyze the difference between the median percentage of Ki67+ cells in SIV-infected and -uninfected SMs. To compare the medians of CD4 count or viral load when grouped by viral subtype or number of responses, a one-way nonparametric analysis of variance (ANOVA, Kruskal-Wallis) was performed followed by a Dunn multiple comparison procedure. Statistics were performed using GraphPad-Prism 4.0b (San Diego, CA) for Macintosh.
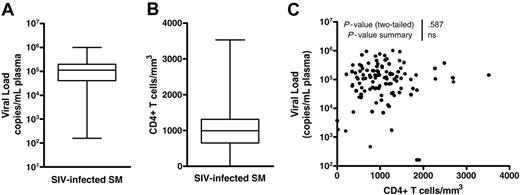
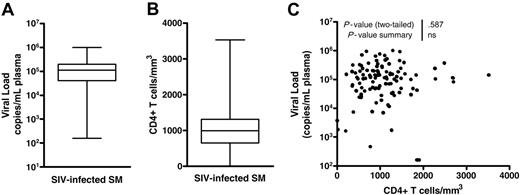
Viral load and CD4+ T-cell count in naturally SIV-infected SMs. (A) Viral load (SIV RNA copies/mL plasma) in 110 SIV-infected SMs included in this study. (B) CD4+ T-cell counts (cells/mm3) in the same 110 SIV-infected SMs. (C) Lack of correlation between CD4+ T-cell counts (cells/mm3) and viral load (SIV RNA copies/mL plasma) in the same cohort of 110 SIV-infected SMs. For panel C, P = ns indicates that the P value of the correlation coefficient was more than .05 (Spearman rank correlation test).
Viral load and CD4+ T-cell count in naturally SIV-infected SMs. (A) Viral load (SIV RNA copies/mL plasma) in 110 SIV-infected SMs included in this study. (B) CD4+ T-cell counts (cells/mm3) in the same 110 SIV-infected SMs. (C) Lack of correlation between CD4+ T-cell counts (cells/mm3) and viral load (SIV RNA copies/mL plasma) in the same cohort of 110 SIV-infected SMs. For panel C, P = ns indicates that the P value of the correlation coefficient was more than .05 (Spearman rank correlation test).
Results
Viral load and CD4+ T-cell counts in SIV-infected SMs
To confirm previous observations made by our group and others,7-9 we first measured viral load and CD4+ T-cell counts in 110 naturally SIV-infected SMs and found high levels of viral replication (average of 171 000 copies/mL, Figure 1A) and generally preserved CD4+ T-cell counts (average of 1076/mm3, Figure 1B). Consistent with our previous observation in a smaller group of animals,9 we found no association between CD4+ T-cell count and viral load (Figure 1C). In all, these results confirm the typical virologic and immunologic features of natural SIV infection of SMs, and illustrate that the main difference between HIV infection of humans and SIV infection of SMs is the better preservation of CD4+ T-cell counts in SMs rather than a lower level of viral replication.
Magnitude and breadth of SIV-specific T-cell responses in SIV-infected SMs
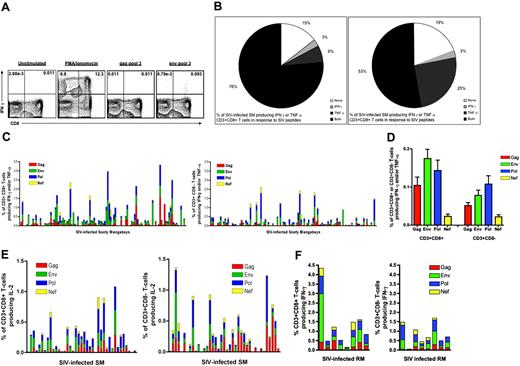
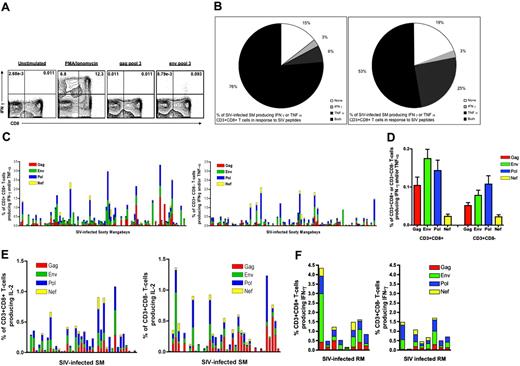
Our previous studies9,39 indicate that both natural and experimental SIVsmm infections of SMs are characterized by limited T-cell activation. However, no data were generated regarding the level of SIV-specific cellular immune responses in these animals, and thus no conclusions could be drawn on the role, either protective or harmful, of these responses in determining the outcome of infection. To address these issues, we first measured both the magnitude and breadth of SIV-specific, CD3+CD8+ or CD3+CD8- (ie, predominantly CD4+) T-cell-mediated responses in the 110 naturally SIV-infected SMs of the Yerkes colony. To the best of our knowledge, this study represents the first systematic analysis of SIV-specific cellular immune responses in a natural host species for SIV infection. SIV-specific responses were measured as the fraction of either CD3+CD8+ or CD3+CD8- T cells producing either IFN-γ or TNF-α in response to peptides spanning the entire sequence of SIVmac239 gag, pol, env, and nef.Figure 2A shows an example of an IFN-γ response to Env pool no. 3 by CD3+CD8+ T cells. SIV-specific CD3+CD8+ T-cell-mediated responses (defined as production of either IFN-γ or TNF-α) were detected in 94 (85.5%) of 110 animals and CD3+CD8- T-cell-mediated responses in 89 (80.9%) of 110 animals (Figure 2B). Figure 2C shows the magnitude of the total SIV-specific responses mediated by CD3+CD8+ or CD3+CD8- T cells. The mean of the total SIV-specific CD3+CD8+ T-cell responses was 0.45% ± 0.060%, and the mean of the total CD3+CD8- responses was 0.26% ± 0.039% (Figure 2C). When the same assay was performed in 20 SIV-uninfected SMs, SIV-specific responses above background were detected at a very low level (ie, total response < 0.05%) in just 2 animals, perhaps indicating prior exposure to SIV-infected animals (data not shown). It is important to note that the observed levels of SIV-specific T-cell responses in naturally SIV-infected SMs are markedly lower than those reported, using the same technique, in HIV-infected individuals.40,41 Figure 2D shows the relative contribution of the 4 individual SIV antigens used in these experiments. The hierarchy of immunogenicity for CD3+CD8+ T-cell responses was Env(39.1%) > Pol (32.1%) > Gag (23.4%) > Nef (5.4%), while for CD3+CD8- T-cell responses the hierarchy was Pol (41.3%) > Env (30.1%) > Gag (20.0%) > Nef (8.6%). It is interesting to note that this antigen immunogenicity profile is different from that described in HIV-infected patients where Gag-specific cellular immune responses consistently predominate.40-43 The reasons for this difference are unclear, but are unlikely to involve lack of recognition of the peptides used in this study, as the SIV antigen most commonly recognized by CD3+CD8+ T cells (ie, Env) has the greatest sequence variability in naturally SIV-infected SMs (S.I.S. and S. Garg, unpublished observations, June 2005).
SIV-specific T-cell responses in naturally SIV-infected SMs. The responses were measured by intracellular cytokine staining for IFN-γ, TNF-α, and IL-2 in response to peptide pools encompassing the entire sequence of gag, pol, env, and nef genes of SIVmac239. A positive T-cell response was defined as cytokine production greater than unstimulated negative control by at least 0.01%. (A) Representative plot of an IFN-γ response to Gag pool no. 3 and Env pool no. 3 (right) along with the unstimulated negative control (left) and positive control (PMA and ionomycin: middle). (B) Distribution of naturally SIV-infected SMs based on the presence of above-background responses to SIV by CD3+CD8+ (right) and CD3+CD8- (left) T cells. Animals were divided as producing no cytokine, IFN-γ only, TNF-α only, or both cytokines in response to any pool of SIVmac239 peptides. (C) Magnitude of SIV-specific T-cell responses defined as percent of CD3+CD8+ (left) or CD3+CD8- (right) T cells producing either IFN-γ or TNF-α in response to SIVmac239 peptide stimulation. Each bar represents an individual animal. The contribution of each of the tested antigens to the total SIV-specific T-cell response is shown. (D) Average magnitude of the responses to the 4 tested SIV antigens by CD3+CD8+ (left) and CD3+CD8- (right) T cells. (E) Percentage of CD3+CD8+ (left) or CD3+CD8- (right) T cells producing IL-2 in response to SIVmac239 peptide stimulation in 39 SIV-infected SMs. The contribution of each of the tested antigens to the total SIV-specific T-cell response is shown. (F) Magnitude of SIV-specific T-cell responses in 8 experimentally SIVsm-infected rhesus macaques (RMs) defined as percent of CD3+CD8+ (left) or CD3+CD8- (right) T cells producing IFN-γ or TNF in response to SIV stimulation. The total SIV-specific 6T-cell response is broken down as response to any of the 4 tested SIV antigens.
SIV-specific T-cell responses in naturally SIV-infected SMs. The responses were measured by intracellular cytokine staining for IFN-γ, TNF-α, and IL-2 in response to peptide pools encompassing the entire sequence of gag, pol, env, and nef genes of SIVmac239. A positive T-cell response was defined as cytokine production greater than unstimulated negative control by at least 0.01%. (A) Representative plot of an IFN-γ response to Gag pool no. 3 and Env pool no. 3 (right) along with the unstimulated negative control (left) and positive control (PMA and ionomycin: middle). (B) Distribution of naturally SIV-infected SMs based on the presence of above-background responses to SIV by CD3+CD8+ (right) and CD3+CD8- (left) T cells. Animals were divided as producing no cytokine, IFN-γ only, TNF-α only, or both cytokines in response to any pool of SIVmac239 peptides. (C) Magnitude of SIV-specific T-cell responses defined as percent of CD3+CD8+ (left) or CD3+CD8- (right) T cells producing either IFN-γ or TNF-α in response to SIVmac239 peptide stimulation. Each bar represents an individual animal. The contribution of each of the tested antigens to the total SIV-specific T-cell response is shown. (D) Average magnitude of the responses to the 4 tested SIV antigens by CD3+CD8+ (left) and CD3+CD8- (right) T cells. (E) Percentage of CD3+CD8+ (left) or CD3+CD8- (right) T cells producing IL-2 in response to SIVmac239 peptide stimulation in 39 SIV-infected SMs. The contribution of each of the tested antigens to the total SIV-specific T-cell response is shown. (F) Magnitude of SIV-specific T-cell responses in 8 experimentally SIVsm-infected rhesus macaques (RMs) defined as percent of CD3+CD8+ (left) or CD3+CD8- (right) T cells producing IFN-γ or TNF in response to SIV stimulation. The total SIV-specific 6T-cell response is broken down as response to any of the 4 tested SIV antigens.
To then determine whether natural SIV infection of SMs is associated with SIV-specific IL-2 production (in the absence of IFN-γ or TNF-α production), potentially due to the presence of SIV-specific T cells with functional features of “tcentral memory” T cells (TCMs),44 we measured IL-2 production in response to SIVmac239 peptides in 39 naturally SIV-infected SMs. As shown in Figure 2E, we found that only a very small percentage of CD4+ and CD8+ T cells from SIV-infected SMs produce IL-2 in response to SIV peptides, thus ruling out the possibility that these animals may manifest strong SIV-specific TCM-like responses that result in selective production of IL-2.
To further explore the possibility that the nonpathogenic nature of natural SIVsm infection of SMs is related to the presence of strong SIV-specific T-cell responses, we compared the responses as described above to those observed in 8 SIVsmm-infected rhesus macaques (RMs) using the same ICS assay. As shown in Figure 2F, the level of SIV-specific CD4+ and CD8+ T-cell-mediated responses in SIVsmm-infected RMs, measured as production of either IFN-γ or TNF, was similar to that observed in SMs. This set of data confirms that the level of SIV-specific T-cell responses in naturally SIV-infected SMs is not higher than that observed in pathogenic HIV/SIV infections, thus supporting the hypothesis that the absence of disease in naturally SIV-infected SMs is unlikely to be related to the presence of exceptionally strong T-cell responses to the virus.
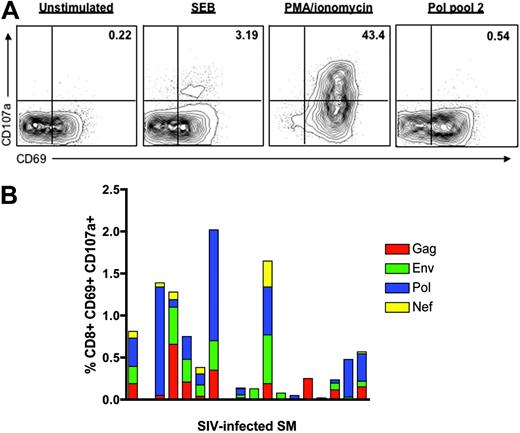
CD8+T-cell degranulation in response to SIV peptides in naturally SIV-infected SMs. In all experiments, degranulation was measured as the percentage of CD3+CD8+ T cells coexpressing CD69 and CD107a. (A) Representative plot of a positive response to SIV-Pol pool no. 2 (right) along with the unstimulated negative control (left) and 2 positive controls (SEB and PMA + ionomycin: middle). (B) Percentage of CD8+ T cells that degranulate in response to SIV peptide stimulation in 18 naturally SIV-infected SMs. Each bar represents an individual animal. The contribution of each of the tested antigens to the total SIV-specific T-cell response is shown.
CD8+T-cell degranulation in response to SIV peptides in naturally SIV-infected SMs. In all experiments, degranulation was measured as the percentage of CD3+CD8+ T cells coexpressing CD69 and CD107a. (A) Representative plot of a positive response to SIV-Pol pool no. 2 (right) along with the unstimulated negative control (left) and 2 positive controls (SEB and PMA + ionomycin: middle). (B) Percentage of CD8+ T cells that degranulate in response to SIV peptide stimulation in 18 naturally SIV-infected SMs. Each bar represents an individual animal. The contribution of each of the tested antigens to the total SIV-specific T-cell response is shown.
Finally, as we were concerned that using a single assay (ie, ICS) to detect SIV-specific T-cell responses in SMs may have led us to an underestimation of these responses, we measured SIV-specific T-cell responses in 18 SIV-infected SMs using the recently described T-cell degranulation assay based on staining for the CD107/LAMP degranulation marker.45 As shown in Figure 3, the level of CD8+ T-cell degranulation in response to SIVmac239 peptide stimulation was of limited magnitude (mean, 0.57%), and in fact was comparable with the level of IFN-γ and/or TNF-α in response to the same stimuli, thus further confirming the presence of relatively low levels of SIV-specific T-cell responses during natural SIV infection of SMs.
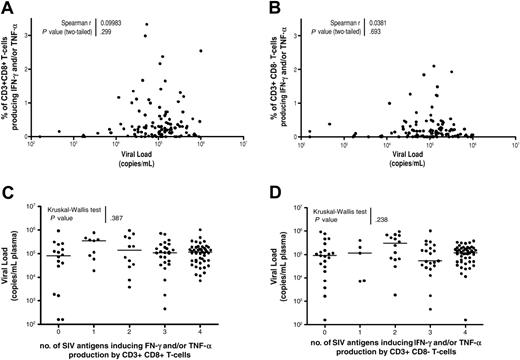
In SIV-infected sooty mangabeys, the level of viral replication does not correlate with the magnitude or the breadth of SIV-specific T-cell responses
To determine whether SIV-specific T-cell responses play a significant role in determining the set-point level of viral replication in naturally SIV-infected SMs, we sought to correlate the magnitude or breadth of these cellular immune responses with the level of plasma viremia. As shown in Figure 4A-B, no significant correlation was found between the magnitude of SIV-specific CD3+CD8+ or CD3+CD8- T-cell-mediated responses and viral load. In addition, no significant correlation was found between viral load and the magnitude of CD3+CD8+ or CD3+CD8- T-cell responses to individual SIV antigens (Gag, Pol, Env, or Nef; data not shown). To then investigate a potential correlation between breadth of SIV-specific T-cell responses and the level of viral replication, we divided the SIV-infected SMs into 5 groups according to the detection of CD3+CD8+ or CD3+CD8- responses to 4, 3, 2, 1, or no SIV antigens. As shown in Figure 4C-D, no significant differences in viral load were found between these subsets of animals, demonstrating that breadth of T-cell responses does not correlate with viral load in naturally SIV-infected SMs. In all, these findings indicate that in naturally SIV-infected SMs there is no relationship between set-point viremia and magnitude or breadth of SIV-specific T-cell responses.
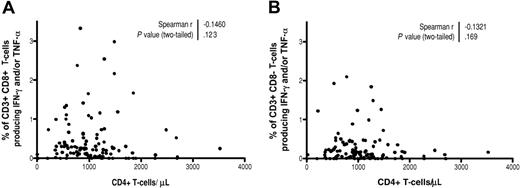
In SIV-infected sooty mangabeys, CD4+ T-cell counts do not correlate with the magnitude or the breadth of SIV-specific T-cell responses
We next sought to determine whether, in naturally SIV-infected SMs, there is a relationship between SIV-specific T-cell responses and CD4+ T-cell count. In fact, as shown in Figure 5A-B, no significant correlation was found between the magnitude of either SIV-specific CD3+CD8+ or CD3+CD8- T-cell-mediated responses and CD4+ T-cell counts. In addition, the magnitude of CD3+CD8+ or CD3+CD8- T-cell responses to individual SIV antigens also did not correlate with CD4+ T-cell count (data not shown). Finally, no significant differences in CD4+ T-cell counts were found between the subsets of animals showing greater or lesser breadth of CD3+CD8+ or CD3+CD8- T-cell responses to SIV (data not shown).
In all, these results indicate that in naturally SIV-infected SMs the preservation of normal CD4+ T-cell counts is not related to the presence of a strong and broadly reactive T-cell response to SIV antigens. In addition, these results indicate that there is no trend toward higher CD4+ T-cell counts in the animals with the lowest SIV-specific cellular immune responses, demonstrating that suppression of these responses is not a requirement to maintain CD4+ T-cell homeostasis in naturally SIV-infected SMs.
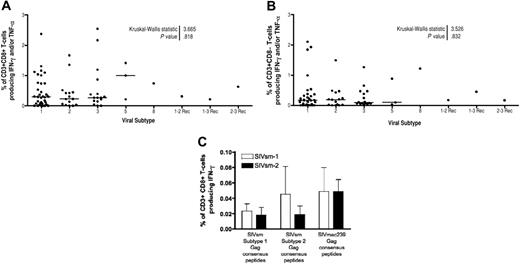
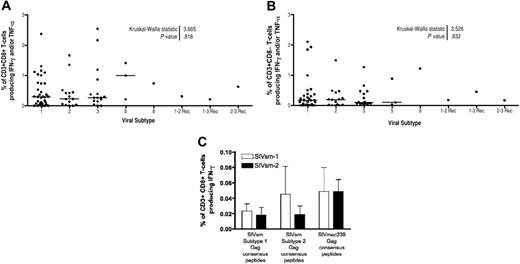
Magnitude and breadth of T-cell responses to SIV antigens in SMs is not related to infection with specific SIVsmm subtypes
In the experiments described under “Magnitude and breadth of SIV-specific T-cell responses in SIV-infected SMs,” the antigenic stimulus was provided by peptides derived from SIVmac239. Given the high genetic variability of SIVsmm in naturally SIV-infected SMs,12,32,46 we were concerned that lack of recognition of SIVmac239 peptides by T cells raised in response to infection with heterologous strains of SIVsmm may have resulted in an underestimation of the total SIV-specific responses. To test this possibility, we first compared the cellular immune responses found in SIV-infected SMs harboring different SIVsmm virus subtypes.47 Of 84 animals that were subtyped, we identified 5 of the known SIVsmm subtypes, with a predominance of subtypes-1, -2, and -3, and 3 recombinant viruses that were found in one animal each. As shown in Figure 6A-B, we did not find a significant difference in the magnitude of the CD3+CD8+ or CD3+CD8- T-cell responses in animals infected with different SIVsmm subtypes. Similarly, we did not find any differences between groups of animals infected with different SIVsmm subtypes in terms of the breadth of their SIV-specific CD3+CD8+ or CD3+CD8- T-cell-mediated responses (data not shown).
SMs infected with SIVsmm subtype-1 or -2 do not show increased levels of SIV-Gag-specific T-cell responses when subtype-1 or -2 consensus Gag-derived peptides are used as stimuli
To more directly assess whether using SIVmac239 peptides might have led us to underestimate the SIV-specific T-cell responses in SIV-infected SMs, we sought to repeat our study using a stimulus that more closely resembles autologous virus. As it is virtually impossible to generate peptide pools derived from the autologous virus isolated from each tested animal, we addressed the issue of variability of SIVsmm by using peptides derived from consensus amino acid sequences of Gag found in SIVsmm subtypes-1 and -2. To this end, we first sequenced a large portion (approximately 900 bp) of the SIVsmm-gag gene in all animals infected with SIVsmm subtypes-1 and -2 (the 2 most common subtypes) and generated a consensus amino acid sequence for both subtypes. We then designed and synthesized a set of 15-mer peptides that includes the discrepant regions between SIVmac239-Gag and the SIVsmm subtype-1 and subtype-2 Gag “consensus” sequences. A total of 56 new peptides were synthesized, pooled as SIVsmm-Gag-consensus-1 and SIVsmm-Gag-consensus-2, and used to measure Gag-specific T-cell responses in 9 SMs infected with SIVsmm subtype-1 and 10 SMs infected with SIVsmm subtype-2 (to compare these responses with those obtained using the corresponding set of SIVmac239-Gag peptides). As shown in Figure 6C, the use of these consensus SIVsmm-Gag peptide pools as stimuli did not result in a significant increase in the level of detectable Gag-specific T-cell responses, suggesting that a major underestimation of SIV-specific cellular immune responses in naturally SIV-infected SMs due to the use of SIVmac239 peptides is highly unlikely.
Lack of correlation between magnitude or breadth of SIV-specific T-cell responses and viral load in naturally SIV-infected SMs. (A-B) The percent of SIV-specific CD3+CD8+ T cells (A) or CD3+CD8- T cells (B) was plotted along with SIV viremia (copies/mL plasma). Magnitude of the SIV-specific response is represented by the percent of CD3+CD8+ or CD3+CD8- T cells producing either IFN-γ or TNF-α in response to SIVmac239 peptide pools. P = ns indicates that the P value of the correlation coefficient is more than .05 (Spearman rank correlation test). (C-D) Comparison of viral load (copies/mL plasma) in naturally SIV-infected SMs grouped by the presence of detectable CD3+CD8+ (C) or CD3+CD8- (D) T-cell-mediated responses to 4, 3, 2, 1, or no SIVmac239 antigens. One-way nonparametric ANOVA (Kruskal-Wallis) followed by Dunn multiple comparison test found no significant differences between the groups. Horizontal lines indicate mean values.
Lack of correlation between magnitude or breadth of SIV-specific T-cell responses and viral load in naturally SIV-infected SMs. (A-B) The percent of SIV-specific CD3+CD8+ T cells (A) or CD3+CD8- T cells (B) was plotted along with SIV viremia (copies/mL plasma). Magnitude of the SIV-specific response is represented by the percent of CD3+CD8+ or CD3+CD8- T cells producing either IFN-γ or TNF-α in response to SIVmac239 peptide pools. P = ns indicates that the P value of the correlation coefficient is more than .05 (Spearman rank correlation test). (C-D) Comparison of viral load (copies/mL plasma) in naturally SIV-infected SMs grouped by the presence of detectable CD3+CD8+ (C) or CD3+CD8- (D) T-cell-mediated responses to 4, 3, 2, 1, or no SIVmac239 antigens. One-way nonparametric ANOVA (Kruskal-Wallis) followed by Dunn multiple comparison test found no significant differences between the groups. Horizontal lines indicate mean values.
Lack of correlation between magnitude or breadth of SIV-specific T-cell responses and CD4+ T-cell counts in naturally SIV-infected SMs. (A-B) The percent of SIV-specific CD3+CD8+ T cells (A) or CD3+CD8- T cells (B) was plotted along with CD4+ T-cell counts (cells/mm3). Magnitude of the SIV-specific response is represented by the percent of CD3+CD8+ or CD3+CD8- T cells producing either IFN-γ or TNF-α in response to SIVmac239 peptide pools. P = ns indicates that the P value of the correlation coefficient is more than .05 (Spearman rank correlation test).
Lack of correlation between magnitude or breadth of SIV-specific T-cell responses and CD4+ T-cell counts in naturally SIV-infected SMs. (A-B) The percent of SIV-specific CD3+CD8+ T cells (A) or CD3+CD8- T cells (B) was plotted along with CD4+ T-cell counts (cells/mm3). Magnitude of the SIV-specific response is represented by the percent of CD3+CD8+ or CD3+CD8- T cells producing either IFN-γ or TNF-α in response to SIVmac239 peptide pools. P = ns indicates that the P value of the correlation coefficient is more than .05 (Spearman rank correlation test).
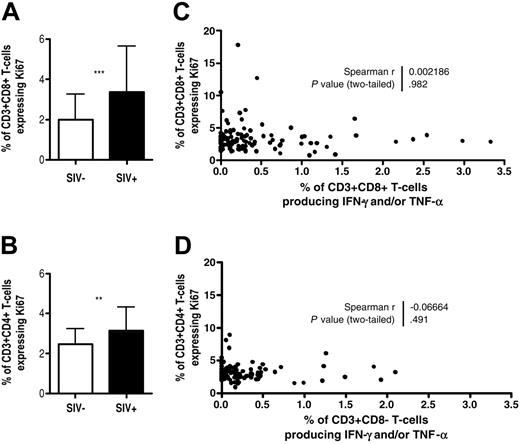
In SIV-infected SMs, the magnitude of SIV-specific T-cell responses does not correlate with the levels of T-cell activation and proliferation
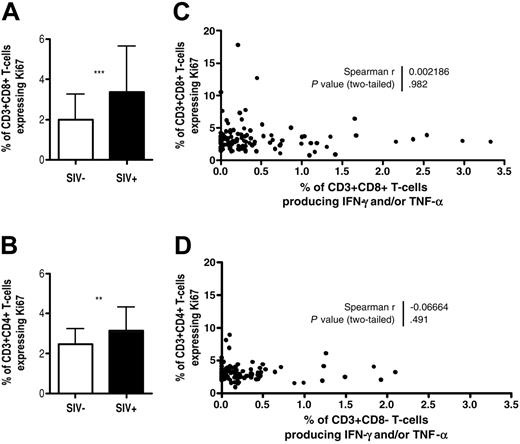
During natural as well as experimental SIVsmm infection of SMs, the levels of T-cell activation and proliferation are significantly lower than those reported for HIV-infected individuals.9,39 In this context, the observation of low levels of SIV-specific cellular responses in naturally SIV-infected SMs may reflect this lack of immune activation. To investigate this possibility, we first measured the fraction of CD4+Ki67+ and CD8+Ki67+ T cells in the peripheral blood of 110 SIV-infected SMs as well as 30 SIV-uninfected animals. As shown in Figure 7A-B, SIV-infected animals show a minor, albeit significant, increase in the fraction of Ki67+ T cells compared with uninfected animals. Of interest, no correlation was found between the fraction of CD4+Ki67+ or CD8+Ki67+ T cells and the magnitude (Figure 7C-D) or breadth (data not shown) of SIV-specific responses mediated by CD3+CD8- and CD3+CD8+ T cells, respectively. Similarly, no correlation was found between the magnitude of SIV-specific responses and the presence of markers of activation and/or expansion of effector T cells (HLA-DR, CD25, CD69, CD95, loss of CD28, loss of CCR7, loss of CD127) on CD4+ or CD8+ T cells (data not shown). Taken as a whole, these data indicate that SIV-specific T-cell responses are not the main contributor to the prevailing levels of T-cell activation and proliferation in naturally SIV-infected SMs.
Similar magnitude or breadth of SIV-specific T-cell responses in naturally SIV-infected SMs grouped by infecting SIVsmm viral subtypes. A total of 84 animals were included in this study. (A-B) Magnitude of CD3+CD8+ (A) and CD3+CD8- (B) T-cell responses in SIV-infected SMs grouped by infecting viral subtype. One-way nonparametric ANOVA (Kruskal-Wallis) of all groups followed by Dunn multiple comparison test found no significant differences between the groups. Horizontal lines indicate mean values. (C) Percentage of CD3+CD8+ T cells producing IFN-γ in response to pools of SIVsmm-Gag subtype-1 or -2 “consensus” peptides in 9 SIVsmm subtype-1-infected and 10 SIVsmm subtype-2-infected SMs. Each bar represents an individual animal. No significant differences were observed between groups using a 2-way ANOVA. Error bars indicate standard deviation.
Similar magnitude or breadth of SIV-specific T-cell responses in naturally SIV-infected SMs grouped by infecting SIVsmm viral subtypes. A total of 84 animals were included in this study. (A-B) Magnitude of CD3+CD8+ (A) and CD3+CD8- (B) T-cell responses in SIV-infected SMs grouped by infecting viral subtype. One-way nonparametric ANOVA (Kruskal-Wallis) of all groups followed by Dunn multiple comparison test found no significant differences between the groups. Horizontal lines indicate mean values. (C) Percentage of CD3+CD8+ T cells producing IFN-γ in response to pools of SIVsmm-Gag subtype-1 or -2 “consensus” peptides in 9 SIVsmm subtype-1-infected and 10 SIVsmm subtype-2-infected SMs. Each bar represents an individual animal. No significant differences were observed between groups using a 2-way ANOVA. Error bars indicate standard deviation.
Lack of correlation between magnitude of SIV-specific T-cell responses and the level of T-cell proliferation measured as fraction of Ki67+ T cells. (A-B) Comparison of the percent of Ki67+ cells in the CD3+CD8+ (A) or CD3+CD4+ (B) T-cell subsets in SIV-infected and uninfected animals (**P < .01, ***P < .001 as determined by the Mann-Whitney U test.) (C-D) Lack of correlation between the percent of CD3+CD8+ (C) and CD3+CD4+ (D) T cells expressing the Ki67 proliferation marker and the magnitude of SIV-specific responses mediated by CD3+CD8+ (C) and CD3+CD8- (D) T cells. P = ns indicates that the P value of the correlation coefficient is more than .05 (Spearman rank). Error bars in panels A and B indicate standard deviation.
Lack of correlation between magnitude of SIV-specific T-cell responses and the level of T-cell proliferation measured as fraction of Ki67+ T cells. (A-B) Comparison of the percent of Ki67+ cells in the CD3+CD8+ (A) or CD3+CD4+ (B) T-cell subsets in SIV-infected and uninfected animals (**P < .01, ***P < .001 as determined by the Mann-Whitney U test.) (C-D) Lack of correlation between the percent of CD3+CD8+ (C) and CD3+CD4+ (D) T cells expressing the Ki67 proliferation marker and the magnitude of SIV-specific responses mediated by CD3+CD8+ (C) and CD3+CD8- (D) T cells. P = ns indicates that the P value of the correlation coefficient is more than .05 (Spearman rank). Error bars in panels A and B indicate standard deviation.
Discussion
Natural SIV infection of SMs is characterized by the absence of AIDS and, in the majority of animals, normal CD4+ T-cell counts, despite levels of virus replication similar to HIV-infected humans.7-9 The mechanisms underlying this lack of disease progression are still poorly understood, although our previous work has shown low levels of immune activation and T-cell apoptosis in naturally SIV-infected SMs.9 As chronic immune activation is considered to be a key contributor to the loss of CD4+ T-cell homeostasis during HIV infection,16-18,48 we proposed that the attenuated T-cell activation of naturally SIV-infected SMs plays an important role in maintaining the disease-free status of these animals.9 However, the relationship between T-cell activation and HIV/SIV disease progression is very complex, as the level of “bulk” T-cell activation reflects, at least in part, the level of virus-specific T-cell responses49 that are thought to protect from disease progression during pathogenic HIV and SIV infections.19-31,50
To better understand the complex nature of the interaction between host antiviral cellular immune responses and disease progression during retroviral infections, we undertook a systematic analysis of the SIV-specific T-cell responses in naturally SIV-infected SMs. In essence, we wanted to investigate whether the nonprogressive nature of natural SIV infection of SMs is related to the presence of highly effective SIV-specific cellular immune responses or, alternatively, to the suppression of these SIV-specific T-cell responses with a resultant state of limited immune activation. We sought to answer these questions by (1) measuring the magnitude and breadth of the SIV-specific T-cell responses in both the CD3+CD8+ and CD3+CD8- T-cell populations; (2) investigating the presence of a relationship between the magnitude or breadth of these T-cell responses and the markers of disease progression (ie, viral load and CD4+ T-cell count); and (3) investigating the relationship between the level of SIV-specific T-cell responses and the level of “bulk” T-cell activation.
In synthesis, the data presented here show that SIV-infected SMs mount a detectable, albeit of small magnitude, T-cell response to SIV antigens, indicating that complete suppression of virus-specific cellular responses (ie, immunologic tolerance and/or ignorance) is not an absolute requirement for the establishment of the low levels of T-cell activation that characterize these animals. Thus, naturally SIV-infected SMs do not appear to be tolerant to SIV, but rather should be considered “low responders.” It is important to note that these low cellular immune responses to SIV during natural SIV infection of SMs are consistent with the presence of high viral loads and the absence of generalized immune activation.
Of importance, in naturally SIV-infected SMs the magnitude and breadth of SIV-specific T-cell responses (measured both as production of cytokines or degranulation in response to SIV peptide pools) are clearly lower than what has been reported for HIV-infected humans40 and are of similar magnitude to the SIV-specific T-cell responses that we have observed in SIVsmm-infected RMs. The comparison between SIV-specific cellular responses in pathogenic versus nonpathogenic primate lentiviral infections clearly indicates that it is highly unlikely that an exceptionally strong cellular immune response is responsible for the lack of disease progression during natural, nonpathogenic SIV infection of SMs. In addition, the level of SIV-specific cellular responses in SIV-infected SMs does not correlate with either control of viral replication or the number of circulating CD4+ T cells. This finding is consistent with the known observation that, in HIV-infected individuals, there is no correlation between the level of HIV-specific T-cell responses and viral load40,42 and indicates that, in both HIV-infected humans and SIV-infected SMs, the level of set-point viremia is unlikely to be dictated solely by the prevailing level of T-cell responses to the virus.
In SIV-infected rhesus macaques (RMs), the in vivo role of SIV-specific CD8+ T-cell responses has been assessed by experimentally depleting CD8+ T cells. In these CD8+ T-cell-depleted SIV-infected RMs, a marked increase in viral replication was seen.28-31,50,51 Similar experiments were conducted by our group in 6 SIV-infected SMs with only modest changes in viral replication (ie, usually < 1 log) seen following CD8+ T-cell depletion (A. Barry, G.S., J.T. Safrit, B.S., N. Kozyr, H.M.M., S.I.S., M.B.F., “Depletion of CD8+ T cells in sooty mangabeys naturally infected with SIV reveals limited role for immune control of virus replication in a natural host species,” manuscript in preparation), consistent with the hypothesis of a limited in vivo role of CD8+ T-cell-mediated responses in determining viral replication in SIV-infected SMs.
Given the genetic variability of SIVsmm,47 we were concerned that SIVmac239-based peptides may not detect all the SIV-specific responses present in naturally infected SMs. Indeed, a certain level of underestimation of the total SIV-specific cellular responses is possible unless endogenous viral sequences are used for peptide synthesis. It should be noted, however, that a similar caveat applies to the vast majority of studies that have been performed to measure the level of HIV-specific T-cell responses in humans.40-42 Two indirect but important reasons suggest that a major underestimation of SIV-specific T-cell responses due to SIV sequence variability between animals is unlikely: first, there was no significant difference in terms of magnitude and/or breadth of SIV-specific cellular immune responses in SMs infected with different viral subtypes; second, the SIV antigen (ie, Env) most commonly recognized is also the most variable in sequence. Despite this evidence, we still felt that it was necessary to directly address the issue of SIVsmm variability, and thus decided to repeat our measurement of SIV-specific T-cell responses in a subset of animals using “autologous consensus” SIVsmm peptides as stimuli. We first generated consensus amino acid sequences for SIVsmm-Gag subtypes-1 and -2 (the most common subtypes), and then synthesized peptides that include all the sequence changes between SIVmac239-Gag and the SIVsmm subtype-1 and subtype-2 consensus Gag. Of importance, the use of these consensus SIVsmm-Gag peptide pools as stimuli did not result in a significant increase in the detection of Gag-specific T-cell responses in SMs, indicating that using SIVmac239-derived peptides does not significantly underestimate the level of these responses (at least those targeting the Gag antigen).
Perhaps the most interesting implication of this study concerns the nature of the evolutionary coadaptation of SIV and its natural hosts that has occurred over the many thousands of years in which these animals have been infected with SIV. HIV infection of humans (a species that only recently became a host for a primate lentiviral infection) is associated with strong, but ultimately ineffective, antiviral cellular immune responses that may eventually contribute to the chronic generalized immune activation that is related to the progression to AIDS.16-18,48 In contrast, our work clearly indicates that SMs, and perhaps other natural hosts for SIV, have adapted to the selective pressure of SIV infection and have reached a disease-free state in a way that does not involve the generation of a strong and broadly reactive antiviral cellular immune response. Instead, a favorable evolutionary outcome appears to have resulted from a general attenuation of both the SIV-specific T-cell response and the overall level of immune activation. The notion of a protective effect of limited immune activation during SIV infection of natural host monkey species is consistent with the recent and very intriguing finding of limited inflammatory responses during acute SIVagm infection of African green monkeys.52 It is tempting to speculate that this host-virus adaptation that results in low levels of SIV-specific cellular immune responses reflects the extreme elusiveness of SIV as a target for protective immunity. In this regard, our study emphasizes the tremendous challenge of artificially inducing, with an AIDS vaccine, a type of protective immunity that has not been selected for in many thousands of years of evolutionary pressure posed by this retrovirus on the primate immune system.
In summary, the present study strongly supports the hypothesis that an attenuated SIV-specific T-cell response and lack of generalized immune activation are essential for the AIDS resistance of naturally SIV-infected SMs. The exact molecular and cellular mechanisms underlying the striking difference in the level of immune activation between HIV-infected humans and SIV-infected SMs remain elusive and will be the subject of intense future investigation. It is conceivable that the mechanisms of immune attenuation in the presence of high antigenic load may act at several levels, including the innate immune response to SIV, the interface between innate and adaptive antiviral immunity, and the intrinsic responsiveness of SIV-specific T cells. It is hoped that a complete understanding of the mechanisms responsible for the AIDSresistant phenotype of SMs will provide advances in our understanding of the pathogenesis of AIDS in humans, and eventually translate into new, immune-based therapeutic strategies that may be used in addition to standard highly active antiretroviral therapy (HAART) in HIV-infected individuals.
Prepublished online as Blood First Edition Paper, March 7, 2006; DOI 10.1182/blood-2005-12-4897.
Supported by National Institutes of Health (NIH) grants R01-AI52755 (G.S.), R01-AI049155 (S.I.S.), and P20-RR020159 (C.A.), and by the Yerkes National Primate Research Center P51 NIH-NCRR-RR00165.
R.D., P.P., and A.M. analyzed T-cell responses using intracellular cytokine staining; J.E. optimized and performed the CD107 assay; S.G. and B.S. performed the immunophenotypic analysis; B.L., S.G., and S.I.S. optimized and performed the viral load assay; H.M.M. supervised the housing and care of the animals; Y.-X.X. and C.I. optimized the assays used to measure SIV-specific T-cell responses; K.E. performed the statistical analyses; N.K., I.P., and C.A. sequenced the autologous SIVsmm virus used to generate consensus peptides; M.P., D.L.S., and M.B.F. contributed to the design, analysis, and writing of this paper; and G.S. wrote the paper, with contributions from the other authors as appropriate.
Harold M. McClure died on October 23, 2004.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
The authors wish to thank Drs Daniel Douek, Louis Picker, and Ronald Veazey for helpful discussions; Stephanie Ehnert, Dr Elizabeth Strobert, and Chris Souder for their assistance with animal studies; Dr Ann Chahroudi for critical reading of this paper; and the research staff of the Emory Center for AIDS Research (CFAR) Immunology and Virology Cores for their facilitation of this work.
This paper is dedicated to the memory of our colleague and friend Harold M. McClure (1937-2004) without whom this work would not have been possible.